The plague is a serious infectious disease that can be fatal. The trigger is the bacterium Yersinia pestis, which is transmitted from rat fleas to humans. In Europe, the disease no longer plays a role today. In some regions of Africa, Asia and South, Central and North America, however, there are always (smaller) plague outbreaks. Read how to protect yourself against infection when traveling in high-risk areas and why you should go to the doctor as soon as possible if you have a suspected plague!

Quick Overview
- What is pest? Highly contagious infectious disease transmitted by rodent fleas. Does not matter anymore in Europe today.
- History: There were two major plague pandemics in Europe that wiped out millions of lives. These disease waves laid the foundation for the understanding of diseases and infection routes of today’s medicine.
- symptoms: Depending on the shape z. High fever, chills, swollen lymph nodes, black / bluish skin coloration, bloody sputum
- Reason: The trigger is the bacterium Yersinia pestis. It is transmitted by flea bites and can also be passed on from person to person. Rarely, the infection occurs through direct contact with infected rodents. In lung plague, droplet infection is the most important transmission route. Risk factors are u. a. bad hygiene standards.
- Treatment: antibiotics
- Forecast: good at early start of therapy, otherwise the disease usually ends fatally.
Pest: Description
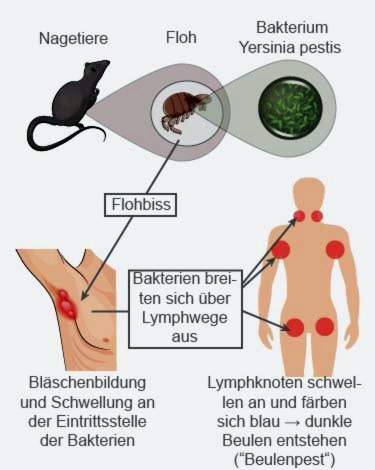
The times when the plague (“Black Death”) wiped out entire villages is fortunately over. Today, the infectious disease in Europe no longer matters. It is caused by the Bacterium Yersinia pestis, Rodents like rats and mice are the reservoir of the pathogen. About fleas, the bacterium can be transferred from the animals to humans. Rarely do people directly attack infected rodents. Diseases that, like the plague of vertebrates (such as rats), are transmissible to humans (and vice versa) are known as zoonoses.
People infected with plague can also pass on the pathogen to other people. This happens especially with the lung plague. It is transmitted via droplet infection.
Pest: Contained, but not extinguished
The danger of becoming infected with plague exists especially in areas where there are pest-infected wild rodents. This is according to Robert Koch Institute, however, only in limited endemic areas in Africa, Asia, in the tropical Central and South America as well as in the southwest of the USA. The spread of the plague is fostered when many people live together in a confined space under poor hygienic conditions.
But big epidemics and pandemics, which claimed millions of victims in the Middle Ages, no longer exist today.
Between 2010 and 2015, the World Health Organization registers 3,248 pest diseases worldwide, including 584 deaths. However, this figure is very inaccurate as more than 80% of infections occur in Africa, where not all cases are reported to the WHO. Incidentally, in Germany, there is also a reporting obligation under the Infection Protection Act (IfSG) for any suspected plague, proven diseases and deaths from plague.
In addition to cholera, smallpox and yellow fever, the plague is one of the four quarantine diseases as defined by the World Health Organization (WHO). These diseases have a particularly threatening course of the disease and are extremely contagious.
Plague: symptoms
The time span between the infection with the pest agent and the appearance of the first symptoms (incubation period) varies considerably. It is between a few hours and up to seven days.
Basically, there are three different main types of plague in humans with some different pest symptoms.
bubonic plague
The bubonic plague, too bubonic plague or Black Death called, is the most common and well-known form of the plague. It is generally transmitted only by flea bites. As a rule, the first symptoms appear two to six days after infection:
- high fever
- chills
- a headache
- general feeling of weakness
At the point where the plague bacteria have penetrated into the skin via flea bite, sometimes small bubbles form. Sometimes a mild red rash develops in later stages. The plague pathogens migrate into the adjacent lymph nodes, which swell by the infection and can be easily palpated. The swollen regions are hard and hurt at the bubonic plague. Often affected are groin, armpits and neck, where the large lymph node stations are located. In the further course, the disease spreads and also more distant lymph nodes swell.
Like a bruise, lymph node swelling turns blue within a few days, giving the typical picture of dark bumps in plague patients. Rarely do they open and empty highly infectious secretions.
When the lymph nodes bleed, complications can occur. Because then there is a risk that bacteria get into the blood or the lungs. Then a so-called postsepsis or a lung plague can result. Both forms of disease are serious and often fatal.
pneumonic
The pneumonic plague arises either as a complication of bubonic plague or as an “independent” disease after transmission of the plague pathogen via droplet infection: Diseased people Spreading when talking, coughing or sneezing tiny secretions droplets in the ambient air. These droplets contain pest bacteria and are highly contagious. When healthy people breathe in them, the bacteria enter the lungs directly and trigger the lung plague.
The first signs of pulmonary plague develop within a few hours after the plague virus reaches the lungs. First, the patient only has a fever, may have chills and / or headaches, and generally feels weak. On the second day, coughing, often with (bloody) expectoration, and chest pains are added. The patient has a fast pulse and shortness of breath. Because of the strong coughing, sufferers vomit frequently or have abdominal pain.
Pestsepsis
In approximately ten percent of all cases, the plague bacteria get into the blood and cause “blood poisoning”. This so-called Pestsepsis occurs as Complication of bump or lung plague on. Possible symptoms include falling blood pressure, high fever, confusion or lethargy, and digestive problems.
Since the pathogens can spread throughout the body via the blood, the consequences of plague sepsis are manifold and can affect various organs. Especially dangerous are coagulation disorders, because this is associated with bleeding inside the body. Heart stumbling, enlargement of the spleen and liver as well as kidney failure are other possible consequences.
Untreated, the plague septicemia leads to a circulatory failure. If the blood flow in the body can not be maintained, the patient dies from the plague sepsis.
Pest: causes and risk factors
That the plague could rage so extremely in former times, was because people did not know their cause and therefore could not prevent infection. Only for a good 120 years, one knows that the plague of one Bacterium (Yersinia pestis) is triggered. The pathogen mainly occurs in rodents and can be transmitted from their fleas to humans. Patients can also pass on the plague bacteria directly to other people. In pulmonary plague, this happens via droplet infection.
The plague bacterium is highly contagious, Besides, it can be done with a special mechanism outsmart the human immune system: Important defense cells of the immune system are certain white blood cells. They can “eat” intruders such as bacteria and thus stop an infection. Not so with the plague: the “eaten up” plague bacteria simply divide further inside the defense cells.
Where does the plague happen?
Nowadays, the plague no longer exists in many countries. This is because hygiene standards have improved dramatically in many places. Lack of hygiene, rats in the house and a life in slums are namely possible risk factors for the emergence or spread of the plague. Today the plague still occurs in the following regions:
- Africa (especially Central, South and East Africa)
- Asia (especially Russia, Middle East, China, Southeast Asia, Myanmar)
- Central and South America (tropical and subtropical regions)
- North America (southwestern US)
Pest: examinations and diagnosis
If a plague is suspected, the doctor will first discuss it with the patient To raise medical history (Anamnese). For this he asks, for example, the following questions:
- What symptoms do you have exactly?
- Since when do the complaints exist?
- Have you been away lately? If so, where to go?
- Did you have contact with rodents?
- Did you notice insect bites?
- Are you a laboratory worker at S3 security level (these are labs that make the breeding of pest bacteria for sample evaluation)?
Then follows one physical examination, Among other things, the doctor will scan the lymph nodes and look for swelling and pain. Sometimes the typical bumps of the bubonic plague have already formed, which is a clear indication. With lung plague the symptoms are often less clear. Cough, bloody sputum and fever can easily be misinterpreted as severe pneumonia.
You have to do that for a reliable diagnosis Demonstrate plague bacteria in the body, To do this, the doctor pricks into a swollen lymph node, takes a sample and sends it to the laboratory for analysis. In case of suspected lung pneumonia, some expectoration or a saliva sample will be sent. In a plague disease, the triggering bacteria in these secretions or in the sample material from the swollen lymph nodes are detectable.
In addition to this direct pathogen detection is also a blood test important. On the basis of this test it can be determined whether the bacterium is already in the blood (see also: Pestsepsis), and whether the immune system has already recognized the pathogen.
Pest: treatment
If the diagnosis is “plague”, the patient is isolated so that he does not infect anyone. His hospital room may only be entered under strict safety and protection regulations. Any unnecessary contact with the patient is avoided.
The plague is with these days antibiotics treated with, for example, streptomycin, gentamycin, tetracyclines (eg doxycycline) or chloramphenicol. Most doctors administer the drug intravenously via syringe, later in tablet form.
After starting antibiotic therapy, patients with bubonic plague must remain isolated for at least two days, and patients with lung pneumonia at least four days
Pest: Disease course and prognosis
If the bubonic plague is recognized early and treated consistently, the prognosis is good and almost all patients survive. If left untreated, 50 to 60 percent of those affected die.
Pulmonary and pest sepsis have a low chance of survival if patients are not treated quickly. If the doctor makes the diagnosis in good time and starts antibiotic therapy, the mortality rate for these two types of pests drops to about 15 percent.
After surviving pest infection, one is largely immune to re-infection. However, it can sometimes come to a renewed illness. A vaccine against pest is currently not available in Germany.
The plague in the Middle Ages
The plague is one of the major infectious diseases of the Middle Ages. Colloquially she will too Black Death or Black plague called. The name comes from the fact that in the course of the disease the skin may turn black and die off.
In the Middle Ages raged large plague outbreaks in Europe, which claimed lives in the hundreds of millions. But there are also indications that the Black Death existed long before the Middle Ages. However, it is unclear whether this really was an infection with the bacterium Yersinia pestis.
Scientists have gathered much information about the plague in the Middle Ages these days. Thus, the outbreak and the spread of the disease at that time can be well understood. In fact, in the Middle Ages, there were two major plague waves in Europe. The 19th and 20th centuries were followed by a global pandemic, but Europe was largely spared. The spread and distribution of the disease took place in different ways. It is still unclear why the further spread of the plague in Europe between the two major plague waves has not progressed for more than 700 years.
Pest Pandemic 1 (about 541 to 750 AD): The first great wave of the plague in the Middle Ages lasts from about 540 to 750 AD. She came from Egypt across the Mediterranean to Europe to today’s France. During this first major plague pandemic, approximately 100 million people worldwide died, including about half of the European population. There are many theories about the socio-economic and political consequences of this mass extinction in Europe. Some historians associate it with the Arab spread to southern Europe.
Pest Pandemic 2 (14th to 19th centuries): In the years 1340 to 1350, there was a major plague outbreak in Central Asia. Via the trade route Silk Road, the plague returned to Europe and Africa. The world population shrank during that time from about 450 million to 350 million people. The great wave of plague ended just a few years after it began in Asia. However, until the 19th century there were always small outbreaks in Europe.
The black plague: change in medicine
The highly contagious infectious disease plague has led to a fundamental rethinking in medicine. The foundations of our current understanding of diseases and pathways of infection have been marked by important discoveries during that time.
In the Middle Ages, for example, research on the dead was forbidden. Due to the many pest deaths this general ban was slowly dissolved and that Dissecting corpses acceptable. This change is an important moment in the medical understanding of the body.
The next big step was the realization that diseases can be contagious and transmitted through body contact with sick people. However, it took another 200 years before this so-called contagion theory prevailed.
Only with the third major plague plague in the 18th and 19th century, the transmission path of the plague finally cleared. This was because the church view (plague as a punishment of God) was no longer enough for the population to explain. This started the search for more secular explanations. In 1894, the Swiss-French physician and bacteriologist Alexandre Yersin, the pest-Bacterium prove. In his honor, it received its scientific name: Yersinia pestis.
Additional information
guidelines:
- Leading issue “Plague and Pulmonary Disease, Pathogenicity, Epidemiology, Clinic and Therapy” of the Federal Ministry of Health (2015)