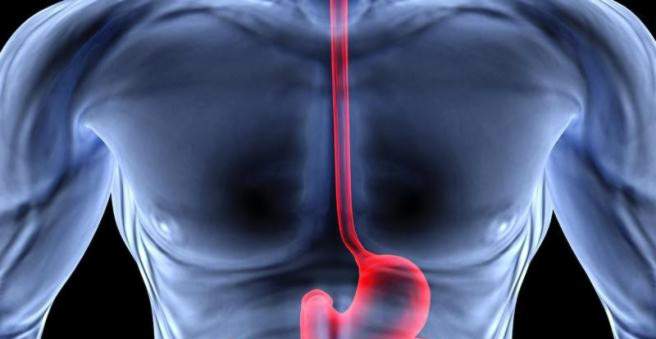
An esophageal carcinoma is a particularly malignant cancer: Since the cancer causes symptoms such as swallowing symptoms only at an advanced stage, it is usually discovered late. As with almost every cancer, a late diagnosis worsens the chances of survival – in the case of an esophageal carcinoma even considerably. The two most common forms of esophageal cancer are squamous cell carcinoma and adenocarcinoma, which develop from different cell types. Here you read everything important about the disease esophageal cancer.
Esophageal cancer: description
Esophageal carcinoma is a relatively common cancer worldwide. However, esophageal cancer is rare in Germany. According to the Center for Cancer Registry Data at the Robert Koch Institute in Germany, about 1,000 women and 4,000 men contract it every year. The mean age of onset is 66 years. Esophageal cancer before the age of 40 is rare. The number of new cases (incidence) has been steadily increasing since the 1980s. Especially in women, the incidence of new esophageal cancer is strikingly high.
Doctors assume that the steadily increasing incidence of esophageal cancer in recent decades is due to lifestyle factors such as overeating, as well as the consumption of alcohol and nicotine. These factors favor the so-called reflux disease. Reflux means that acidic gastric juice enters the esophagus and damages the mucous membrane there. The reflux disease is significantly involved in the development of adenocarcinoma of the esophagus. Although adenocarcinoma is currently the second most common form of esophageal cancer, this form is increasingly common and has contributed significantly to the overall increase in esophageal cancer.
Life expectancy and chances of recovery depend on how far the cancer has progressed when it is discovered. Most of the time, an esophageal cancer is unfortunately only diagnosed late, if it has already spread to the surrounding lymph nodes and neighboring organs (metastasis). At the time of diagnosis, only about 40 percent of those affected can help with surgery. Although the prognosis of esophageal cancer has improved significantly in recent decades due to today’s treatment options, many people die from the tumors. Of the patients who receive the diagnosis of esophageal carcinoma, only about 15 to 20 percent survive the next five years.
An esophageal cancer can basically develop anywhere in the esophagus. In three areas of the esophagus, however, the cancer occurs more often. These are sections where other organ structures narrow the esophagus somewhat: the entrance of the esophagus just behind the throat, in the area where the esophagus passes the aortic arch, and the passage of the esophagus through the diaphragm. Depending on the degenerated cell type, esophageal cancer is classified into various histological forms:
Esophageal cancer: squamous cell carcinoma (about 80 percent)
In a squamous cell carcinoma, the tumor cells develop from cells of the mucosa (squamous epithelium) of the esophagus. This cancer can arise in all sections of the esophagus. About 15 percent occur in the first third of the esophagus, 50 percent in the middle and 35 percent in the last third. Squamous cell carcinoma is favored by heavy alcohol consumption, hot drinks, smoking and fungal toxins.
Esophageal cancer: adenocarcinoma (about 20 percent)
In the case of adenocarcinoma, the tumor arises from altered glandular cells. It forms in 95 percent of cases in the lower section of the esophagus. The cause of this is especially the reflux disease, in which again and again sour stomach contents get into the esophagus. It damages the mucous membrane, which initially leads to cell changes, a so-called Barrett’s esophagus, from which eventually develops into a Barrett’s carcinoma (adenocarcinoma). Adenocarcinomas have increased exponentially in recent decades.
Esophageal cancer: undifferentiated carcinoma (about 10 percent)
If the original cell type, from which the tumor has developed, can no longer be determined with certainty, physicians call this “undifferentiated esophageal carcinoma”. It is the rarest form of esophageal cancer.
Esophageal cancer: symptoms
Everything important to the typical signs of esophageal cancer can be read in review esophageal cancer â € “Symptoms.
Esophageal cancer: causes and risk factors
There are different risk factors for the two main forms of esophageal cancer (squamous cell carcinoma and adenocarcinoma):
Squamous-risk factors: Esophageal cancer, which develops from degenerated cells of the squamous epithelium, is preferably formed by
- Consumption of high-percentage alcohol
- Smoke
- Consumption of hot drinks
- Nitrosamines (which are included in many foods)
- Aflatoxins (poison from molds)
- Achalasia (when the lower esophageal sphincter does not sufficiently relax to pass the food easily.)
Adenocarcinoma risk factors: Five percent of people with reflux disease (chronic heartburn) develop a so-called Barrett’s esophagus, which is a precursor to cancer. The normal mucosal cells of the esophagus change into glandular cells (metaplasia). In ten percent of this precursor is adenocarcinoma of the esophagus, which is also referred to as Barrett’s carcinoma.
There are other factors that favor all forms of esophageal cancer. These include:
- Previous radiotherapy near the esophagus (for example in breast cancer)
- Infection with papillomavirus HPV 16 (also involved in cervical cancer)
- Genetic corneal thickening on hands and feet (Tylosis palmaris and plantaris)
- Narrowing scarring after a caustic soda
- Plummer-Vinson syndrome: a rare disease caused by iron deficiency
In addition to the listed possible causes of esophageal cancer, there are also protective factors. People who take acetylsalicylic acid (Aspirin®, “ASA”) or other non-steroidal analgesic drugs for longer periods of time appear to have fewer oesophageal cancers, according to studies. However, you should not take such medications as a preventive measure because they can cause even serious side effects such as stomach ulcers.
Esophageal cancer: examinations and diagnosis
The right contact for suspected esophageal cancer is a specialist in internal medicine, which specializes in diseases of the digestive tract (Gastroenterology). The doctor first inquires about your current complaints and any previous illnesses (Anamnese). Basically, the symptoms of esophageal cancer occur only in a very advanced stage of the disease (“dull cancer”). For example, your doctor may ask you if you suspect esophageal cancer:
- Have you lost weight in the past few weeks and months?
- Do you suffer from loss of appetite and nausea?
- Do you have pain when swallowing or a feeling of pressure in the throat or behind the breastbone?
- Did you have vomiting?
- Do you take any medicine?
Even if you have already developed an esophageal cancer, such symptoms often occur only occasionally or even not at all. Your doctor also tries to clarify the above-mentioned risk factors for esophageal carcinoma. If any suspicion of oesophageal cancer develops during an exam or in the medical history, your doctor will refer you to a gastroenterologist.
On the anamnesis follows the physical examination, The doctor checks whether lymph nodes are enlarged or nodes are to be touched elsewhere. Since the esophagus can only be assessed from the outside to a very limited extent, further investigations are usually necessary in cases of suspected esophageal cancer.
Further investigations
The esophagus and the ability to swallow are judged by various studies. These include the esophagoscopy, an ultrasound of the esophagus (endosonography) and the so-called Röntgenbreischluck. In the latter case, the patient receives a contrast agent that allows the doctor to closely follow the swallowing process. Further imaging techniques such as computed tomography (CT), magnetic resonance imaging (MRI) or positron emission tomography (PET) can be used to determine the spread of the tumor in the body (staging). Dependent on the result of the staging a stage-dependent therapy takes place.
Esophageal cancer: esophagoscopy
An esophagoscopy is an esophageal reflection. Similar to a gastroscopy, the examiner must be sober for it. He is given a light sleeping aid before the examination, so that he does not consciously experience the examination himself and also feels no pain. For the examination, a tube with a small camera and a light through the mouth is guided into the esophagus. On a screen, the doctor can see if the esophageal mucosa is altered or if it appears narrowed at certain points. If a certain area looks altered, he can use a small pair of pliers to take a tissue sample (biopsy). This usually happens in several places. The samples thus obtained are then examined under the microscope. The histologic examination of tissue samples also detects precancerous lesions such as Barrett’s esophagus.
Esophageal cancer: endoscopic ultrasonography
Endosonography of the esophagus is similar to esophagoscopy in its presentation. In this case, however, an ultrasound head is inserted into the esophagus. Using this method, it is easy to estimate the extent of the affected areas – an important information in esophageal cancer. Forecasting and therapy depend significantly on whether the esophageal cancer already affects deep tissue layers and whether it has already spread to surrounding structures (for example, lymph nodes). In addition, endoscopic ultrasound reveals enlarged lymph nodes.
Esophageal cancer: Röntgenbreischluck
In the so-called Röntgenbreischluck the patient is asked to swallow an X-ray contrast agent. During swallowing is X-rayed. Instead of a single X-ray image, this study provides a short film in which the swallowing motion as well as the size and shape of the esophagus can be assessed. For example, the X-ray crush can be used to detect bottlenecks (stenosis), asymmetry or contour changes in the esophagus. Such changes may indicate esophageal cancer.
Esophageal cancer: imaging
In order to detect the exact spread of esophageal cancer in the body (staging), a computer, nuclear spin or positron emission tomography is usually performed. For these examinations, the patient is driven on a couch into a tube in which images of the affected body parts are created. Each of these investigations has advantages and disadvantages. Therefore, the doctor decides individually which of the methods makes the most sense. Sometimes the patient receives a contrast medium to drink before the examination.
The purpose of these different procedures is to determine where exactly the tumor sits, to which neighboring structures it is adjacent, and how tall it is. The crucial factor is whether the esophageal cancer has already spread to lymph nodes or other organs. This information determines the later therapy of esophageal cancer. Healing chances are greater, the smaller the tumor is – and the less it has already spread. Even with an advanced disease can be treated by a closer examination more targeted and improve the esophageal cancer prognosis.
Esophageal cancer: Complementary diagnosis
If it is suspected that the esophageal cancer has already grown into the larynx or bronchial tubes, a reflection of these organs is necessary (bronchoscopy, laryngoscopy). The examination is similar to a gastroscopy. However, a slightly thinner hose is used. In other cases, an ultrasound of the upper abdomen is performed.
If conspicuous structures appear in the bone on CT, MRI, PET or X-ray images, bone scintigraphy makes sense. For this purpose, a contrast agent is injected into the arm vein of the patient, which accumulates in the metabolically active, well-perfused areas in the bone. That also applies to metastases. In pictures shot by a so-called gamma camera, secondary tumors (metastases) then appear as dark spots.
Esophageal cancer: treatment
Various procedures are available for the treatment of esophageal cancer. Surgery, radiation or chemotherapy – which therapy option is used depends on how big the tumor is, whether it has spread in the body and what the general condition of the patient is. Frequently, different methods will also be combined. A special case is patients whose esophagus is so narrowed by the tumor that they can no longer receive food. In that case, the doctor may stretch the esophagus (bougienage) and insert a metal tube (stent) that will open the way for food.
Esophageal cancer: surgery
If discovered at a very early stage, the chances of esophageal cancer healing are very high. In many cases, the tumor can then be easily removed as part of an esophageal reflection (endoscopically). If the tumor is more advanced, a major intervention is necessary. The entire esophagus is removed along with the associated lymph nodes. In order for the patients to be able to eat again after the operation, the doctor inserts a piece of the small intestine instead of the esophagus. Alternatively, he can suture the stomach directly to the upper rest of the esophagus (gastric pull). If the surgeon succeeds in completely removing the tumor and has not yet spread metastasis, this procedure may be sufficient for complete cure until stage IIa.
Esophageal cancer: chemo and radiation
In advanced esophageal cancer, it has been proven to perform chemotherapy or radiation in addition to surgery. Chemotherapy or radiation are sometimes performed prior to surgery to reduce the size of the tumor (downstaging). This should make the surgical procedure less serious, which reduces the surgical risk for the patient. Despite this combined therapy, only 35 percent of those affected survive a complete removal of esophageal carcinoma. Scientific studies are currently testing whether chemotherapy should be combined with radiation to improve the esophageal cancer prognosis. This form of therapy (chemotherapy + radiation) is also chosen if no surgery can be performed.
Esophageal cancer: palliative therapy
A highly advanced esophageal cancer can not be cured anymore. So that the patient still has as few complaints as possible, a palliative (symptom-reducing, non-healing) therapy is performed. It is determined individually and may include chemotherapy or radiation. In the end stage of esophageal cancer, the patient may also be fed extra food through a nasogastric tube.
Esophageal cancer: disease course and prognosis
Esophageal cancer grows rapidly into the surrounding organ structures. First, it expands into the outer wall layers of the esophagus. In the end stage of the esophageal cancer, the lung mantle, the heart mantle, the diaphragm, the aorta, the vertebral bodies or the trachea may also be affected. However, before the tumor attacks these other organs, it usually spreads first into the lymph nodes. Through the blood vessels, cancer cells spread and also settle in the liver, the lung, in the brain or in bones. Unfortunately, such metastases are not uncommon in esophageal cancer.
Unfortunately, life expectancy and prognosis of this tumor disease are still poor overall. This is mainly because esophageal cancer is usually only discovered when the tumor is already relatively large and has spread to the lymph nodes. That’s the case with 90 percent of patients. The more advanced the disease, the worse the prognosis. At a very early stage, the tumor may be eroded and healed as part of oesophageal specimens or surgery.
If the cancer has already spread, only 35 percent of patients will survive the next five years – even if the tumor has been completely surgically removed and he has subsequently received chemotherapy or radiation. If surgery is discontinued and only chemo and radiation are performed, 30 percent will survive the next three years. Patients at increased risk should be checked regularly by an internist so that they can have one esophageal cancer can recognize in time.