Dementia refers to a persistent or progressive impairment of memory, thinking or other brain functions. The cause can be different. Thus, there are various forms of dementia such as Alzheimer’s disease or vascular dementia. Read more here: What is dementia (definition)? Which forms are there? How do you recognize dementia? How is she diagnosed and treated?

Dementia: short overview
- Important dementia forms: Alzheimer’s Disease, Vascular Dementia, Lewy Body Dementia, Frontotemporal Dementia
- symptoms: In all forms of dementia mental performance is lost in the long term. Other symptoms and the exact course vary depending on the dementia form.
- Affected: Mainly people over 65 years. Most dementia patients are women because on average they are older than men.
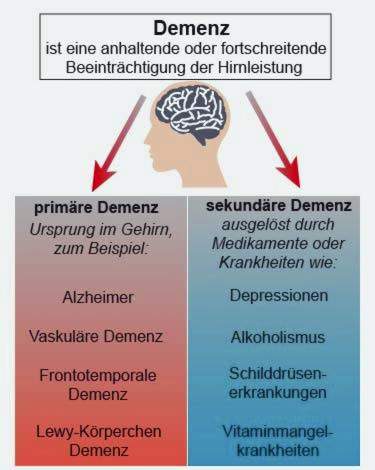
- Causes: Primary dementias (like Alzheimer’s disease) are independent diseases in which neurons gradually die off in the brain – the exact reason for this is unknown. Secondary dementias are the result of other illnesses (such as alcohol addiction, depression) or medications.
- Treatment: Medicines, non-pharmacological measures (such as occupational therapy, behavioral therapy, music therapy, etc.)
- Is dementia curable? Primary dementia is not curable. However, the right treatment can delay the course. Secondary dementia can sometimes be cured if the cause is identified early and treated.
What is dementia?
The term dementia does not refer to a particular illness, but the common occurrence of certain symptoms (“syndrome”), which can have a variety of causes. Overall, the term includes more than 50 disease forms (such as Alzheimer’s disease or vascular dementia).
Allen dementia forms together is the persistent or progressive impairment of memory, thinking and / or other brain functions, Often, other symptoms (such as interpersonal behavior) are added.
Primary and secondary dementia
Under the term “primary dementia“All forms of dementia, which are independent clinical pictures, fall, they have their origin in the brain, where more and more nerve cells die.
The most common primary dementia (and generally the most common dementia disorder) is Alzheimer’s disease. Second is vascular dementia. Other primary forms of dementia include frontotemporal and Lewy body dementia.
When “secondary dementia “ are dementia-related diseases that are caused by drugs or other diseases such as depression, alcoholism, thyroid disease or vitamin deficiency diseases. Secondary dementia forms are rather rare.
There are also mixed forms dementing disease processes, especially mixed forms of Alzheimer’s disease and vascular dementia.
Cortical and subcortical dementia
Another classification of diseases is based on where the changes occur in the brain: The Cortical dementia is associated with changes in the cerebral cortex (Latin: cortex cerebri). This is the case with Alzheimer’s disease and frontotemporal dementia.
When subcortical dementia On the other hand, it refers to dementia with changes below the cerebral cortex or in deeper layers of the brain. These include subcortical arteriosclerotic encephalopathy (SAE), a form of vascular dementia.
However, this classification is not unproblematic, because there are many mixed and transitional forms. For example, dementia with Lewy bodies may manifest as either a cortical or a mixed form.
Dementia syndrome
The term dementielles syndrome is often equated with “dementia”. This is understood as a general intellectual degradation, for example memory and orientation disorders as well as speech disorders. Over time, the personality of the patient often changes.
It is necessary to underestimate dementia syndrome by pseudo-dementia. This term includes temporarily occurring brain disordersthat are faked by a thought and drive inhibition. Most commonly, pseudo-dementia develops as part of a major depression.
You can read more about dementia syndrome and pseudodeficiency in the article Dementia syndrome.
Senile dementia and senile dementia
Because especially older people are becoming dementia, one often speaks of senile dementia. However, this term is not to be equated with “senile dementia”: the latter refers to “senile dementia of the Alzheimer type” (SDAT) – a manifestation of Alzheimer’s disease in old age. In contrast, there is the pre-Alzheimer’s disease, which usually occurs in the 5th or 6th decade of life.
Today, Alzheimer’s disease is predominantly referred to as Alzheimer’s disease or dementia of the Alzheimer’s type (DAT).
Dementia: symptoms
In the case of dementia, intellectual capacity is lost in the long term. In detail, the symptoms of dementia depend on which condition it is – for example, Alzheimer’s or vascular dementia.
Alzheimer’s disease
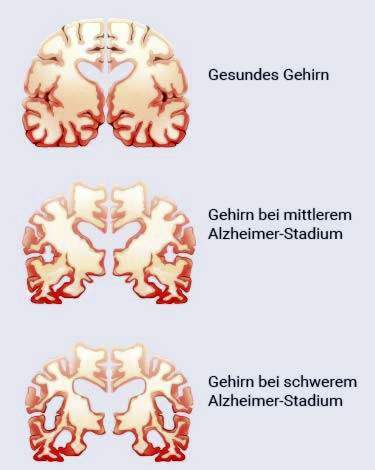
Alzheimer’s (and many other types of dementia) onset dementia symptoms are short-term memory issues: people become increasingly forgetful, often misplacing things and having a hard time concentrating. Sometimes common concepts suddenly fail to come to their mind in conversation. Orientation problems in a foreign environment are also the first signs of dementia of the Alzheimer’s type.
Advanced dementia symptoms in Alzheimer’s patients affect long-term memory. Patients are less and less able to remember the past. At some point, they can no longer recognize persons close to them. In late stages of dementia, the patients also build physically and need help with all activities.
Read more about symptoms, causes, diagnosis and treatment of this most common form of dementia in the article Alzheimer’s Disease.
Vascular dementia
Vascular dementia is the result of circulatory disorders in the brain. It often shows similar dementia symptoms as in Alzheimer’s. However, the exact condition of vascular dementia depends on where in the patient’s brain circulatory disorders occur and how pronounced they are.
Possible symptoms include problems with attentive listening, coherent speech and orientation. These dementia signs are also present in Alzheimer’s, but often appear earlier and more violent in vascular dementia. In addition, the memory in vascular dementia can be retained longer.
Other possible signs of vascular dementia include gait disturbances, slowing, bladder emptying, difficulty concentrating, personality changes and psychiatric symptoms such as depression.
Read more about symptoms, causes, diagnosis and treatment of this second most common form of dementia in the article Vascular Dementia.
Lewy body dementia
The Lewy body dementia also manifests itself with similar dementia symptoms as Alzheimer’s disease. However, many patients show hallucinations (hallucinations) in the early stages of the disease. Memory usually lasts longer than Alzheimer’s.
In addition, many people with Lewy Body dementia show Parkinson’s symptoms. These include stiff movements, involuntary trembling and an unstable posture. Therefore, those affected fluctuate and fall frequently.
Another peculiarity of this type of dementia is that the physical and mental state of the patient sometimes fluctuates greatly. At times, the affected are enterprising and wide-awake, then again confused, disoriented and withdrawn.
Read more about the symptoms, causes, diagnosis and treatment of this form of dementia in the article Lewy Body Dementia.
Frontotemporal dementia
A quite different course shows the frontotemporal dementia – also called Pick disease or Pick’s disease. Typical symptoms of dementia here are changes in personality and often strange behavior: those affected are usually easily irritable, aggressive and act tactless or embarrassing. Excessive eating and apathy are also possible.
Due to the conspicuous and antisocial behavior of many patients, it is often suspected that a mental disorder rather than dementia is present. Only in the advanced stage of Pick’s disease typical dementia symptoms such as memory problems occur. In addition, the language of the patients is impoverished.
Read more about symptoms, causes, diagnosis and treatment of this rarer form of dementia in the article Frontotemporal Dementia.
Difference: Alzheimer’s and dementia of another kind
“What is the difference between Alzheimer’s and dementia?” This question is asked by some people affected and their relatives on the assumption that it would be two different clinical pictures. In fact, Alzheimer’s is just one form of dementia, by far the most common. Correctly, therefore, the question should be what the difference between Alzheimer’s and other forms of dementia is, such as vascular dementia:
A typical difference between these two most common forms of dementia concerns the onset and course of the disease: Alzheimer’s usually begins insidiously and the symptoms slowly worsen. On the other hand, vascular dementia often starts suddenly and the symptoms increase by degrees.
So much for the theory – but the practice often looks a bit different. Any dementia can vary from patient to patient, making it difficult to distinguish. In addition, there are mixed forms, such as Alzheimer’s and vascular dementia. Those affected show features of both dementia forms, which is why a diagnosis is often difficult.
Read more about the similarities and differences between important forms of dementia in the article Difference between Alzheimer’s and dementia?
Dementia: causes and risk factors
In most cases of dementia, it is a primary disease (primary dementia), so a separate disease originating in the brain: in those affected successively nerve cells die, and the connections between the cells are lost. Physicians speak here of neurodegenerative changes. The exact reason varies depending on the form of primary dementia and is often not fully understood:
Alzheimer’s dementia: causes
In the most common form of dementia, so-called plaques form in the brain. These are deposits of a diseased protein (beta-amyloid). Physicians suspect that these plaques contribute to or at least favor Alzheimer’s disease.
Why the plaques form is not known exactly. Rarely – in about one percent of cases – are the causes of genetic nature: Changes in the genome (mutations) lead to plaque formation and disease outbreak. Such mutations make hereditary Alzheimer’s dementia hereditary. In the vast majority of cases, you do not know exactly why someone has Alzheimer’s disease.
Vascular dementia: causes
In vascular (vascular) dementia circulatory disorders in the brain lead to the death of nerve cells. They may, for example, be the result of several small strokes (due to vascular occlusion) that occur simultaneously or at different times in a brain region (“multi-infarct dementia”). Sometimes, vascular dementia also develops on the basis of a major cerebral hemorrhage, such as in hypertensive patients. More rare causes of vascular dementia include vascular inflammation and genetic diseases.
Lewy body dementia: causes
In Lewy body dementia, protein residues from alpha-synuclein are deposited in the nerve cells of the cerebral cortex. These so-called Lewy bodies hinder the communication of nerve cells with each other. Why they form is usually unknown. Very rarely, the disease is genetically determined.
Frontotemporal dementia: causes
In frontotemporal dementia, neurons in the frontal and temporal lobes of the cerebrum gradually die. Again, the cause is largely unknown. In part, the cases are genetically determined.
Secondary dementia: causes
The rare secondary dementias are caused by other illnesses or medications. They can be triggered for example by depression, alcoholism, thyroid disorders or a vitamin deficiency. Also medications are possible dementia causes.
Risk factors for dementia
Higher age and a corresponding genetic predisposition increase the risk of a dementing disease. Other risk factors include hypertension, diabetes mellitus, cardiac arrhythmia, high cholesterol, depression, brain injury, smoking, excessive alcohol consumption and obesity.
Even people with low mental, social and physical activity are more susceptible to dementia.
Dementia: examinations and diagnosis
The fact that you often forget something when you are older is not necessarily a cause for concern. But if the forgetfulness persists for months or even increases, you should go to the family doctor. If there is a suspected dementia, he can refer the patient to a specialist (neurological practice or memory outpatient clinic).
History Talk
The doctor will first ask the patient about his complaints and his general state of health (anamnesis interview). He will also ask if the patient is taking any medications and if so, which ones. Because many preparations can temporarily or permanently worsen brain function. During the conversation, the doctor also pays attention to how well the patient can focus on the conversation.
Often, the doctor also talks with close relatives. For example, he asks her if the patient is more restless or aggressive than before, is very active at night, or has hallucinations.
Cognitive dementia tests
Using a variety of tests, the doctor can determine if someone has a dementia and how severe it is. Frequently used dementia tests include the watch test, MMST and DemTect. They are easy to do and do not take much time. Their informative value in mild and questionable dementia is limited. In addition, these cognitive short tests are not suitable for differentiating the various dementias.
clock test
The clock test helps to detect dementia early on. For this purpose, however, it is always combined with another test: the result of the watch test alone is insufficient for a diagnosis.
The process of the clock test is quite simple: The patient should enter the numbers 1 to 12 in a circle, as they are arranged on a dial. He should also draw the hour and minute hands in such a way that gives a certain time (for example, 11:10 clock).
For example, in the evaluation, the doctor checks to see if the numbers and hands are correctly drawn and the numbers are legible. From errors and deviations he can conclude a possible dementia. For example, people with incipient dementia often place the minute hand incorrectly, but the hour hand correctly.

Read more about this test procedure in the article clock test.
MMSE
The abbreviation MMST stands for “Mini Mental Status Test”. It is a very common dementia test. The patient has to complete a simple questionnaire that examines various brain functions such as memory, attention, and arithmetic. The orientation ability of the patient is also tested with questions like “Which season do we have?” or “In what place are we?”. Each answer is scored with a score.
At the end of the test all scored points are added together. The result is used to estimate the severity of dementia. With regard to Alzheimer’s – the most common form of dementia – a distinction is made between the following dementia stages:
- MMST 20 to 26 points: mild Alzheimer’s dementia
- MMST 10 to 19 points: moderate / moderate Alzheimer’s dementia
- MMST <10 points: severe Alzheimer's disease
Find out more about the procedure and the evaluation of the “Mini Mental Status Test” in the article MMST.
DemTect
The short name DemTect stands for “Dementia Detection”. The approximately ten-minute test tests various cognitive abilities such as memory. For this purpose ten words are read to the patient (dog, lamp, plate, etc.), which he then has to repeat. The order does not matter. It is counted how many of the terms the patient could remember.
In another task, the patient should enumerate as many things as possible, which can be bought in a supermarket. This examines the semantic fluency.
Points are awarded for each task. At the end of the test you count all the points together. From the overall result, it can be estimated whether and how much the patient’s cognitive performance is impaired.
Read more about this test procedure in the article DemTect.
Physical examination
A physical examination is important to rule out other disorders as the cause of the suspected dementia symptoms. It also helps to determine the physical condition of the patient. For example, the doctor measures blood pressure, examines the muscle reflexes and the reaction of the pupils to light.
laboratory tests
Dementia diagnostics also includes one blood test, Here, the blood count is created and various blood levels determined (electrolytes such as sodium and potassium, fasting blood glucose, blood sediment, urea, vitamin B12, thyroid levels, gamma GT, etc.). This can be used to determine if there may be secondary dementia, such as thyroid disease or vitamin B12 deficiency.
In some cases further laboratory tests necessary, for example when the dementia patient is remarkably young or the symptoms progress very rapidly. Then, for example, the doctor orders drug screening, urine tests and / or a test for Lyme disease, syphilis and HIV.
If the medical history and the previous investigations indicate a suspected inflammatory brain disease, one should Sample of nerve water (Liquor) taken from the lumbar spine and analyzed in the laboratory. This CSF diagnosis may also be indicative of Alzheimer’s disease: Characteristic changes in the concentration of certain proteins (amyloid protein and tau protein) in the CSF are highly likely to indicate Alzheimer’s disease.
Imaging procedures
Imaging studies of the brain serve to exclude treatable causes of dementia (such as a tumor). In addition, they help distinguish between the different forms of primary dementia (Alzheimer’s, vascular dementia, etc.).
Above all, they are used Computed tomography (CT) and Magnetic Resonance Imaging (MRI), Sometimes, however, other investigations are carried out. These include, for example, an ultrasound examination of the cervical vessels in suspected vascular dementia. In unclear cases of Lewy body dementia, a nuclear medical examination may be useful (positron emission tomography = PET, single photon emission computed tomography = SPECT).
Genetic examination
If it is suspected that the dementia disease is hereditary, the patient should be offered a genetic counseling and examination. The result of the genetic test has no influence on the therapy. However, some patients want to know exactly whether or not they actually carry a disease-causing gene.
Dementia: treatment
Despite various treatment options for dementia: curable, the disease is usually not (exception: some secondary dementias). Instead, the therapy aims to alleviate the symptoms and slow the progression of the disease. This helps the patient to lead an independent and self-determined life as long as possible.
The dementia therapy consists of a drug treatment and non-drug measures together. For each patient an individually fitting therapy plan is created. Especially in the choice of non-drug measures, the personality and wishes of the patient should be considered. The chances of success of the treatment are greater the earlier the therapy is started.
Dementia drugs (anti-dementia drugs)
In the drug dementia therapy especially so-called anti-dementia drugs are used. They influence different messenger substances in the brain. As a result, they can maintain the mental capacity of patients. However, anti-dementia drugs usually only have a limited time.
Anti-dementia drugs have been used primarily in the treatment of Alzheimer’s disease. Approved are acetylcholinesterase inhibitors and the glutamate antagonist (NMDA antagonist) memantine.
acetylcholinesterase (like donepezil or rivastigmine) inhibit an enzyme in the brain that breaks down the nerve messenger acetylcholine. This messenger substance is important for the communication between the nerve cells. It is not produced in sufficient quantities in Alzheimer’s patients, which contributes to the symptoms. Acetylcholinesterase inhibitors can compensate for this messenger deficiency in early and middle stages of Alzheimer’s disease. Then patients can master their daily lives better again. In addition, brain services such as thinking, learning and remembering are retained longer.
Acetylcholinesterase inhibitors are also often used in other forms of illness, such as Lewy body dementia and mixed forms.
Of theGlutamate antagonist memantine blocked in the brain the docking sites for the nerve messenger glutamate. Its concentration may be increased in Alzheimer’s disease, which permanently destroys the nerve cells. Memantine (neuroprotection) protects against irreversible nerve damage. They are used in middle and late stages of Alzheimer’s disease.
Often also preparations based on the medicinal plant “Ginkgo biloba” in dementia are recommended. They are considered to be less effective, but can be used as a supplement.
Other drugs in dementia
When people experience that they are demented, many develop a depressive mood. Even the downfall of brain cells themselves may be responsible for depression. In such cases, the doctor may antidepressants prescribe. They have a mood-enhancing and drive-enhancing effect.
Some patients become aggressive and restless, suffer from hallucinations or paranoia. Such symptoms can be associated with neuroleptics (such as risperidone, melperone or pipamperone). Their use is due to the strong side effects but very carefully checked and limited in time.
For vascular dementia, risk factors and underlying diseases that could lead to further vascular damage should be treated. This includes, for example, the gift of antihypertensives in hypertension and of lipid-lowering agents with elevated blood lipid levels (such as elevated cholesterol levels).
behavior therapy
The diagnosis of dementia causes insecurity, anxiety, depression or aggressiveness in many people. A psychologist or psychotherapist can help those affected to better deal with their illness through behavioral therapy. Thus, a behavioral therapy is particularly suitable for patients in early dementia stages.
Cognitive training
Cognitive training can slow down the progression of dementia, especially in early and middle stages of the disease. It trains mental (cognitive) skills, such as memory, attention, and orientation. For example, in individual or group therapy, patients need to guess terms, name colors, and add rhymes. Cognitive training should be designed for each patient so that it is neither understatement nor excessive.
Autobiographical work
Autobiographical work can be useful in early to middle stages of dementia: In talks (individual or group therapy), the patient should use pictures, books and personal objects to link up with and relate to past positive experiences. This autobiographical work keeps the memories of a dementia patient awake to his former life and strengthens the feeling for one’s own identity.
reality Orientation
In the orientation to reality, the patients train to orient themselves spatially and temporally and to classify persons and situations better. The temporal orientation can be supported with watches, calendars and images of seasons. For example, to enable patients to find their way around the room (in their home, for example), different living spaces (bathroom, kitchen, bedroom, etc.) can be labeled with different colors.
The orientation to reality makes sense in all stages of the disease. It can be trained individually or in groups.
music therapy
The purpose of music therapy in dementing illness is based on the fact that music can evoke positive memories and feelings. In early stages of dementia, patients – singly or jointly – can play an instrument themselves (drum, triangle, glockenspiel, etc.) or sing. In advanced dementia, at least listening to familiar melodies can calm or calm a patient.
occupational Therapy
In order for patients in the early to middle stages of dementia to be able to cope with everyday activities such as shopping, cooking or reading newspapers for as long as possible, they should regularly practice these activities with a therapist.
In middle to severe stages of the disease, dancing, massage and touch stimulation can encourage physical activity. This can give the patient pleasure and improve their well-being.
milieu therapy
Milieu therapy is about making the patient’s environment suitable for dementia. Those affected should feel safe and comfortable in their living and living spaces. The rooms should therefore be designed as suitable as possible. For example, smooth wood and soft fabrics are perceived by most patients to be very pleasant. Well-known fragrances (such as room fragrance) and favorite flowers can give the patients pleasure, calm or cheer them up and bring back beautiful memories.
Nursing planning: dementia
Sooner or later, dementia patients need help in everyday life, such as dressing, washing, shopping, cooking and eating. The patients and their relatives should therefore deal with the subject as early as possible and take care of the planning of future care.
Important questions that need to be clarified are, for example: Can and does the dementia patient want to stay in his own apartment? What help does he need for his everyday life? Who can provide this help? Which offers of outpatient care are there? If a home care is not possible – which alternatives are in question?
Everything important around topics such as care in the family, ambulant nurses and nursing home read in the article Care planning: dementia.
Dealing with dementia
When one’s own mental capacity decreases, it is frustrating and frightening for many. The relatives often find it difficult to cope with dementia and its consequences.
Above all, dealing with dementia requires patience and understanding – from the patient as well as the relatives and caregivers. In addition, much can be done to slow down mental decline. This includes regularly training the existing cognitive abilities, for example by reading or solving crossword puzzles. Other hobbies such as knitting, dancing or building model airplanes should be continued – if necessary with necessary adjustments (such as lighter knitting patterns or simpler dances).
In addition, dementia patients also benefit from a balanced diet, regular exercise and a structured daily routine.
Read more tips for everyday life with dementia in the article dealing with dementia.
Help with dementia
There are many different associations, institutions and organizations that provide information and assistance to dementia patients and their relatives. These include, for example, the German Alzheimer’s Society, the German Senior League and the Association “Friends of Old People”.
If you would like to remodel your own home for an elderly or dementia sufferer, you can contact the Federal Working Group for Housing Adaptation e.V. for tips and information. If a move to a retirement or nursing home is necessary, Heimverzeichnis.de offers help in the search for a suitable facility.
You can read more about these and other contact points for dementia patients and their relatives in the article Dementia Help.
Dementia: disease course and prognosis
In any form of dementia mental performance is lost in the long term. The personality of the patient is also irreversibly impaired.
In individual cases, however, the course of dementia can vary greatly from patient to patient. It depends mainly on the type of disease. For example, a vascular dementia often occurs suddenly and worsens in batches. In most cases, however, dementia begins insidiously and progresses slowly.
In addition, a dementia patient can sometimes have “good” and sometimes “bad” days. The condition of the patient can also vary during the course of the day. Dementia is stronger in the evening than during the day.
The behaviors of dementia sufferers are also very different. Some patients become increasingly aggressive, others remain friendly and calm. Some patients are physically fit for a long time, others become bedridden.
Insgesamt gilt also: Der Demenz-Verlauf kann individuell sehr unterschiedlich sein. Er lässt sich auch nur schwer vorhersagen.
Demenz-Verlauf beeinflussen
Demenz ist nicht heilbar. Mit Aktivierung, Beschäftigung und menschlicher Zuwendung lässt sich aber die Lebensqualität von Demenzkranken deutlich verbessern. Außerdem kann die richtige Therapie (Medikamente und nicht-medikamentöse Maßnahmen) helfen, den Demenz-Verlauf vorübergehend aufzuhalten oder zumindest zu verlangsamen.
Demenz: Vorbeugung
Viele Faktoren begünstigen eine dementielle Erkrankung. Wenn es gelingt, diese Risikofaktoren zu meiden oder zumindest zu reduzieren, hilft dies, einer Demenz vorzubeugen.
So sollte man zum Beispiel Bluthochdruck, erhöhte Blutfettwerte und Übergewicht behandeln – nicht nur mit Medikamenten, sondern auch mit dem richtigen Lebensstil. Beispielsweise scheint eine mediterrane Ernährung vor Demenz zu schützen: Sie beinhaltet viel Obst und Gemüse, Fisch, Olivenöl und Vollkornbrot. Dagegen sollten Schweinefleisch und Milchprodukte nur in Maßen konsumiert werden.
Von regelmäßiger Bewegung profitieren das Gehirn und der restliche Körper in jedem Alter. So regt körperliche Aktivität die Durchblutung und den Stoffwechsel im Gehirn an. Die Nervenzellen sind dadurch aktiver und vernetzen sich besser. Sport und Bewegung im Alltag senken außerdem den Blutdruck und den Cholesterinspiegel und beugen Übergewicht, Diabetes, Herzinfarkt, Schlaganfall und Depressionen vor. Darüber hinaus hält regelmäßige Bewegung die Gefäße gesund, was vor vaskulärer Demenz schützt. Doch nicht nur zur Vorbeugung eignet sich körperliche Aktivierung: Demenz-Patienten profitieren ebenfalls davon.
Empfehlenswert ist auch “Gehirntraining”: Wie die Muskeln sollte auch das Gehirn regelmäßig gefordert werden. Dafür eignen sich zum Beispiel kulturelle Aktivitäten, mathematische Rätsel oder kreative Hobbies. Solche geistige Aktivität in Beruf und Freizeit kann das Risiko einer Demenz reduzieren.
Will man einer Demenz vorbeugen, sollte man außerdem soziale Kontakte pflegen. Je mehr man sich unter Leute begibt und mit anderen Menschen austauscht, desto wahrscheinlicher ist man auch im hohen Alter noch geistig fit – ein wichtiger Schutz vor Demenz.
Weiterführende Informationen:
Bücher:
- Das Herz wird nicht dement: Rat für Pflegende und Angehörige (Udo Baer und Gabi Schotte-Lange, Beltz, 2017)
- Alzheimer & Demenzen verstehen: Diagnose, Behandlung, Alltag, Betreuung (Wolfgang Maier, Jörg B. Schulz, Sascha Weggen und Stefanie Wolf, TRIAS, 2011)
guidelines:
- S3-Leitlinie “Demenzen” der Deutschen Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde und der Deutschen Gesellschaft für Neurologie (2016)