Myasthenia gravis is a nerve disease that disturbs the signal transmission between the nervous system and the muscles. The causes are so far unclear. Myasthenia gravis is characterized by muscle weakness, which may be slightly different in each affected person. Symptomatic therapy is possible, but the disease is not curable. Read all important information about Myasthenia gravis here.
Myasthenia gravis: description
Myasthenia gravis is a neurological disorder characterized by muscle weakness or failure of individual muscles. It interferes with the transmission of signals between the nervous system and the muscles. As a result, myasthenia gravis does not produce continuous symptoms, in which individual muscles or muscle groups are alternately weakened or can no longer be moved (especially on the face). The weakness can occur spontaneously or slowly increase during the day. How it comes to the disturbance of the signal transmission, is still unclear.
Myasthenia gravis is a relatively rare disease. On average, about 100 to 200 out of a million people get it. In general, myasthenia gravis can occur at any age. However, the 20 to 30 year olds and the 60 to 80 year olds are particularly likely to be affected. Women are more likely to develop myasthenia gravis than men. In recent years, the number of reported illnesses has increased sharply. However, according to scientists, this increase is not due to an increase in actual cases, but rather due to the higher profile of myasthenia gravis.
Once the disease has developed, it will last a lifetime, affecting sufferers more and less of muscle weakness. Therapy and prognosis depend on the stage in which the disease is detected. Myasthenia gravis is not curable, only the symptoms can be relieved with medication.
By the way, dogs can also get myasthenia gravis.
Myasthenia gravis: symptoms
The symptoms that occur in myasthenia gravis are varied and vary from patient to patient. In general, various muscles and muscle groups of the skeleton (striated muscles) are affected by muscle weakness, where movements can be performed with less force or less accuracy. Myasthenia gravis does not affect myocardium and musculature of the internal organs as they belong to a different type of muscle (smooth muscle) and are otherwise supplied with signals.
In principle, Myasthenia gravis can extend to all skeletal muscles. At the beginning of the disease usually only smaller muscles are affected. In the morning and after rest periods, the symptoms are often weaker, in the evening and after physical exertion, they are usually stronger.
In about half of all affected people, the first symptoms on the face are noticeable, especially in the eyes. Sufferers often suffer from the so-called bedroom view, in which the upper lid of the eye hangs down and can no longer be deliberately lifted (ptosis). Often sufferers report double vision or the inability to close their eyes completely. Also in the initial phase is often the mimic muscles affected by muscle weakness. Patients find it difficult to close their mouths properly, to laugh, to chew or to talk. Often, the neck muscles are compromised, which makes it difficult for the patient to keep her head upright.
If muscle weakness spreads to the chewing and pharyngeal muscles, problems with eating and swallowing initially occur. Dangerous it becomes with a stronger paralysis, because then it becomes impossible to swallow the own saliva. In the advanced stage, the inability to swallow can go so far that those affected artificially fed and the saliva must be vacuumed regularly.
If the limbs of Myasthenia gravis are affected, the symptoms in the arms are often more severe than in the legs.
Myasthenia gravis: complications
Myasthenia gravis becomes life threatening if the respiratory muscles are compromised. In severe cases mechanical ventilation is necessary. Even with dysphagia, complications can occur, for example, when swallowed is in the lungs instead of the esophagus. As a result, pneumonia (aspiration pneumonia) often occurs.
To make matters worse, especially in older people, the myasthenia gravis symptoms are often misinterpreted or not properly considered. As a result, in many cases treatment is too late or not at all, which causes the symptoms to continue to worsen.
Myasthenic crisis
As a myasthenic crisis, medical professionals refer to a sudden worsening of the condition of myasthenia gravis patients with severe dysphagia and respiratory problems. Those affected must be hospitalized; even when being treated in an intensive care unit, the risk of dying from a myasthenic crisis is still five percent. The cause of a myasthenic crisis are infections, errors in taking medication (for example, too low a dosage), as well as an early termination of therapy.
Myasthenia gravis: causes and risk factors
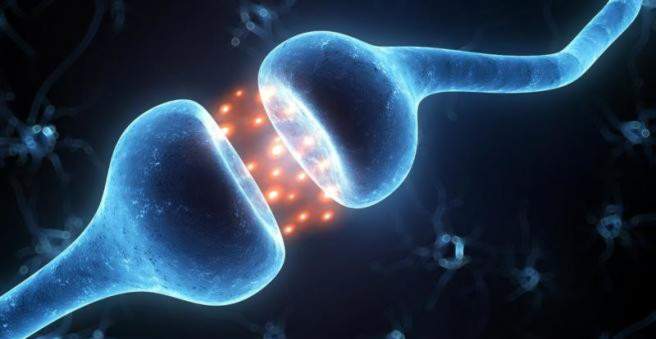
To date, the causes of myasthenia gravis are not fully understood. It is known that myasthenia gravis is one of the autoimmune diseases. This means that the immune system forms antibodies (antibodies) against the body’s own structures that destroy them. In myasthenia gravis, antibodies are formed that destroy the docking sites (receptors) of certain neurotransmitters, thereby impeding signal transmission in the body.
In order to transmit a signal from the brain to the muscles, the signal is transcoded at the end of a nerve, that is, the electrical signal in the nerve now becomes a chemical signal that excites the muscles. For this purpose, messenger substances (transmitters) are distributed. These bind to the muscle cells at specific docking sites (receptors). So the muscle gets excited, it contracts and allows a certain movement. For a single motion, quite a few such signals are combined and merged into one directional motion.
In myasthenia gravis, the receptors on the muscle cells are partially or completely blocked or even destroyed. This gives the muscle less or no signals from the brain. With fewer signals, only the precision and power of the movements are reduced. If no signals are received, the muscle is paralyzed. This severe form of myasthenia gravis is very rare.
The role of the thymus
Scientists suspect a link between myasthenia gravis and abnormal changes in the thymus. The thymus is an organ in which various cells of the immune system (including antibodies) are formed during childhood. In about 10 percent of all myasthenia gravis patients there is a tumor in the thymus (thymoma), in about 70 percent of all patients in the thymus demonstrated an increased activity (thymitis).
External factors influence the symptoms
It is believed that variations in the severity of the symptoms are caused by external factors such as environmental factors, inflammation, mental and psychological stress and other existing illnesses. However, this connection is not conclusively clarified.
Myasthenia gravis: examinations and diagnosis
In order to rule out other diseases and to be able to make a diagnosis that is as clear as possible, different methods of examination are used if myasthenia gravis is suspected.
The suspicion of myasthenia gravis comes to the doctor on the basis of the clinical picture in the physical examination and the recording of the medical history (anamnesis). Typical questions of the anamnesis can be:
- Where exactly do you feel the muscle weakness?
- Since when do you already feel these symptoms?
- When do these onset of weakness occur, in the morning or in the evening, or after you’ve gone to the trouble?
- Do you have problems with chewing, swallowing or speaking?
Simple tests can confirm the suspicion of myasthenia gravis, but they do not allow for accurate diagnosis.
Very often the so-called Simpson test is carried out. Affected persons have to look up as long as possible and open their eyelids wide. As a rule, the eyelids tire quickly, depending on the stage of the disease, the opening of the eyelids is no longer possible. After the administration of a certain drug (Tensilon), these symptoms temporarily disappear.
Another method of investigation for suspected myasthenia gravis is the electrical stimulation of individual nerves. The response of the muscles is recorded as in an electrocardiogram (ECG). In patients with myasthenia gravis, a characteristic drop, a so-called decrement, can be observed in the machine-generated curves, which, among other things, represent muscle activity.
In addition to the neurological examination in case of suspected myasthenia gravis also a laboratory analysis is useful. The antibodies specific for the disease can be detected in a blood sample (acetylcholine receptor antibodies or anti-MuSK antibodies). Since a blood test is not always reliable, a laboratory examination of muscle tissue is also performed.
In addition, the function of the chewing and pharyngeal muscles can be assessed by experienced speech therapists and thus the degree of myasthenia gravis can be better estimated.
In order to determine or investigate the cause of myasthenia gravis, in many cases a computed tomography (CT) is performed, in which the thymus is examined more closely. Both an over-productive thymus and a tumor in the thymus were detected on CT images.
Myasthenia gravis: treatment
Myasthenia gravis therapy is purely symptomatic, meaning it relieves the symptoms but can not stop the disease. A cure is not possible.
Myasthenia gravis: drug therapy
The symptoms of Myasthenia Gravis can be treated with medication. In most cases it is necessary to take the medication for a lifetime. There are three different therapy options to choose from, depending on the stage of myasthenia gravis:
1. Acetylcholinesterase inhibitor:
Acetylcholinesterase inhibitors improve signal transmission. As a result, the weakness of the muscles is usually reversed. It is often reported that the muscles of the extremities respond better to this therapy than the muscles on the face. Most of the active ingredient pyridostigmine bromide is used, which can be taken orally. In severe cases or with proven intolerance neostigmine or pyridostigmine are used, which are given directly into the vein (intravenous, i.v.).
2. Immunosuppressive treatment:
Glucocorticoids or azathioprine weaken the antibodies specific for myasthenia gravis and thus reduce the symptoms.
3. Plasmapheresis or high-dose immunoglobulin administration:
This treatment option is only used in severe cases or in impairment of the respiratory and pharyngeal muscles.
Myasthenia gravis: Further therapeutic measures
With a trained speech therapist a special swallowing therapy can be carried out. As a precaution, patients with moderate myasthenia gravis should only take food that is liquid and can not be easily swallowed. In severe cases, an artificial feeding via a nasogastric tube as well as mechanical ventilation and regular aspiration of the saliva may be necessary.
Double images can be well compensated by a customized prism glass.
In patients between 15 and 50 years of age, removal of the thymus is recommended as early as possible after diagnosis. In children up to 15 years, the thymus should be removed only if no improvement is achieved with a drug therapy, since the thymus still performs important functions in childhood.
Myasthenia gravis: disease course and prognosis
There is no general prognosis, as every person with myasthenia gravis has symptoms that vary in severity, in different places and in different ways.
The majority of patients with myasthenia gravis discovered and treated respond well to therapy. The symptoms are alleviated and, in most cases, normal day-to-day life can be resumed with only minor restrictions. The symptoms of Myasthenia gravis are also never continuous, so that affected people feel on some days, no impairments and are subject to other very severe restrictions.
If left untreated, symptoms of myasthenia gravis continue to develop and severe complications may occur. In extreme cases, when the respiratory muscles fail, this can be deadly. In other cases lifelong mechanical ventilation is necessary. There is more attention these days Myasthenia gravis and symptoms are often recognized early on, such severe courses have become less common.