Meningitis is an inflammation of the meninges. Most commonly, it is triggered by viruses. Rare, but much more dangerous is a meningitis caused by bacteria. It needs to be treated as soon as possible! Bacterial meningitis can develop into a life-threatening emergency within just a few hours. Read all important information about meningitis: symptoms, causes, diagnosis, treatment and prognosis!

Quick Overview
- What is meningitis? An inflammation of the skins that surround the brain – not to be confused with encephalitis. Both inflammations can occur simultaneously (as meningoencephalitis).
- Causes: Most viruses (TBE viruses, coxsackie viruses, herpes viruses, etc.) or bacteria (pneumococci, meningococci, etc.). Rarely are other pathogens (such as fungi, protozoa), cancers or inflammatory diseases (such as sarcoidosis) the cause of meningitis.
- Signs & Symptoms: flu-like symptoms (such as high fever, headache and body aches, nausea and vomiting), painful neck stiffness, sensitivity to light and light, possibly clouding of consciousness, loss of consciousness, possibly neurological deficits (such as speech and walking disorders) as well as epileptic seizures.
- Diagnosis: Medical history (medical history), physical examination, blood test, removal and analysis of nerve water (CSF), computed tomography (CT), magnetic resonance imaging (MRI)
- Treatment: For bacterial meningitis antibiotics and possibly dexamthesone (a cortisone). In viral meningitis symptomatic treatment (fever and pain medication) and possibly viral drugs (antivirals).
- Forecast: Left untreated, meningitis can become life-threatening within hours, especially bacterial meningitis. But if treated early, it can often be cured. However, some patients suffer permanent damage (such as hearing impairment).
Meningitis: symptoms
In general, the onset of meningitis produces symptoms similar to those of influenza. These include, for example high fever, headache and body aches, nausea and vomiting.
In the further course, one joins painful neck stiffness (Menigismus) added. It is a very typical meningitis symptom: The meninges are (unlike the brain) equipped with pain receptors. Inflammation and irritation, such as meningitis, are therefore painful. In addition, the neck stiffens. The pain is particularly noticeable in head movements, because the brain and spinal cord skins are stretched slightly. It hurts most when the chin is led to the chest. The pain also makes the neck muscles tense. This reinforces the neck stiffness.
Cerebral membranes and the brain itself can also be inflamed simultaneously. This combination of meningitis (meningitis) and encephalitis (encephalitis) is called meningoencephalitis.
The following is an overview of all major meningitis symptoms in adults:
|
Meningitis: symptoms in adults |
|
painful neck stiffness (meningism) |
|
fever |
|
a headache |
|
pronounced malaise with body aches |
|
increased photosensitivity of the eyes (photophobia, photophobia) |
|
increased noise sensitivity (phonophobia) |
|
Nausea and vomiting |
|
back pain |
|
Confusion and dizziness |
|
possibly dizziness, hearing disorders, epileptic seizures |
Meningitis: Symptoms of bacterial meningitis
Meningitis symptoms are especially severe in bacterial meningitis: Within hours, the initial mild symptoms can worsen massively and even lead to death! Therefore, it is vital to recognize the signs of bacterial meningitis early and to alert the doctor.
The first symptoms of meningitis show up here two to five days (in meningococcal about two to ten days), after getting infected with the bacteria. It starts as with other forms of meningitis unspecific, flu-like complaints, Over the course of hours or a few days, a highly acute clinical picture can develop. The victims usually have severe headache, extreme neck stiffness and fever, Also neurological deficits are possible, for example, a consciousness cloudiness and slurred speech.
complications
One possible complication of meningococcal meningitis is “septicemia” (sepsis): the bacteria overwhelm the patient’s blood in large numbers. In severe cases, this can be Meningococcal sepsis (Meningitis sepsis) the so-called Waterhouse-Friderichsen syndrome develop (especially in children and people without spleen):
The meningococci carry on their surface harmful sugar chains (endotoxins). When the bacteria disintegrate, these toxins are released into the blood in large quantities. This triggers an uncontrolled blood clotting reaction in the body: it forms numerous clots (Thrombi) that can clog smaller vessels. In addition, due to the massive clot formation necessary for the blood clotting Coagulation factors used up (DIC). That can heavy bleeding in the skin, mucous membranes and internal organs.
For example, initially small bleedings in the skin and mucous membranes, so-called petechiae, develop. They first show up only as about pin-sized, red or brownish dots. These get bigger and bigger and look like “bruises”. Hemorrhages in internal organs also occur, for example in the adrenal glands. They are severely damaged by this, so they fail as a hormone producer. Doctors then speak of one Adrenal Fatigue (Adrenal insufficiency). The heavy bleeding drops the blood pressure, it can develop a shock state up to a coma. The mortality rate in Waterhouse-Friderichsen syndrome is high!
Waterhouse-Friderichsen syndrome can occur in a variety of bacterial diseases. Most commonly, however, it is the result of meningococcal-induced meningitis.
Meningitis: Symptoms of viral meningitis
Virus-induced meningitis occurs generally milder as a bacterial meningitis. Signs first appear about two to fourteen days after infection: flu-like symptoms, followed by painful neck stiffness. In contrast to bacterial meningitis, the symptoms usually do not increase within hours, but rather over several days.
For people with a healthy immune system, the symptoms usually resolve themselves within a few days. The recovery phase can take quite a while. In smaller children, the disease can also be difficult. The same applies to people with weakened immune systems (for example, medications, cancer, or infections such as HIV).
Meningitis: Symptoms in infants and toddlers
Many infants and toddlers show very unspecific meningitis symptoms, The meningitis is then often difficult to diagnose, especially in the early stages of the disease.
First signs of meningitis in infants and toddlers include fever, drinking weakness and noticeable tiredness. The little patients are unusually irritable and listless. Later, abdominal pain, seizures and shrill screaming may be added. The fontanelle (bony gap in the child’s skull, which is covered with connective tissue and skin) may be bulging. The painful neck stiffness (meningism), which is usually a typical sign of meningitis, is often absent in infants and babies.
Tip: Since the meningitis symptoms can develop rapidly and become dangerous especially in small children, you should already go to the doctor for a vague suspected illness.
Meningitis: Symptoms of special forms of meningitis
Among the special forms of meningitis include the tuberculous meningitis (by tuberculosis bacteria) and one Meningitis in neuroborreliosis (by Lyme disease bacteria). Both start slowly – over days, fever can be the only meningitis symptom. Later, other signs of meningitis may be added, such as neck stiffness and headaches.
Overall, these two special forms are very rare. However, they should be considered in the case of a long-lasting disease course.
Meningitis: causes and risk factors
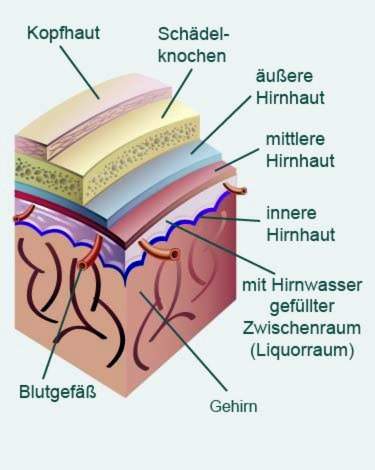
In meningitis, the meninges (meninges) are inflamed. These are connective tissue sheaths that rest against the brain within the skull. There are three pieces of it (inner, middle and outer meninges).
The causes of such meningitis can be quite different: First, meningitis can be caused by a variety of pathogens (Viruses, bacteria, fungi, etc.) are caused. Such pathogens can be transferred to other people with varying degrees of ease, depending on the species. This is why pathogen induced by meningitis contagious.
On the other hand, meningitis can also in the context of various diseases arise, for example in sarcoidosis or cancer. In these cases, meningitis is non-infectious, Read more about the possible meningitis causes below.
Non-bacterial meningitis is also referred to as aseptic meningitis (abacterial meningitis).
Viral meningitis
Viral meningitis is the most common form of meningitis. The most important triggering viruses are:
|
virus |
Diseases primarily caused by the virus |
|
|
Coxsackie virus A and B |
Hand-foot-and-mouth disease, Herpangina, summer flu |
|
|
Herpes simplex virus type 1 and 2 (HSV-1, HSV-2) |
Cold sores, genital herpes |
|
|
TBE virus |
Tick-borne encephalitis |
|
|
Varicella zoster virus (VZV) |
Chickenpox and shingles |
|
|
Epstein Barr virus (EBV) |
Pfeiffer glandular fever (Infectious mononucleosis) |
|
|
Mumps virus |
Mumps (goat peter) |
|
|
Measles virus |
measles |
|
|
Many more viruses: HI virus (HIV), polio virus, rubella virus, parvo B19 virus, etc. |
||
The Type of infection depends on the virus type. Coxsackie viruses, for example, can be transmitted by droplet infection: Patients can distribute tiny saliva droplets in the ambient air during coughing, sneezing and speaking. The droplets contain cosackie viruses. If they are inhaled by a healthy person, they can also become infected. In the process, coxsackie viruses primarily trigger other illnesses, such as a summer flu or herpangina. In the context of this primary disease, the viruses can spread to the meninges and cause meningitis.
In another way, the meningitis infection takes place, for example, in TBE viruses: The pathogens are transmitted by the bite of blood-sucking ticks.
It also depends on the type of virus, how much time passes between the infection and the onset of the first disease symptoms (incubation period). In general, the meningitis incubation period is usually about two to fourteen days.
Bacterial meningitis
Bacterial meningitis is less common than viral meningitis but is often severe. The most common pathogens of bacterial meningitis are the so-called pneumococcal (Streptococcus pneumoniae). The meningitis is then referred to as pneumococcal meningitis. However, pneumococci can also cause other diseases, such as pneumonia, otitis media and sinusitis.
Another common cause of bacterial meningitis are meningococcal (Neisseria meningitidis). Meningococcal meningitis is very dangerous. In fact, within a few hours it can lead to “blood poisoning” (meningococcal sepsis) and further to Waterhouse-Friderichsen syndrome. Then there is a great danger to your life!
Pneumococci and meningococci are the main causes of bacterial meningitis. But there are many other bacteria as polluters in question:
|
bacterium |
caused diseases |
|
|
pneumococcal |
V. A. Meningitis, pneumonia, middle ear and sinusitis etc. |
|
|
meningococcal |
V. A. Meningitis and blood poisoning (sepsis) |
|
|
staphylococci |
Meningitis, food poisoning, wound infections, sepsis, etc. |
|
|
Enterobacteria incl. Pseudomonas aeruginosa |
Diarrhea, intestinal inflammation, pneumonia, meningitis etc. |
|
|
Haemophilus influenzae type B |
Meningitis, pneumonia, sepsis, heart muscle inflammation (myocarditis) |
|
|
Streptococcus agalactiae (B streptococci) |
Meningitis, sepsis, urinary tract infections, wound infections |
|
|
Listeria monocytogenes |
“Listeriosis” (diarrhea and vomiting, blood poisoning, meningitis, encephalitis, etc.) |
|
The different bacteria are depending on their age, the cause of meningitis differently. For example, infantile meningitis is often caused by Streptococcus agalactiae, Listeria monocytogenes or E. coli (one of the enterobacteria). In infants meningococci, pneumococci and haemophilus influenzae type B are the most common causes. Meningitis in adults is most commonly caused by pneumococci or meningococci.
It also depends on the causative bacterium how meningitis transmission occurs (usually droplet infection).
Other meningitis causes
Viruses and bacteria are responsible for the majority of meningitis. Meningitis rarely has a different cause. This is often the case with people whose immune system is weakened by another disease (such as HIV or cancer) or medications (immunosuppressants). The following is an overview of other triggers of meningitis (besides viruses and bacteria):
|
Other causes of meningitis |
|
Special bacteria: Tuberculosis (tuberculous meningitis), neuroborreliosis |
|
Fungal infection: Candidosis, cryptococcosis, aspergillosis |
|
parasites: Echinococcosis (tapeworm) |
|
Protozoa (Protozoa): toxoplasmosis |
|
Cancers: Meningeosis carcinomatosa, Meningeosis leucaemica |
|
Inflammatory diseases: Sarcoidosis, lupus erythematosus, Behçet’s disease |
Meningitis: examinations and diagnosis
If you suspect meningitis you should not lose time. You need to see a doctor without delay! Contact the family doctor, a pediatrician (in small patients), a neurologist or the emergency department of a hospital. Diagnosing and treating meningitis quickly can be life-saving!
An experienced doctor can already diagnose the meningitis based on the symptoms and the physical examination. However, it is important to clarify whether it is a bacterial or viral meningitis. That depends on the treatment.
The most important steps to meningitis diagnosis are:
Medical history (anamnesis)
In conversation, the doctor will first raise your medical history or that of your sick child (anamnesis). Possible questions of the doctor are:
- Is there currently a cold (sore throat, cough, chronic cold)?
- Do you have a headache, fever, and / or a painful neck stiffness?
- Are any underlying or pre-existing conditions known (HIV, sarcoidosis, Lyme disease, etc.)?
- Are your children taking or taking medication on a regular basis?
- Do you or does your child have an allergy to medication (for example, to antibiotics)?
- Did you or did your child have contact with other people with headaches, fever and neck stiffness?
- Were you or was your child recently abroad (for example in an African country)?
Physical examination
At the physical examination, the doctor will first check the classic signs of meningitis. For this purpose, he tries to guide the head of the patient lying on his back with his chin to the chest. This can be a painful neck stiffness (meningism) notice. In addition, the patients typically reflexively pull on the legs at this head tilt (Brudziński’s sign) – an involuntary reaction to the pain caused by the slight stretching of the cerebral and spinal cord skins during head tilt. The Brudzinski sign is a good indication of meningitis).
Another sign of meningitis is when the sick person can not straighten his leg while seated because it is too painful (Pithy characters).
Also the so-called Lasègue characters can be conspicuous in meningitis: The doctor moves the lying patient each one stretched leg slowly upwards – so he performs a hip joint flexion with a straight knee. If the patient feels pain from the back of the leg (positive Lasègue sign), this indicates irritation of the brain’s lining.
The Lasègue sign is also positive for a herniated disc.
Very important is also the exact examination of the entire skin of the patient. In severe bacterial meningitis, small Bleeding on the skin (petechiae) occur. They are an alarm signal for the doctor! He will immediately initiate further investigations and treatment. The bleeding initially looks like little blue or brownish dots. These become larger patches in the course and typically can not be pushed away with a transparent object (glass) (Glass test).
Further investigations
By the anamnesis interview and the physical examination, the doctor can already estimate well whether meningitis requiring treatment is present. If there is even the slightest indication that it is actually a meningitis, the physician will initiate further investigations. For example, if you were initially at the family doctor or pediatrician, you will usually be forwarded directly to a clinic. Because of the possible serious complications of meningitis, further examinations and treatment should be better done in the hospital.
The first steps of further investigations in case of suspected meningitis are:
1. Decrease of blood for blood cultures: Through so-called blood cultures, one can try to detect and identify a pathogen – especially bacteria. The physician may then select for bacterial meningitis therapy a suitable antibiotic effective against the particular type of bacteria.
2. removal of nerve water (CSF): In the CSF function, a small hollow needle is used to remove some nerve water (cerebrospinal fluid) from the spinal canal at the level of the lumbar vertebrae. The whole thing takes only a few minutes and is usually perceived as not particularly painful. The CSF sample is examined in the laboratory for possible pathogens of meningitis. If necessary, a computed tomography (CT) is performed before the CSF function in order to rule out an increased intracranial pressure. With increased intracranial pressure, CSF should not be performed.
3. Computed Tomography (CT) or Magnetic resonance imaging (magnetic resonance imaging, MRI): These imaging techniques provide more information about the condition of the brain. Sometimes they can also give clues as to where the pathogen originally came from (for example, from suppurated sinuses).
Meningitis: treatment
If meningitis is suspected, a rapid start of treatment may be crucial for the prognosis. Since it is difficult to foresee how the disease develops, it should in any case in the hospital be treated. The most suitable is a hospital with a neurological department.
As soon as blood and nerve water have been removed, the doctor starts one antibiotic therapy – even if you do not even know if there actually is a bacterial meningitis. With the early antibiotics you play it safe, because a bacterial meningitis can quickly become very dangerous.
The doctor sets for the treatment Broad-spectrum antibiotics (Ceftriaxone, ampicillin etc.). These antibiotics are effective against many bacteria simultaneously, including those most commonly responsible for bacterial meningitis. As a rule, the antibiotics are administered as an infusion directly into a vein. So they can quickly develop their effect.
As soon as the actual pathogen has been determined on the basis of the blood and nerve water sample, the doctor adjusts the meningitis treatment accordingly: If it is indeed a bacterial meningitis, the patient may be switched to other antibiotics that better and more targeted fight the causative bacterium , But if it turns out that a virus is responsible for meningitis, usually only the symptoms are treated.
Bacterial meningitis: therapy
The one described above antibiotic therapy can fight the cause of bacterial meningitis. In addition, sometimes that is Glucocorticoid (“Cortisone”) Dexamethasone given. It has an anti-inflammatory effect. This can, for example, lower mortality from pneumococcal meningitis. In addition, combined treatment with antibiotics and dexamethasone may reduce the incidence of severe hearing loss in Haemophilus influenzae meningitis.
Should be the dreaded Waterhouse-Friderichsen syndrome develop, treatment in intensive care is necessary.
Special measures for meningococcal meningitis
To reduce the risk of infection for others, the patient is placed in a single room and isolated from other patients. Contact persons the patient may receive preventively an antibioticFor example, rifampicin in tablet form: This is necessary in all people who had close contact with the patient (family members, work colleagues, classmates, etc.) about seven days before to ten days after onset of disease. Maybe there is one too Meningococcal vaccine for the contact persons useful if they have not already been vaccinated as a child.
Viral meningitis: therapy
In viral meningitis usually only the symptoms are treated. Only against a few viruses, there are special drugs (antivirals) that can mitigate the disease. This applies for example to the group of herpesviruses (herpes simplex virus, varicella-zoster virus, Epstein-Barr virus, cytomegalovirus) and HIV (HIV).
In principle, viral meningitis is primarily about alleviating symptoms. Bed rest as well as antipyretic and analgesic medications help. It may also be necessary to prevent an epileptic seizure by medication. If the condition is favorable, the patient can usually be discharged soon and treated at home.
Meningitis of other cause: therapy
If meningitis has causes other than bacteria or viruses, the trigger will be treated as appropriate. For example, fungal infections (antifungals) are prescribed for fungal meningitis. Worm remedies (antihelmonthics) are used against tapeworms. If a sarcoidosis, cancer or other underlying disease is behind the meningitis, it will be targeted.
Meningitis: disease course and prognosis
Meningitis is a potentially life-threatening disease. Among other things, the prognosis depends on which pathogen causes meningitis and how quickly the patient is treated properly.
Especially the Bacterial meningitis is an emergencywho needs to be treated with antibiotics as quickly as possible. If left untreated, it practically always ends fatally. With timely treatment, but the prospect is good that the patient is completely recovered. The chances of a full recovery depend on the exact type of pathogen and the general health of the patient. For example, the prognosis is less favorable for infants, and sometimes for seniors, because their immune system is often not as efficient as a healthy adult.
A viral meningitis is usually much less life threatening than bacterial meningitis. But here, too, the prognosis depends on the particular virus and on the general physical condition. Especially the first days are critical. If the person has survived this well, the chances of recovery are usually good. Viral meningitis usually heals within several weeks without any sequelae.
Meningitis: episodes
In some cases, meningitis permanent neurological damage entail. These include hearing damage, paralysis or impairment of the psyche or behavior. Complications and long-term damage are more likely to occur when the inflammation also spreads to the brain (meningoencephalitis).
Meningitis: Prevention
If you want to prevent meningitis, you should, if possible, above all protect against infections with the most common pathogens (viruses and bacteria).
Bacterial meningitis: Prevention through vaccination
The Standing Vaccination Commission at the Robert Koch Institute (RKI) recommends different vaccinations for all children. These include three vaccinations against common bacterial meningitis pathogens: meningococcal vaccine, pneumococcal vaccine and Haemophilus influenzae type B vaccine. The immune system of young children is not yet mature and therefore can not ward off pathogens so well. Therefore, these three vaccinations significantly reduce the risk of bacterial meningitis:
Meningococcal vaccination
There are several subgroups (serogroups) of meningococci. In Europe, meningococcal meningitis is usually triggered by serogroups B and C.
A Meningitis caused by meningococci C is less common, but often severe and has complications (such as the Waterhouse-Friderichsen syndrome). All children in the second year of life should therefore be vaccinated against meningococcal C. If this vaccination date missed, the vaccination should be made up to the age of 18 years.
Against the much more common Meningococcal meningitis B there is a brand new vaccine since the end of 2013. In infants, it is given in four doses. For older children, two doses are sufficient. So far, STIKO does not have enough data to recommend this vaccine for all children. Currently, the Meningokokken B vaccine will therefore only people with certain underlying diseases advised – in addition to the combined Vaccination against meningococci A, C, W and Y, These include, for example, people with a congenital or acquired immune deficiency (such as in the absence of spleen) and endangered laboratory personnel. The same applies to unvaccinated people living in the same household as patients living through a severe infection with one of the meningococcal serogroups (A, B, C, W or Y).
Pneumococcal vaccine
The pneumococcal vaccine is recommended to all children. Three doses of vaccine are planned: the first dose should be given at the age of two months, the second dose at the age of four months. The three dose dose should be given half a year later, between the ages of 11 and 14 months.
Haemophilus influenzae type B vaccine
The Hib vaccine is also recommended for all children. It is given in four doses – one dose from the 2nd month of life, the 3rd month of life, the 4th month of life and the end of the first year of life (11th to 14th month).
Viral meningitis: Prevention by vaccination
Some forms of viral meningitis can also be prevented by vaccination. By default recommended for all children are the mumps vaccine, measles vaccine and rubella vaccine (mostly combined as MMR vaccination administered).
There is also a Vaccine against tick-borne encephalitis (TBE). This is a tick-borne viral inflammation of the meninges and brain. The STIKO recommends the TBE vaccination to all people living or staying in TBE risk areas (such as on vacation) and could be stung by ticks (by frequent or long stays in nature).
For a longer vaccine protection a primary immunization with three vaccine doses is recommended. After three years, the TBE vaccine can be refreshed with another dose. Thereafter, booster creams at five-year intervals are recommended if one continues to use a combined one meningitis and to prevent encephalitis caused by TBE viruses.
Additional information
guidelines:
- Guideline “Viral meningoencephalitis” of the German Society of Neurology (2015)
- Guideline “Outpatient acquired bacterial (purulent) meningoencephalitis in adulthood” of the German Society of Neurology (2015)