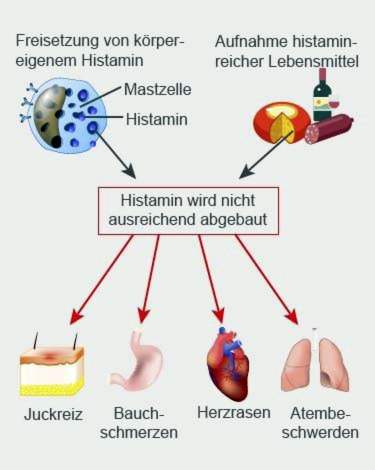
In the case of histamine intolerance, the body reacts to an increased amount of histamine with intolerance reactions. This substance occurs naturally in the body, but is also found in many foods. Possible symptoms of histamine intolerance include wheals on the skin, itching, headache and gastrointestinal discomfort. Mostly women are affected in middle age. Read all about histamine intolerance.

Quick Overview
- What is histamine intolerance? Incompatibility with larger amounts of histamine. Histamine is a tissue hormone and messenger that occurs naturally in the body. He is also in many foods. Histamine intolerance (HI, histaminosis), however, is a controversial issue among experts.
- symptoms: very diverse, e.g. Flushing with flushing sensation, itching, hives (urticaria), palpitations, headache, stuffy or runny nose, asthma, diarrhea, abdominal pain
- Causes: Experts suspect that an affected or (more rarely) congenital disorder of histamine degradation in the body.
- investigations: Doctor-patient interview to collect the medical history (anamnesis), investigations to rule out other possible causes of the complaints, three-stage diet change, possibly a provocation test
- Treatment: adapted diet, possibly enzyme preparations
Histamine intolerance: symptoms
Histamine intolerance symptoms are very diverse. Some patients only show individual complaints (such as redness with itching). Others, on the other hand, have histaminosis with symptoms in several parts of the body. This is because the most diverse cells and organs have docking sites (receptors) for histamine. These include, for example, smooth muscle cells (in the stomach and intestinal wall, in the bronchi and uterus, in the blood vessel walls, etc.), glandular cells, nerve cells and cells of the immune system (such as mast cells).
Histamine mediates its action by binding to these receptors. With a high amount of histamine, the receptors are activated nonstop. Depending on where in the body they are, this results in sensitive people a variety of histamine intolerance symptoms.
Histamine intolerance symptoms: skin
Histamine can activate so-called mast cells in the skin. These then release allergenic ingredients that can cause various skin symptoms:
- urticaria (Hives): It is characterized by small, fleeting swellings of the skin (wheals), which usually stand together beetartig. The skin usually appears red or white with a red border at the affected areas. The wheals may appear distributed throughout the body. They usually disappear after 24 hours. As long as the trigger of hives but continues to exist, can always form new wheals.
- Itching: The substances released from the mast cells trigger not only urticaria but also a massive itching. Especially the skin over the wheals is very irritated. Unlike other itchy skin diseases, however, wheals are not scratched, just rubbed and pressed.
Histamine intolerance symptoms of the skin also show in an increased blood circulation: histamine leads to a release of nitric oxide, which broadens the blood vessels. This allows more blood to flow through. This causes the affected Skin areas reddened and warmed, If this phenomenon occurs in the face, it is also called flush designated.
Histamine intolerance symptoms: brain
Also in the brain, histamine via the release of nitric oxide can cause the blood vessels to dilate. If this happens in the arteries of the meninges, headaches can occur. This mechanism is also discussed in migraine.
Other potential symptoms of histamine intolerance that may be from the head include dizziness, nausea, and vomiting. Some patients also report decreased attention and fatigue.
Histamine intolerance symptoms: cardiovascular system
If histamine changes the vessel width of the coronary blood vessels (coronary vessels), palpitations and heart stuttering (extrasystoles) may occur. These are usually harmless cardiac arrhythmias. Some patients also report noticeable palpitations.
If the blood vessels in the body periphery expand, the blood pressure can drop. In extreme cases (with very high amounts of histamine), the blood in the legs can sag, so that not enough is transported back to the heart: the blood pressure drops dramatically, shock symptoms can occur. But that rarely happens.
Histamine intolerance symptoms: gastrointestinal tract
In the stomach, histamine increases gastric acid production. Also, the muscle cells in the wall of the gastrointestinal tract are more activated by histamine. Therefore, abdominal pain or cramping, diarrhea and flatulence are common histamine intolerance symptoms in the digestive tract. They occur mainly in the intake of histamine-rich foods and drinks.
Histamine intolerance symptoms: genital tract
In women, histamine is produced in, among other things, the uterus and the ovaries. It aims to increase the concentration of the female sex hormone estrogen. This hormone causes the uterus to contract painfully during the menstrual period. This means: Histamine can be partly responsible for menstrual problems such as menstrual pain.
In contrast, hormone fluctuations in pregnancy can have a positive effect on women with histamine intolerance: often histamine-related symptoms then disappear.
Histamine intolerance symptoms: respiratory tract
During or immediately after eating high-histamine meal or drinking alcohol, patients with histamine intolerance may develop symptoms such as a runny or stuffy nose. In extreme cases, an asthma attack with severe respiratory distress may occur.
In patients with asthma, moreover, less histamine is often broken down by a given enzyme than in healthy people. As a result, histamine also increasingly accumulates in the bronchi, independent of food intake. This can trigger corresponding complaints.
Histamine intolerance: description and causes
In histamine intolerance (HI), the body reacts Incompatible with increased levels of histamine, This so-called biogenic amine is formed in various cells such as mast cells, platelets and nerve cells from the protein (amino acid) histidine and then stored in these cells. Certain stimuli can release histamine, for example, through the body’s own enzymes, various medicines and foods. Also, chemical stimuli in the context of inflammation and physical stimuli such as injury or lack of oxygen can stimulate a release of histamine.
Histamine exercises as biological messenger different functions in the body. For example, it stimulates gastric juice secretion, dilates blood vessels and lowers blood pressure. As a nerve messenger (neurotransmitter), histamine regulates, among other things, the sleep-wake cycle, the appetite control, the learning ability, the memory and the emotions.
Above all, however, histamine acts as a Mediator of inflammatory processes in allergic reactions: It triggers the typical allergy symptoms such as redness, wheal, itching, malaise, vomiting, diarrhea, asthma attacks and headaches. These symptoms may also occur with histamine intolerance. Nevertheless, it is about no histamine allergyThat is, the HI symptoms are not triggered by an overreaction of the immune system to histamine.
Instead, experts suspect that an acquired or (more rarely) congenital Disorder in histamine degradation the histamine intolerance triggers. In the body of the affected then falls through the body’s own production and / or histamine-rich food more histamine than can be broken down. Once a certain limit is exceeded, it comes to complaints. How high this histamine threshold is is individually different.
Disturbed histamine degradation
Basically, the body has two different enzymes that can break down histamine:
- The enzyme Histamine N-methyl transferase is located inside the cell and can therefore inactivate histamine in the cells.
- The Diaminooxidase (DAO) can break down histamine, which is outside the cells – for example, in the blood.
The DAO is thus responsible for the degradation of histamine from food. It therefore plays a central role in histamine intolerance: in some patients, the enzyme may be present in an inadequate amount (enzyme deficiency). For others, it may be less active (disturbed enzyme function). Since DAO requires auxiliaries such as vitamin B6 and vitamin C for histamine degradation, a deficiency of these vitamins can limit the function of the enzyme. But there are also drugs that affect the activity of diaminooxidase (see below).
Whether enzyme deficiency or impaired enzyme function – is the histamine turnover out of balance, develops in some people a histamine intolerance. In addition to histamine-rich foods and certain medications can also be a increased endogenous histamine production in allergic diseases How hay fever causes the symptoms: The allergic histamine increase in the body can exceed the enzymatic degradation capacity. This is especially true if the patient feeds histamine rich at the same time.
Histamine Intolerance: The Influence of Drugs
Histamine is produced as an endogenous messenger substance in different cells and stored. Under certain stimuli, it can be released from the cells and perform its functions. Such a stimulus can also emanate from some medications, that is: some medications promote histamine release, Most often, this effect occurs as an undesirable side effect.
In addition, certain medications can Affect degradation of histamine: Dietary histamine is degraded mainly by the enzyme diaminooxidase (DAO). This enzyme is also responsible for the degradation of other metabolites. If drug treatment causes more of these products, the enzyme may release less histamine. As a result, the histamine concentration increases.
Other drugs directly inhibit the function of diaminooxidase. This can also increase the histamine concentration and thus trigger discomfort of histamine intolerance.
Below are the most common medications which may result in increased release or decreased histamine depletion. If the triggering medication is discontinued, it is in many cases possible to “cure” histamine intolerance.
- all X-ray contrast agents
- certain muscle relaxants (muscle relaxants like suxamethonium)
- certain analgesics (acetylsalicylic acid, diclofenac, metamizole, morphine etc.)
- Prilocaine (local anesthetic)
- certain remedies for hypertension and heart diseases such as arrhythmias (dihydralazine, alprenolol, verapamil etc.)
- Furosemide (diuretic = diuretic)
- certain antibiotics (neomycin, vancomycin etc.)
- Metoclopramide (remedy for nausea and indigestion)
- certain mucus removers (acetylcysteine, ambroxol)
- certain remedies for asthma (aminophylline, theophylline)
- Amitriptyline (antidepressant)
- Cyclophosphamide (cancer and rheumatism)
- Cimetidine (remedy for heartburn and acid-related stomach discomfort)
Histamine Intolerance: Diet can trigger symptoms
Histamine and its precursors are present in almost all foods and in some beverages (see below: “Histamine Intolerance: Food”). However, the histamine content varies significantly and can be influenced by processing processes such as maturation or fermentation. Consuming histamine-rich foods increases the concentration of histamine in the body. If the histamine metabolism can not be increased accordingly, the histamine sales out of balance – complaints may occur.
Histamine intolerance: associated disorders
For some inflammatory bowel disease There may be a deficiency in the histamine-degrading enzyme diaminooxidase. As a result, less histamine can be degraded overall. This results in an increase in histamine concentration, which can cause symptoms of histamine intolerance.
In addition, there are other diseases associated with histaminosis. Even with them the enzyme diaminooxidase is reduced active. These diseases include:
- Chronic kidney failure
- virus-induced liver inflammation (viral hepatitis)
- cirrhosis
- Hives (urticaria)
- seasickness
Histamine Intolerance: Controversial Disease
Histamine intolerance is a very controversial disease: First, because the symptoms can vary considerably from patient to patient. On the other hand, because the different symptoms can also occur in many other diseases. Also, diagnostics often do not provide clear evidence of histaminosis. Therefore, some doctors reject the clinical picture of histamine intolerance. Others, however, are convinced that it exists.
Experts suggest that about one percent of the German population suffers from histamine intolerance. 80 percent of those affected are women. The middle age is considered the most common disease onset in histamine intolerance.
Histamine intolerance: examinations and diagnosis
Many patients with histamine intolerance have already had many visits to the doctor, in which a cause for their symptoms could never be found. Often the symptoms are nonspecific, and examination results are not pathological findings. A histamine intolerance diagnosis is a doctor usually only if he has this disease in mind. Targeted questions or a histamine intolerance test confirm the hypothesis.
Doctor-patient conversation
The right contact for suspected histamine intolerance is a specialist in dermatology (dermatologist) or internal medicine (internist), who specializes in allergic diseases (allergist). He first raises your medical history (anamnesis). For this he asks, for example, about your current complaints and any pre-existing conditions. Possible questions include:
- Do you suffer from allergic diseases or food intolerances?
- Have you discovered a connection between your symptoms and the consumption of certain foods or are you keeping a food diary?
- Do the symptoms improve if you do without these foods?
- Do you take medications regularly or as needed?
- In women: Are your symptoms related to your cycle?
Exclusion of other causes
The symptoms that occur with histamine intolerance may also have other causes (differential diagnosis). For example, those who often have abdominal pain and maybe even diarrhea after eating may be suffering from one Food intolerance (such as lactose intolerance, fructose intolerance, celiac disease). Also one chronic inflammatory bowel disease such as Crohn’s disease or ulcerative colitis may be behind it. Nausea and vomiting associated with a meal may also occur at one time Ulcer of the gastric mucosa (Stomach ulcer) occur. A facial flush with flushing (flushing) may be the sign of a neuroendocrine tumor be.
If histamine intolerance is suspected, the physician must rule out such differential diagnoses. Which examinations are necessary depends on the symptoms. For example, gastric ulcer can be reliably detected or excluded with gastroscopy.
Histamine intolerance: diet change test
With the help of a food test one can detect a possible histamine intolerance. At the same time, the individually tolerable histamine dose can be estimated for each patient.
This dietary change histamine intolerance test consists of three phases: the qualifying phase, the test phase and the long-term diet. In addition to nutrition, individual factors influencing histamine levels such as stress, the use of certain medications and hormone status (menstruation) are taken into account in all phases.
Grace period: In this first phase of the diet change, the symptoms are to be reduced as much as possible. The patient should do this for 10 to 14 days preferably no histamine to absorb with food. A completely histamine-free diet is hardly possible because histamine is contained in many foods. A special grocery list, however, helps the patient to design his diet so that he consumes as little histamine as possible.
In addition, the diet should also as few other biogenic amines as possible include. These are also decomposed by the histamine-degrading enzyme diamine oxidase (DAO). In larger quantities they can therefore “employ” the enzyme so that even small amounts of histamine can no longer be broken down. In addition, some biogenic amines may have a histamine-like effect (dilation of the blood vessels) – another reason to keep their nutritional low in the provocation test.
Test phase: This second test phase lasts up to six weeks. During this time, deliberately “suspicious” foods are slowly being reintegrated into the diet. Starting with a small amount of histamine, the histamine content of the diet is gradually increased. In parallel, the patient notes in a food diary, which foods he has taken on each day and whether complaints have occurred. Thus, it can be estimated from which individual histamine threshold signs of disease occur.
Permanent line: From the findings of the test phase, the doctor can derive individual nutritional recommendations for the patient. These are suitable for a permanent diet. In addition to the individually tolerable amount of histamine, the doctor also takes into account the energy requirements of the patient and influencing factors such as hormone levels, medication intake or stress.
Histamine intolerance test: provocation
With the diet change described above can estimate how much histamine tolerates someone. This is often enough to shape the diet accordingly. If you want to know exactly from which amount someone develops histamine intolerance symptoms, you can perform a “titrated provocation”. For this provocation test, the patient should first eat some histamine-free diet for a while and currently have no symptoms. The doctor then administers increasing amounts of histamine (for ingestion) every two hours. The dose at which histamine intolerance symptoms appear is then considered as an individual threshold dose.
The provocation test must be performed under medical supervision. If violent intolerance reactions such as nausea and vomiting to temporary circulatory disorders occur, the doctor can treat them quickly.
Further histamine intolerance tests
Often, other histamine intolerance tests are recommended to safely detect histamine intolerance. The validity of such investigations is limited. They include:
- Measurement of DAO activity in blood serum: One possible cause of histamine intolerance (HI) is decreased activity of the histamine-degrading enzyme diaminooxidase (DAO). In the affected patients, therefore, the DAO activity in the blood serum should be measurably reduced. However, according to experts, this procedure is not meaningful enough to make a histamine intolerance diagnosis.
- Measurement of the amount of histamine in the blood plasma: It should also be suitable as a histamine intolerance test. The validity of this study is disputed among experts. Conspicuous readings – in addition to histaminosis – can also have many other causes.
- Measurement of the amount of histamine in the stool: Sometimes a stool is offered in the stool in order to clarify the suspicion of histamine intolerance. However, various intestinal bacteria excrete large amounts of histamine in part. The measured values in the stool are therefore not very meaningful.
- Measurement of Methyl Histamine Amount in Urine: Methylhistamine is a breakdown product of histamine. Its concentration in the urine should give indications of a possible histamine intolerance. However, this reading generally depends on the protein content of the diet. Therefore, the determination of methyl histamine as a histamine intolerance test is controversial.
- Histamine 50-prick test: The prick test is a widespread allergy test. The suspected irritant – in this case the histamine – is scratched into the skin of the patient in dissolved form (as a drop). In case of intolerance, the skin reacts with the formation of wheals (skin blisters). If these are still present after 50 minutes, it is assumed that the breakdown of the histamine in the skin is disturbed. However, this does not mean that the body can not break down even through ingested histamine properly. Therefore, this histamine intolerance test is also critically considered by experts.
Conclusion
None of the currently available histamine intolerance tests can reliably prove whether someone can actually tolerate (from a certain amount) on externally supplied histamine and therefore react with complaints. Experts recommend that doctors diagnose histamine intolerance for the following diagnostic steps:
- Survey of the medical history in the doctor-patient interview (anamnesis)
- Investigations to exclude other possible causes of the symptoms such as gastrointestinal ulcer (for nausea / vomiting) or lactose intolerance or fructose intolerance (for abdominal pain, diarrhea)
- Histamine intolerance test using a three-stage diet change
- If the change in diet could actually alleviate the symptoms, a titrated provocation test may be performed to more accurately determine individual histamine tolerance
Histamine intolerance: treatment
The histamine intolerance therapy is mainly to avoid triggering factors. This succeeds above all with an adapted nutrition. If possible, patients should also refrain from medication that may trigger the discomfort of histamine intolerance. In certain cases, the use of certain medications may help with histamine intolerance symptoms (drug histamine intolerance therapy).
Diet with histamine intolerance
Foods high in histamine, such as aged cheese or cured meat, should not be consumed. In addition, people with histamine intolerance should avoid foods that can release histamine from cell stores (histamine liberators such as tomatoes or strawberries). Also unfavorable are foods that contain larger amounts of other biogenic amines (bananas, pineapples, peanuts, etc.).
In addition, with a histamine intolerance diet, caution should also be exercised when choosing drinks: Red wine in particular is unfavorable for histamine intolerance. Coffee, on the other hand, is usually well tolerated in small quantities of one to two cups a day.
Tip: For more on adverse foods in histaminosis, see Histamine Intolerance: Foods below.
How strictly affected must adhere to a histamine intolerance diet, can be determined in the context of diagnostics (three-stage diet change, possibly provocation test) or self-testing. Do not forget: The onset of discomfort depends on the total amount of histamine in the body – that is, the dietary histamine plus the histamine produced in the body. It is the individual histamine compatibility is not the same every day, It is influenced by various factors, such as the distance between meals, alcohol intake, medication, bowel disease or hormonal status (menstruation). This means that despite a consistently low-histamine diet, a patient may be symptom-free on one day and may be the next to struggle with symptoms such as wheals, itching, and headaches.
Histamine intolerance: discontinue or change medication
Many medications can trigger or worsen histamine intolerance. Patients should therefore discontinue such preparations if the treating physician deems this justifiable. Maybe he can recommend as an alternative another drug that is better tolerated.
Never discontinue medication on your own, but always in consultation with the attending physician!
Drug histamine intolerance therapy
Sometimes it is not possible to do without “critical” medications. This may be the case with X-ray contrast media in the context of examinations or muscle-relaxing means during operations. Then patients with histamine intolerance can prevent antihistamines (Histamine receptor blocker). These drugs block the docking points of histamine (histamine receptors). Thus, despite increased accumulating histamine in the body no or at least significantly less intolerance symptoms.
For existing histamine intolerance symptoms, antihistamines may also help.
Sometimes doctors use so-called histamine intolerance Mast cell stabilizers, They are used as antihistamines actually in allergies. Their effect is based on stabilizing the cell membrane of mast cells. As a result, they release less histamine (and other inflammatory messengers).
If there is a deficiency in the histamine-degrading enzyme diaminooxidase (DAO), it can be taken in capsule form. Such DAO preparations are available as a dietary supplement without prescription. They can be taken before a meal if it contains a lot of histamine or if you can not estimate its histamine content (eg when traveling or at family celebrations). If symptoms are already present, the enzyme preparation does not help anymore.
The said preparations for the prevention or alleviation of histamine intolerance symptoms are no longer a long-term replacement for a histamine-poor diet. They serve only as a supplement and should only be taken as needed! Patient and doctor should discuss together, if and which preparations are meaningful. Some of the medications (like antihistamines) are also available by prescription only.
vitamin supplements
Vitamin C and vitamin B6 are cofactors of diaminooxidase (DAO), which means that the two vitamins are important for the function of the enzyme. Therefore, the intake of appropriate vitamin supplements may be useful. Patients should discuss this with their attending physician. If necessary, he can recommend a suitable preparation and a suitable dosage.
Histamine intolerance: food
Foods that contain a lot of histamine and / or other biogenic amines should be avoided with histamine intolerance. Also unfavorable are products that stimulate the release of histamine from its storage cells. These three food groups should therefore know patients:
Histamine intolerance: foods high in histamine
Histamine or its precursor histidine are included in almost all foods. However, the respective histamine content differs significantly. It is enhanced by maturation, fermentation and fermentation processes. For example, old Gauda contains more histamine than young Gouda, smoked ham more than cooked. Many bacteria or yeasts are able to release histidine. In microbially produced foods such as long-matured cheese, wine or sauerkraut high histamine concentrations are therefore not uncommon.
In addition, many people with histamine intolerance do not tolerate foods such as fish, meat and sausage badly or not at all – in these products, microorganisms often accumulate. Last but not least, some vegetables naturally contain histamine, even when fresh – so they are also unfavorable for histamine intolerance.
A list of particularly histamine-rich foods can be found here:
- Fish: mackerel, herring, sardine, tuna
- Cheese: Gouda, Camembert, Cheddar, Emmentaler, Swisstaler, Parmesan
- Meat: sausage, salami, smoked ham
- Vegetables: sauerkraut, spinach, eggplant, tomatoes, avocado
- Alcohol: red wine, white wine, top and bottom fermented beer, champagne
- Others: red wine vinegar, soy sauce, yeast preparations
Histamine intolerance: food with other biogenic amines
In addition to histamine, other biogenic amines (such as tyramine, serotonin, spermine, cadaverine) are degraded via the enzyme diamine oxidase (DAO). Under certain circumstances, they “employ” the enzyme so much that even small amounts of histamine can no longer be broken down. A histamine overload can be the result. Some biogenic amines also have properties similar to histamine. So you can trigger directly histamine-like symptoms.
Rich biogenic amines contain, for example:
- Pineapple, bananas, papaya, pears, raspberries, oranges, kiwi
- peanuts
- Legumes (lentils, beans, soy)
- wheat germ
Histamine intolerance: foods that release histamine
So-called histamine liberators contain neither histamine nor other biogenic amines in larger quantities. But you can still trigger the symptoms of histamine intolerance. The reason: They ensure that the body’s own histamine from certain memory cells in the body (mast cells) is released. Therefore, they should also be avoided in case of histamine intolerance. The histamine liberators include:
- Citrus fruits, strawberries
- Tomatoes, tomato puree, ketchup, tomato juice
- Chocolate, cocoa
- Meeresfrüchte (Muscheln, Krebs)
- Nüsse (vor allem Walnüsse und Cashewnüsse)
- Alkohol und sein Abbauprodukt Acetylaldehyd
Ernährungstipps bei Histaminintoleranz
Lebensmittel der genannten kritischen Gruppen sollten Sie bei einer Histaminintoleranz möglichst selten auf Ihren Speiseplan setzen. Wer nicht komplett darauf verzichten will, sollte kritische Lebensmittel immer auf mehrere Mahlzeiten verteilen. Wenn man zum Beispiel eine Scheibe reifen Gouda am Morgen isst und eine kleine Tomate als Nachmittagssnack, wird das meist besser vertragen als wenn man beide histaminreichen Speisen gleichzeitig verzehrt.
Generell sollten Sie Lebensmittel so frisch wie möglich verzehren. Gerade leicht verderbliche Gerichte wie Hackfleisch und Fisch sollten Sie nicht ein zweites Mal aufwärmen – der Verzehr führt schnell zu Symptomen einer Histaminintoleranz.
Hier noch einige Tipps für bestimmte Lebensmittel und Getränke:
Käse: Verzichten Sie auf Hartkäse (wie Emmentaler, Bergkäse, Parmesan), lang gereiften Schnittkäse (etwa alten Gouda), sehr reifen Schimmelkäse (wie sehr weichen Camembert) sowie Rohmilch- und Schmelzkäse. Greifen Sie lieber zu jungen Käsesorten (wie Butterkäse), Streichkäse, Frischkäse, Cottage Cheese und Topfen.
Wurst und Fleisch: Anstelle von Rohwurst (wie Salami, Rohschinken, Teewurst) sollten Sie Kochwurst (Fleischwurst, Kochschinken) wählen. Bei Fleisch stellen besonders mariniertes (Grillfleisch, Gyros, Dönerfleisch) und lang gegartes Fleisch (Gulasch, Braten) für Menschen mit Histaminintoleranz Lebensmittel dar, die oft Probleme bereiten.
Fisch: Meiden Sie Fischsorten wie Makrele, Sardelle, Hering und Thunfisch. Bekömmlicher als geräucherter, getrockneter und gesalzener Fisch ist frischer oder tiefgekühlter Fisch.
Alkohol: Rotwein enthält meist mehr Histamin als Weißwein. Besonders histaminreich sind französischer Rotwein, Chianti und Muskatwein.
Süßigkeiten und Knabbereien: Schokolade und andere kakaohaltige Süßigkeiten werden meist schlecht vertragen. Das Gleiche gilt manchmal auch für Lakritz. Stillen Sie Ihre Lust auf Süßes besser mit Fruchtgummi und Bonbons (beide ohne Azofarbstoffe) sowie schokoladefreie Kuchen und Gebäckwaren. Salzstangen und Kartoffelchips ohne Geschmacksverstärker und Hefeextrakt sind in der Regel unproblematisch bei Histaminintoleranz. Lebensmittel mit Nüssen (wie Nusskuchen) hingegen sollte man meiden, da sie Histamin freisetzen können.
Histaminintoleranz: Verlauf und Prognose
Die richtige Ernährung bei Histaminintoleranz ist der wichtigste Baustein der Behandlung. Wer auf histaminreiche Lebensmittel (weitgehend) verzichtet, kann seine Beschwerden meist deutlich verbessern. Tragen bestimmte Medikamente zu den Histaminintoleranz-Beschwerden bei, kann der Arzt den Patienten in vielen Fällen auf ein besser verträgliches Präparat umstellen. Ergänzend können im Bedarfsfall Medikamente wie Antihistaminikak die Beschwerden lindern.
Viele Patienten mit Histaminintoleranz leiden gleichzeitig an Nahrungsmittelunverträglichkeiten wie Fruktose-, Laktose- oder Sorbit-Intoleranz. Wenn man zu viele Lebensmittel (histaminhaltige Speisen, Obst, Milchprodukte etc.) vom Speiseplan streicht, kann es unter Umständen zu einer Mangelversorgung kommen. Die Ernährung bei Histaminintoleranz plus Nahrungsmittelunverträglichkeiten muss daher besonders sorgfältig geplant werden. Ein Ernährungsberater kann Patienten hier wertvolle Unterstützung geben.
Additional information
Bücher:
- Histaminintoleranz – die unentdeckte Krankheit: Histamin – eine häufige Ursache für Allergien, Nahrungsmittelintoleranzen und vieles mehr! (Rainer Bloch und Sigrid Nesterenko, Rainer Bloch Verlag, 2017)
guidelines:
- Leitlinie zum “Vorgehen bei Verdacht auf Unverträglichkeit gegenüber oral aufgenommenem Histamin” der Deutschen Gesellschaft für Allergologie und klinische Immunologie, der Gesellschaft für Pädiatrische Allergologie und Umweltmedizin, des Ärzteverbandes Deutscher Allergologen und der Schweizerischen Gesellschaft für Allergologie und Immunologie (2017)