Hepatitis is an inflammation of the liver. This can be caused by viruses, toxins, drugs or autoimmune diseases. Physicians distinguish different forms of hepatitis depending on the cause, duration and histologic features. Read more about symptoms, causes and treatment of liver inflammation and how to prevent hepatitis!

Quick Overview
- What is hepatitis? An inflammation of the liver that can be acute or chronic
- To shape: Viral hepatitis (hepatitis A, B, C, D, E), viral concomitant hepatitis, autoimmune hepatitis
- symptoms: sometimes no symptoms; in other cases, significant to severe symptoms such as nausea, fever, upper abdominal pain and possibly jaundice
- Causes: Viruses, poisons (such as alcohol), medications, metabolic diseases, autoimmune processes
- Treatment: depending on the cause and severity of the disease; e.g. Protection, light food, alcohol abstinence, medication, possibly liver transplantation
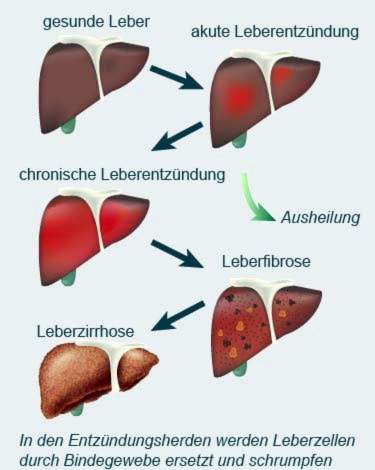
- Forecast: Acute forms usually heal by themselves. Chronic forms can permanently damage the liver. Cirrhosis and liver cancer are possible consequences.
Forms of hepatitis
The term hepatitis means liver inflammation. But that is already over with the simplicity. The exact nature of hepatitis can only be answered a little more vaguely because there are different forms of the disease.
First of all, the duration of hepatitis can be divided into two forms:
- acute hepatitis: lasts less than half a year
- chronic hepatitis: lasts longer than six months, develops mainly from hepatitis B, C and D.
Also according to the cause you can divide hepatitis:
- Viral hepatitis: Hepatitis A, B, C, D or E hepatitis viruses (all reportable)
- Virus accompanying hepatitis: Liver inflammation as a “by-product” of another viral disease (herpes, glandular fever)
- Autoimmune hepatitis: Liver inflammation due to dysfunction of the immune system
Very rarely, hepatitis is caused by parasites, fungi or bacteria.
Hepatitis A
Hepatitis A becomes major transferred fecal-oralFor example, about drinking water that has been contaminated by the excrement of patients. The infection can also over contact infection If patients do not wash their hands thoroughly after going to the bathroom, they can, for example, transfer the viruses to doorknobs, taps, cutlery or towels. From there, the pathogens can reach the hands and eventually the oral mucosa of healthy people.
Sometimes hepatitis A is also over contaminated food (Seafood, ice cream, fruit, etc.).
After infection, 15 to 50 days pass before the first symptoms appear (incubation period). These include non-specific symptoms such as fever, nausea or loss of appetite. Later, skin and eyeballs sometimes turn yellow, the urine becomes dark and the stool becomes light. Several months may pass before the patients have recovered. However, hepatitis A infection can not become chronic. In addition, one is immune to hepatitis A virus for a long time after surviving infection.
Everything important about this form of liver inflammation can be read in the article Hepatitis A.
Hepatitis B
Hepatitis B is one of the most common viral hepatitis worldwide. The infection takes place via blood and sexual contacts (sperm, saliva). Hepatitis B viruses can also be transmitted via other body fluids such as tears, cerebrospinal fluid (CSF), urine, gastric juice and breast milk. Overall, especially medical staff, Dialysepatienen such as drug addicts (Spraying!) A high risk of infection.
Type B liver inflammation can be both acute and chronic. The first symptoms appear on average two to four months after the infection.
Chronic hepatitis B is widespread. According to the World Health Organization (WHO), around 240 million people worldwide suffer from it. As a result of chronic liver inflammation, a shrinking liver (liver cirrhosis) and a malignant liver tumor (liver cancer) may develop.
You can get more information about hepatitis B in the text Hepatits B.
Hepatitis C
Experts estimate that around 71 million people worldwide have chronic hepatitis C. The triggering viruses can be detected in almost all body fluids. The infection will however transmitted mainly via blood, The risk of infection is particularly high with contaminated cutlery for drug use, but also with tattooing or Piercingwerkzeug. In about 30 percent of all patients with chronic hepatitis C, no clear transmission pathway can be established.
About ten percent of hepatitis C patients have an infection with the hepatitis G virus at the same time. So far, no symptoms are known that can be clearly assigned to this pathogen. In addition, it is difficult to detect hepatitis G viruses.
The symptoms of hepatitis C are usually mild and rather unspecific: those affected, for example, muscle and joint pain, mild fever, nausea and aversion to certain foods. Later, dark urine, yellowing of the skin and eyeballs (jaundice) and discolored stools may occur.
Chronic hepatitis C is ongoing usually creeping and unnoticed for many years, However, patients have a fairly high risk of liver cirrhosis or liver cancer.
Read more about this hepatitis form in the article Hepatitis C.
Hepatitis D
Hepatitis D viruses can only multiply with the help of hepatitis B viruses and cause an infection. This means that a hepatitis D infection is only possible in people who are either simultaneously infected with hepatitis B or already have a chronic hepatitis B infection.
Together, hepatitis B and D often lead to severe chronic hepatitis
Hepatitis E
The hepatitis E virus is found mainly in Asia and Africa. The disease is transmitted mainly via drinking water or food. A human-to-human transmission is very rare.
Hepatitis E is acute and often mild, similar to hepatitis A. The symptoms are noticeable two to eight weeks after infection and resolve after about six weeks.
In general, hepatitis E is not particularly dangerous. Only in pregnant women can it be severe in rare cases and even end fatally.
Read all important about this type of hepatitis in the article Hepatitis E.
Autoimmune hepatitis
In contrast to the hepatitis forms mentioned above, autoimmune hepatitis is not caused by viruses, but a malfunction of the immune system. This form of liver inflammation is very rare. Most commonly, autoimmune hepatitis occurs between the ages of 40 and 70 years. Most patients are female.
Autoimmune hepatitis is almost always chronic. Often, then, for a long time, no or only nonspecific symptoms such as tiredness, loss of appetite, abdominal and headache as well as nausea and vomiting. In severe cases, chronic autoimmune hepatitis leads to cirrhosis – with the risk of liver failure.
The therapy of autoimmune hepatitis consists in the administration of immunosuppressants. These are medicines that suppress the immune system. In liver cirrhosis a liver transplant may be necessary.
Read more about risk factors, symptoms and disease progression in Autoimmune Hepatitis.
Hepatitis: Symptoms
Hepatitis symptoms can be quite different. In some patients, hepatitis is severe. Others, on the other hand, have no symptoms, and the disease is only discovered by chance because of elevated liver enzymes. Sometimes, but not always, occurs jaundice (jaundice), which is often mistaken for hepatitis.
Acute hepatitis: Symptoms
The symptoms of acute hepatitis are in the early phase non-specific and include:
- Nausea and vomiting
- anorexia
- fever
- Epigastric pain
- Joint or muscle pain
- changed sense of smell and taste
After two to eight weeks follows the Jaundice phase, The enlarged liver causes pressure pain under the right lower costal arch. The skin may turn yellow, as do the eyeballs. This is because the bile pigment bilirubin is no longer released into the intestine via the bile, but is accumulated in the blood. As part of it is excreted via the kidneys, the urine turns dark. By contrast, the stool loses its typical color due to the bacterial processing of bilirubin. Itching is also a common symptom. It arises because bile acids accumulate in the skin.
The recovery phase (convalescence) of acute hepatitis may take several weeks to months. During this time, sufferers occasionally feel weak, tired and exhausted.
Chronic hepatitis: symptoms
Chronic hepatitis manifests itself in symptoms like
- reduced efficiency
- fatigue
- anorexia
- Pressure pain under the right costal arch
- joint pain
- changing diarrhea
In mild (re) n cases, it may well be that no symptoms occur. Typical are thrusts with enlarged liver and jaundice. In addition, the rule can be missed for women. In males, the mammary glands (gynecomastia) may enlarge, the testes become smaller (testicular atrophy) and / or the hair on the abdomen and pubis are less (stomach bald).
Hepatitis: causes and risk factors
In the vast majority of cases, hepatitis is a viral disease (viral hepatitis). It is mainly caused by type A, B, C, D or E hepatitis viruses. All are notifiable.
Sometimes other viruses can trigger a usually milder viral hepatitis. This applies, for example, to the Epstein-Barr virus (Pfeiffer’s glandular fever), cytomegalovirus (CMV infection), Coxsackie virus and herpes viruses. Then doctors speak of one Virus accompanying hepatitis.
Occasionally, liver inflammation is the result of dysregulation of the immune system (Autoimmune hepatitis).
Rare are bacteria such as Leptospira (leptospirosis), Brucellen (brucellosis) or Salmonella (salmonellosis) as well as parasites (Causative agent of amoebic dysentery and malaria) the cause of hepatitis.
At a toxic hepatitis on the other hand, alcohol is usually the “culprit”. Doctors also speak of one here alcoholic fatty liver hepatitis (Medical Steatohepatitis, ASH). In those affected, excessive consumption of alcohol damages the liver. As a result, fat accumulates and inflammation occurs. If alcohol is consumed further, liver cirrhosis may develop.
There is also a non-alcoholic fatty liver hepatitis (non-alcoholic steatohepatitis, NASH). It is caused, for example, by obesity or diabetes mellitus.
An excess liver damaging drugs Paracetamol or certain anesthetic gases (eg halothane) can also cause toxic hepatitis. The same applies poisons like that of the tuberous mushroom.
Chronic hepatitis results from existing acute hepatitis such as:
- Hepatitis B, C or D
- toxic hepatitis (caused by certain drugs or alcohol)
- Autoimmune hepatitis
- a (cholestatic) liver disease caused by biliary congestion, such as inflammation of the inner and outer bile ducts (primarily sclerosing cholangitis)
- a liver disease originating from the internal bile ducts (primarily biliary cirrhosis)
Furthermore you can congenital metabolic diseases cause chronic hepatitis. These include the copper storage disease (Wilson’s disease) and the iron storage disease (hemochromatosis).
In some cases, the cause of chronic liver inflammation can no longer be reliably proven. The doctor can then only guess.
Hepatitis: transmission
The five most common forms of viral hepatitis (types A, B, C, D and E) can be transmitted in different ways. In general, there is an increased risk of hepatitis infection in the following cases:
- Drug addicts who inject the drug into the veins and share the syringe with each other
- medical staff, which often comes in contact with infected body excretions of patients (such as blood)
- Unprotected intercourse, especially with frequently changing sexual partners
- People who can be pierced in non-sterile conditions pierced ears, piercings or tattoos
- Travelers traveling in poorly hygienic countries (especially hepatitis A)
- Babies of mothers who are infected with hepatitis B or C (transmission before or during birth)
- Blood products (donor blood, blood coagulation factors, etc.), which are transmitted as a transfusion (since the introduction of strict controls in Germany only rarely a hepatitis transmission path)
- Dialysis patients (if the dialysis machine was previously used in a hepatitis patient and then not thoroughly cleaned as prescribed)
Hepatitis: examinations and diagnosis
If you suspect liver inflammation, you should visit your family doctor or internist. This will be your first in a detailed conversation To raise medical history (Anamnese). He gives a detailed description of your symptoms and inquires about possible liver-damaging influences. Possible questions of the doctor can be:
- Do you drink alcohol? If so, which one, how much and how long?
- Do you have pre-existing conditions such as diabetes mellitus or cancer?
- What do you do for a living? Are you in contact with toxins such as carbon tetrachloride, vinyl chloride or phosphorus?
- Do you take medications like acetaminophen, tetracycline, methotrexate, isoniazid, rifampicin or azathioprine?
- Do you take drugs?
- Did you receive a blood transfusion?
- Have you been abroad recently?
- Did you have sexual contact with frequently changing partners?
- Does the family have metabolic disorders such as Wilson’s disease or a1-antitrypsin deficiency?
In addition, the doctor will ask you if yours Weight has changed up or down. Tell him too, if you have been lately loss of appetite suffer or get the Color of your stool and / or urine has changed. An important hint can also be a increased bleeding tendency be. It may be caused by, for example, the liver forming less clotting factors than normal due to disease / injury.
Physical examination
After the anamnesis interview, a physical examination follows. The doctor will, among other things, scan your stomach. There is a pressure pain in the right upper abdomen, this indicates a possible liver disease. When palpating the doctor can also determine whether the liver and / or spleen are enlarged. He will also look for signs of jaundice during the examination.
blood tests
By measuring different blood values, the performance of the liver can be determined. Typically, liver inflammation increases liver enzymes GOT (AST) and GPT (ALT). In technical jargon these liver enzymes are also called transaminases.
To determine if it is a viral infection, the blood sample is tested for antibodies to hepatitis viruses (A, B, C, D and E) (hepatitis serology). So that’s one indirect hepatitis test: It is not looking directly for the pathogens of viral hepatitis, but for specific antibodies that the body produces in an infection with such agents. The type of antibody detected also indicates how far the liver inflammation has progressed.
It is also possible a direct Hepatitis Test: In doing so, one checks whether the genotype of the various hepatitis viruses can be detected in the patient’s blood. Maybe it is necessary to the small genome “snippets” by means of the so-called Polymerase chain reaction (PCR) before they can be identified.
The suspicion of autoimmune hepatitis can be confirmed, if typical in the blood Autoantibodies are found, which attack the liver tissue.
Ultrasonic
An ultrasound scan can help the physician to understand the size and structure of the liver. In the case of chronic liver inflammation, the study may also indicate if the disease has led to shrinking liver (liver cirrhosis) or even to liver cancer.
Cirrhosis of the liver and its “precursor” – the liver fibrosis – can also be detected with a special ultrasound examination – the so-called elastography.
Tissue sample of the liver
Generally, in liver disease, the doctor will usually take a tissue sample from the liver (liver biopsy) to have them examined more closely in the laboratory. Thus, the suspicion of liver inflammation can finally be clarified. On the basis of the histologic examination of the tissue sample one can also assess the degree of liver inflammation.
Hepatitis: treatment
Hepatitis patients should no alcohol consume. In addition, they should (in consultation with the doctor) Avoid liver-damaging medication, This is not only true if the hepatitis is caused by alcohol or medication, but in all other cases. The breakdown of alcohol and medication takes place in the liver and can put a heavy burden on the inflamed organ. This can worsen the course of the disease.
Further hepatitis treatment depends on the cause, course and severity of the disease.
In acute hepatitis, patients should be save, Maybe the doctor even recommends bed rest, Besides that is light food advisable, which is rich in carbohydrates and low in fat. A special diet is not necessary.
Sometimes acute hepatitis heals by itself. If necessary, symptomatic measures are useful, such as painkillers for severe muscle and joint pain or a remedy for nausea and vomiting.
In some cases, hospital inpatient hepatitis therapy is needed.
In many cases, however, liver inflammation must be specifically treated with medication become. For example, people with chronic hepatitis B or C receive antiviral drugs. In autoimmune liver inflammation (autoimmune hepatitis) drugs are used, which inhibit the immune system. These include cortisone and azathioprine.
For severe hepatitis, one can liver transplantation become necessary. However, finding a suitable donor organ is often not easy.
For hepatitis B and C, it is important to inform your family and sexual partner about the condition. These can then be vaccinated so as not to infect you.
Hepatitis: disease course and prognosis
An acute hepatitis usually heals by itself again. If it is caused by medication or alcohol, avoiding these substances helps the liver to recover. The prerequisite is that the organ is not permanently damaged.
Especially with alcohol abuse and hepatitis C in the chronic course, the risk increases that the liver is scarred (liver cirrhosis) and permanently damaged. Also, liver cancer (hepatocellular carcinoma = hepatocellular carcinoma) is a common complication of chronic hepatitis (especially type B). A vaccine can protect effectively here.
Hepatitis: prevention
Most important for the protection against a viral hepatitis infection hygiene and (for hepatitis viruses A and B) a vaccine (see below).
Hepatitis A and E are mainly transmitted via contaminated drinking water and food. Therefore, pay attention to careful Food hygieneespecially when traveling. With tap water, ice cubes, raw vegetables and seafood (especially mussels and oysters) you should be extra careful. In general, you should follow the rule of thumb in countries with a high risk of infection when eating: “Cook it, peel it or forget it”.
In Germany and other industrialized countries, hepatitis E is often transmitted via poorly cooked pork or venison. Therefore, meat should always be cooked well.
You can prevent an alcoholic hepatitis disease by taking Alcohol – if anything – only very moderate enjoy.
If you are taking medications, ask your doctor if they can damage your liver. Possibly is a switch to one less liver-damaging preparations possible.
Heavy obesity and a high-fat diet can promote hepatitis. You should therefore go to one healthy body weight pay attention and yourself to feed balanced.
Hepatitis vaccination
You can get vaccinated against hepatitis A and B. In China, a hepatitis E vaccine is also available. This is not allowed in Europe.
The Ständige Impfkommission (STIKO) at the Robert Koch Institute recommends the hepatitis A vaccine especially for travelers in regions with increased risk of infection. Such regions are about many tropical countries as well as the Mediterranean and Eastern Europe. People with a high risk of infection should also be vaccinated against hepatitis A. These include, for example, medical personnel, sewerage workers and people with the haemophilia haemophilia, who get transmitted blood clotting factors.
Vaccination against hepatitis B is also particularly important for people with a high risk of infection (such as medical staff). In addition, the STIKO recommends vaccination for all infants.
Read more about the benefits and risks of such vaccinations and about the possible reimbursement of costs by the health insurance companies in the article “Hepatitis vaccine”.
Additional information
guidelines:
- Guideline “Prophylaxis, Diagnosis and Therapy of Hepatitis Cvirus (HCV) Infection” of the German Society of Gastroenterology, Digestive and Metabolic Diseases (2016)
- Guideline “Prophylaxis, Diagnosis and Therapy of Hepatitis B Virus Infection” of the German Society of Gastroenterology, Digestive and Metabolic Diseases (2011)
Support Groups:
- German Liver Assistance e.V.
- German Liver Foundation