In a spinal stenosis (spinal stenosis, spinal stenosis, edema stenosis) the channel is narrowed in the spine through which the spinal cord passes. The resulting pressure on the spinal cord, nerves and blood vessels can cause back pain and permanent nerve damage. Mostly a spinal canal narrowing arises as a result of aging processes. Read here about the causes, symptoms and treatment options of spinal stenosis.

Quick Overview
- causes: Mostly wear (degeneration) of the spine. Rare congenital constrictions (hollow back, spinal deformities), spinal surgery, disc protrusion or prolapse, hormonal changes, bone diseases such as Paget’s disease.
- symptoms: Initially often asymptomatic. Later unspecific complaints such as back pain with radiating to the legs (lumboischialgie), decreased mobility of the lumbar spine and muscle tension in the lower back. In case of severe spinal canal stenosis feelings of weakness and feeling of weakness in the legs, limp (claudication spinalis), bladder and / or rectal disorders, disturbed sexual function. Very rare Cross-sectional syndrome with paralysis of the legs and problems with bowel movements and / or urination.
- Diagnosis: Based on the characteristic symptoms associated with imaging techniques (magnetic resonance imaging, computed tomography).
- treatment: Most conservative therapy with a combination of physiotherapy, back therapy, heat therapy, electrotherapy, orthopedic brace, pain management training and pain therapy. Rarely, surgery is needed to relieve the spinal canal.
- History and prognosis: Even without therapy usually very slow course. With consistent conservative therapy, the typical symptoms can usually be treated and alleviated well.
Spinal stenosis: causes
The most common cause of the spinal stenosis is the Wear (degeneration) the spine: Over time, the discs between the vertebral bodies lose fluid. As a result, they become flatter and can thus cushion bad movement-related pressure – that is, the vertebral bodies are more heavily loaded and then press on the spinal canal (spinal canal).
Due to the shrunken intervertebral discs, the ligaments along the spine are less taut and lose their elasticity. Thus, the entire spine structure can become latent unstable. The vertebral bodies may shift against each other (spondylolisthesis, spondylolisthesis) and compress the vertebral canal.
A well-trained back muscles then stabilizes the spine, so that one is symptom-free despite spinal stenosis. In contrast, patients with poorly developed back muscles often develop typical stenosis symptoms. Because when the muscles can not support the unstable spine, the body creates new bone structures on the vertebral bodies to stabilize the spine. These newly formed bony structures become osteophytes called. They can not only worsen, but also cause a spinal canal narrowing.
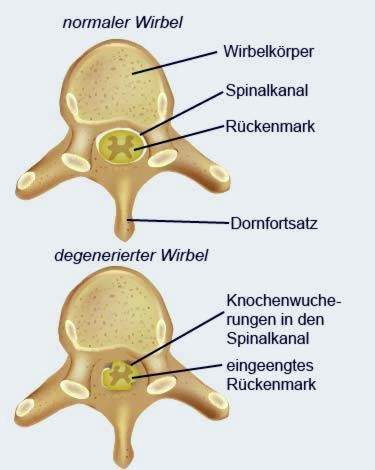
Also one Osteoarthritis of the vertebral joints (Facet joints) can lead to bony neoplasms and thus favor a spinal stenosis.
Rarer causes for a spinal canal stenosis are:
- Congenital malformations such as a strong hollow back, spondylolisthesis, chondrodystrophy (disturbances in the conversion of cartilage to bone tissue in the embryonic age). The symptoms occur in such cases already at the age of 30 to 40 years.
- Spinal surgery (the excessive formation of scar tissue can narrow the spinal canal)
- Injuries to the vertebral bodies
- Bulges or prolapse of disc material into the spinal canal
- hormonal changes affecting the bone substance and the stability of the vertebral bodies (e.g., Cushing’s disease)
- Bone diseases (such as Paget’s disease): This leads to a localized remodeling and cultivation of bone. Spinal stenosis in this disease is more common in the lumbar spine than in the cervical spine.
- narrowed spinal canal of unknown cause (idiopathic spinal canal stenosis)
Spinal stenosis: symptoms
A spinal stenosis usually occurs in the Lumbar area (lumbar spinal canal stenosis) on. It does not necessarily lead to complaints. Such occur only when the spinal canal is narrowed so that nerves or blood vessels are compressed. Which symptoms are specific, when and how strongly they occur depends on several factors. These include the severity of the disease, the patient’s posture and the level of exercise.
At the beginning of the disease, the symptoms are less characteristic and diverse. These non-specific complaints include:
- Back pain in the lumbar region (Lumbago), which usually radiate unilaterally in the legs (lumboischialgie)
- decreased mobility in the lumbar region
- Muscle tension in the lumbar region
If the stenosis continues, the following symptoms are possible:
- Feelings in the legs
- Lesions in the legs, e.g. Burning, running ants, feeling cold, cotton wool feeling underfoot
- Feeling of weakness in the leg muscles
- pain-related limping (Claudicatio spinalis)
- Bladder and / or rectal disorders (problems with bowel movements and urination or incontinence)
- disturbed sexual function
Typical of the disease is that the discomfort in sitting or in other positions in which the trunk is bent forward (for example when cycling, bending over and going uphill) usually improve significantly.
Limping in spinal stenosis (claudicatio spinalis) must be distinguished from temporary limping due to circulatory disturbances in the case of “intermittent claudication” (PAD). The latter is called intermittent claudication.
Very rarely, the spinal stenosis leads to a so-called Spinal cord injury: Both legs are paralyzed, and there are problems with bowel movements and urination.
Sometimes, the narrowing of the spinal canal does not affect the lumbar region but the lumbar spine Cervical region (cervical spinal canal stenosis), The sufferers often have neck pain that radiate in the arms. Over time, emotional disorders in the legs, rectal and bladder disorders can also develop here.
Spinal canal stenosis: treatment
In most cases, the spinal stenosis can be treated well with conservative therapies. Only rarely (in very severe cases) surgery is necessary.
Conservative treatment
Conservative therapies for spinal stenosis include:
- Physiotherapy (exercise therapy, baths, muscle-relaxing treatments, etc.) to relieve and stabilize the spine
- Heat therapy to relax the back muscles
- Electrotherapy for pain treatment and muscle relaxation
- Support corsets (orthoses) to relieve the spine
- Back training (targeted strengthening training for the back and abdominal muscles, tips for back-friendly postures, behavioral tips)
- Psychological pain management training
- pain Management
Most of these measures are combined. This is called a modular therapy concept.
drugs
Effective pain management is a cornerstone of conservative stenosis therapy. Depending on the intensity of the pain different agents are used. For mild pain can non-opioid analgesics like ibuprofen, paracetamol or diclofenac. They have an analgesic and anti-inflammatory effect (the latter is very low in the case of acetaminophen). For moderate pain come slight opioids used, often in combination with mild (non-opioid) analgesics. Strong pain, however, with strong opioids treated.
Some analgesics may irritate the stomach lining after prolonged ingestion. That is why doctors often prescribe so-called accompanying Proton pump inhibitors, These medications provide “stomach protection” for the body to produce less stomach acid.
In addition to the classic painkillers, the doctor may be mild antidepressants prescribe. In low dosage they can help with chronic pain.
Sometimes, with a spinal stenosis, too Muscle-relaxing drugs help. For very severe pain may come one high-dose cortisone therapy question: Cortisone causes the soft tissues that press on the spinal canal to swell. So in the channel again a little more space.
The various active ingredients with analgesic, anti-inflammatory, locally anesthetic and / or decongestant effect can often be administered not only via the mouth (as a tablet, capsule, etc.). In many cases, they can also be injected directly into the affected area of the spinal canal narrowing. These injection therapy is especially indicated when a nerve root is highly inflamed. The combination of anti-inflammatory agents such as cortisone and analgesics combats the inflammation and relieves the pain-related symptoms. On the other hand, if the pain comes from the small vertebral joints, local injections with painkillers can help.
In injection therapy studies, patients have been given ineffective substances (placebo) rather than real medicines, often simple saline. Despite this sham treatment, many patients subsequently had less pain. The researchers discovered that the placebo injections released the body’s own “painkillers” (endorphins).
surgery
Almost all patients with spinal stenosis are treated conservatively. Surgery is rarely necessary – usually when important nerves fail. In addition, surgery can be performed if the conservative treatment fails or the patient has a strong emotional distress and is clearly limited in his everyday life.
The surgical procedure always aims to relieve the region in which the spinal cord is squeezed. There are several methods available for this:
- The Pressure relief (decompression) The constricted nerves are considered the method of choice. For this, the vertebral arch at the stenosis site is removed on one or both sides together with the spinous process (hemi- / laminectomy). Sometimes only parts of the vertebral arch are removed (microdepression).
- Fusion (spinal fusion): Individual vertebrae are connected and stiffened by material from the iliac crest or by screws. This prevents them from sliding into each other and narrowing the spinal canal.
- Interspinous implants connect the spinous processes of the vertebral bodies and thus prevent the forward or backward tilt of the spine in the affected area.
Which method is most suitable in a particular case, decides the doctor. All three procedures can usually minimally invasive or microsurgical be performed. This means that the physician does not have to cut much to reach the affected area. Several small incisions are enough, through which the surgeon introduces a tiny camera with light source and the fine surgical instruments.
Every operation involves certain risks. For example, nerves can be damaged during the procedure. In addition, the “skin” around the spinal cord can be injured so that fluid from the spinal cord escapes (liquor fistula). Therefore, before undergoing spinal canal stenosis, the physician will carefully weigh up the expected benefits and potential risks.
Spinal stenosis: examinations and diagnosis
in the first meeting (Anamnesis) the doctor interviews the patient in detail about his complaints and known pre- or underlying diseases (herniated disc, osteoarthritis, osteoporosis, etc.). After that follows one physical examination: Among other things, the doctor may ask the patient to bend the upper body first far back and then forward. If there is a spinal canal stenosis, the back hurts, while the symptoms disappear when the trunk is bent.
Provide further information Imaging procedures, Experts recommend primarily magnetic resonance imaging (magnetic resonance imaging, MRI) without contrast medium. It can depict nerves, intervertebral discs, blood vessels and other structures in detail in detail.
Alternatively, the spine can be visualized by computerized tomography with contrast media. However, this so-called myelo-CT exposes the patient to a certain radiation exposure.
Not every narrowing of the spinal canal that is visible on MRI or other imaging techniques actually causes discomfort!
In addition, the doctor can x-ray the patient while standing and in certain postures (functional shots).
To clarify a spinal stenosis can also electrophysiological examinations be used. These include, for example, an electromyography (EMG) and so-called evoked potentials. These methods help to assess the function of nerves.
Spinal stenosis: history and prognosis
Even if it is not treated, the spinal stenosis usually progresses only very slowly. Depending on the cause, the disease can also be very different. The pain caused by the pressure on the nerve tracts can remain constant, decrease with certain movements or with time or come and go constantly. Sometimes the symptoms diminish even in old age as the spine becomes less mobile. Because then the nerves are irritated less often, motion-dependent pain occur less frequently.
In some cases, a spinal canal stenosis is acute: if, for example, disc tissue shifts (protrusion, prolapse), if arthrosis causes capsular swelling, or if fluid accumulates near the nerve tracts, the symptoms of spinal canal stenosis can suddenly become worse. Often, one side of the body is particularly affected.
Overall, the Spinal Stenosis in most cases treat well with conservative treatment methods, so that those affected can live relatively free of charge.
Additional information
guidelines:
- Guideline “Lumbar Spinal Canal Stenosis” of the German Society for Orthopedics and Orthopedic Surgery and the Professional Association of Doctors for Orthopedics (2002)