Rubella is an acute and contagious viral infection. They can cause a typical red rash. In some people, the infection is also without symptoms. Rubella most commonly affects baby and toddler. Rubella is much rarer in adults. In most cases, an infection is without complications. During a pregnancy, however, it can be dangerous for the unborn baby. Read all important information about rubella here.

Quick Overview
- symptoms: first cold-like symptoms, followed by the typical rubella rash: small, bright red patches that first appear behind the ears and then spread across the face to the entire body;
- Reason: Viruses (so-called rubella viruses)
- Infection: via droplet infection; between infection and the appearance of the first symptoms pass two to three weeks (incubation period)
- Treatment: often not necessary; possibly measures that relieve the symptoms (for example, analgesics and antipyretics)
- Danger: Rubella in pregnancy can be transmitted to the unborn baby. Especially in early pregnancy then threaten severe harm to the child.
- Prevention: Rubella vaccination
Rubella: symptoms
Rubella symptoms can be slightly different in each person. In addition, many of them are not specific to the disease. That means similar complaints can also show up in other diseases.
Up to 50 percent of all people who get infected with rubella show no symptoms. Then doctors speak of an asymptomatic course.
First rubella symptoms
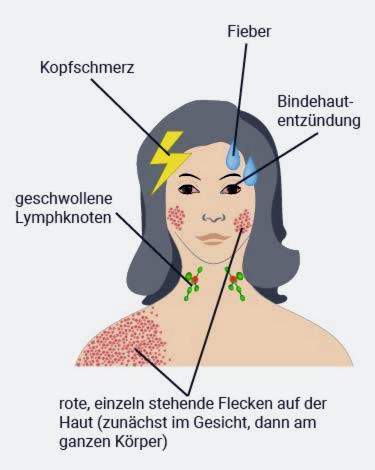
The first symptoms, which usually occur in a rubella disease, are reminiscent of a common cold. These include, for example to cough, sniff and mild to moderate a headache, In some cases, one comes Conjunctivitis added. The eyes look red and may itch. Often these remain the only rubella symptoms. They are then usually not recognized as rubella.
Classical rubella symptoms
In addition to the signs of a cold, about half of all patients experience additional symptoms. These include swollen, often painful lymph nodes in the neck and neck area (in adolescents and adults often at other parts of the body). This swelling occurs because the pathogens initially multiply in the lymph nodes before they spread through the blood in the body. The lymph nodes behind the ears and neck can also hurt or itch.
In some patients, the rubella infection is one of increased body temperature (below 38 degrees Celsius).
Typical of rubella is a skin rash (Exanthem) from small, light red, slightly raised spots. He does not itch, or at most easily. The red spots do not fuse together, as is the case with the measles. Often the rubella rash is only slightly visible. He first forms behind the ears. Over the course of a few hours, it spreads to the face, neck, arms and legs and finally to the whole body. After one to three days, the rash disappears again.
In Germany, rubella is sometimes referred to as “Rubeola”. The term originally covers all skin diseases with a red rash. That’s why he’s misleading. In England, for example, the term is used for measles. In addition, scarlet fever is called in the jargon “Rubeola scarlatinosa”. Because of the possible misinterpretation “Rubeola” is therefore rarely used in German.
Rubella: complications
The rubella is usually mild and harmless. But they can also cause complications. The risk increases with age. That is, rubella in adults (and adolescents) is more likely to have complications than children.
Possible complications are:
- Arthritis: especially young women with rubella often get swollen, aching joints
- bronchitis
- Middle ear infection (otitis media)
- Brain inflammation (encephalitis)
- Myocarditis (myocarditis)
- Pericarditis (pericarditis)
Rubella: infection
The rubella contagion occurs over droplet infection: When coughing, sneezing or kissing Infected small saliva droplets with the rubella viruses can be transmitted to other people. The viruses enter the body through the mucous membranes of the upper respiratory tract (mouth, nose, throat). Also about objectsInfected with the pathogens, a contagion is possible: For example, if you use the same cutlery as a sick person, you can also become infected.
The following applies: People who are not vaccinated against rubella or have not yet had the disease can be infected. Rubella symptoms in spite of vaccination or a successful infection are as good as ever: Only if the vaccination or the disease is very long ago, you can possibly get infected again with rubella. Such reinfection but it is very rare. The affected then usually show no and only very mild symptoms (such as run cold).
Rubella: incubation period
The time between the infection with a pathogen and the onset of the first symptoms refer to doctors as the incubation period. For rubella it is between 14 and 21 days. Infected people are contagious for about a week before to about a week after the appearance of the typical rash.
Even those who are infected with rubella viruses, but shows no symptoms (so do not get sick), can transmit the pathogens to other people!
Rubella & pregnancy
Rubella in pregnancy is very feared: the pathogen can be transmitted from the mother via the placenta to the unborn child. Such a childlike rubella infection in the womb becomes congenital rubella syndrome called. It can damage the child’s organs so badly that it is born with significant disabilities. A miscarriage is possible.
The decisive factor is the stage of pregnancy: The damage that rubella can cause in children in the womb is the more frequent and serious the earlier the infection occurs. Any defects that can cause rubella infection in the unborn child are termed “Congenital rubella syndrome“(CRS) summarized.
Rubella in the 1st to 11th week of pregnancy
Rubella infection in the 1st to 11th week of gestation can cause particularly many and severe damage to the child. The rubella embryopathy can occur in different forms:
- clinical triad (Gregg syndrome): Organ malformations of the heart, eye and inner ear (such as heart defects, cataract, hearing damage)
- extended rubella syndrome: Jaundice, skin rash, decreased platelet count (bleeding risk!), Anemia, myocarditis, pneumonia, encephalitis, bone disease
- Late-Onset-rubella syndrome: It does not become noticeable until the 4th and 6th month of life: The babies no longer grow, get a chronic rash and repeated pneumonia. The mortality is high (especially in pneumonia).
- Late effects in youth: Hearing impairment, diabetes (diabetes mellitus), impaired release of hormones, seizure disorders (epilepsy), progressive inflammation of the whole brain tissue (panencephalitis)
In addition to Gregg syndrome and enlarged rubella syndrome, some unborn babies also experience developmental disorders: for example, the head is remarkably small (microcephalus) and mental development is delayed.
Rubella in the 12th to 17th week of pregnancy
A rubella infection of the unborn child in this section of pregnancy usually damages the inner ear: The little ones are born with a hearing loss (inner ear hearing loss).
Rubella after the 18th week of pregnancy
In this phase, a rubella infection is less critical. Maybe the unborn child can develop a little more slowly than it would be the case without infection. As a rule, however, long-term consequences can not be expected.
If a pregnant woman becomes infected with the rubella virus shortly before the birth, it can happen that the newborn is suffering from rubella.
Rubella: cause
The cause of rubella is a virus that is also known as rubella virus or rubella virus. The virus enters the body via the upper respiratory tract mucosa and proliferates mainly in the lymphatic tissue (such as the lymph nodes). From there, the rubella viruses can enter the bloodstream (viraemia) and spread in this way throughout the body.
Rubella: examinations and diagnosis
If rubella is suspected, a doctor should be consulted. Sometimes the disease can be associated with serious complications.
In conversation, the doctor first collects all the important information to the medical history of the patient (anamnesis). He asks the patient (parents, for example):
- Since when is the rash exactly?
- Does the itch itch?
- Is the body temperature elevated?
- Do you feel tired?
The anamnesis is followed by one physical examination, Among other things, the doctor examines the rash and scans the lymph nodes (such as the neck and neck).
On the basis of the medical history and the symptoms, rubella can not be established beyond doubt. Rash and swollen lymph nodes can also occur in many other diseases. Therefore, in case of suspected rubella should always be carried out laboratory tests:
In the blood can be in a rubella infection, the specific body formed by the Defensive substances (antibodies) against the rubella virus prove. This works best from five days after symptom onset (fever and rash).
For pregnant women, such an antibody test is used as a precaution if, according to your vaccination record, the woman was not vaccinated against rubella or only received one of the two recommended rubella vaccine doses. The same applies if the vaccination status is unclear, so you do not know if the woman has ever received a rubella vaccine.
Up to five days after the onset of the rash the doctor may throat swab or one urine sample send to the lab to detect rubella viruses based on their genome. This is a simple, reliable method, especially for children, to safely confirm a suspected rubella and to be able to give good advice to pregnant women (such as the pregnant mother).
Examinations of the unborn child
In pregnant women with suspected or proven rubella infection, the unborn child can also be examined. That happens in the context of prenatal Diagnosis, So an experienced doctor can prepare a sample of the nut cake (chorionic villus sampling) or amniotic fluid (amniocentesis) remove. In the laboratory it is examined whether the genotype of the rubella virus can be detected in the sample.
From the 22nd week of pregnancy, it is also possible to take a blood sample of the unborn child from the umbilical cord using a long, thin needle (Umbilical blood sampling). This fetal blood can be tested for antibodies against rubella viruses or the genome of the pathogens.
Any suspected rubella as well as a proven infection must be reported by the attending physician to the responsible health department. He must also specify the name of the patient. Deaths due to rubella are also notifiable.
Rubella: treatment
There is no treatment that can directly combat the rubella virus – so no causal (causal) treatment, Is possible just a symptomatic treatmentFor example, you can take antipyretic drugs (such as ibuprofen or paracetaml) or calf rolls to lower the elevated temperature if necessary. In itself, fever is desirable – it shows that the immune system combats the pathogen. Therefore, you should reduce fever only when absolutely necessary. The best way to discuss this with the attending physician.
The antipyretics ibuprofen and paracetamol also have an analgesic effect. Ibuprofen also helps fight inflammation. Both drugs are also suitable for rubella patients with headaches and painful, inflamed joints.
Acetylsalicylic acid (ASA) is also a popular painkiller and antipyretic. It must not be used in children and adolescents with feverish diseases! Otherwise, there is a risk that the rare but dangerous Reye syndrome develops.
In a rubella disease and adequate hydration and rest are useful. This helps the body to get well.
Patients should also keep as far as possible from other people. This reduces the risk that they pass on the viruses. In particular, the contact with pregnant women should be avoided: If they are not sufficiently immune to the pathogen, otherwise there are serious risks to the unborn child.
Pregnant women who are not immune to rubella and have had contact with a patient should go to the doctor quickly. Within the first three days after contact, he can inject the pregnant woman with ready-made antibodies against the pathogen. Later, this so-called post-exposure prophylaxis no longer makes sense.
Rubella: disease course and prognosis
A rubella disease usually runs without problems. It does not pose a major threat to children born as well as adolescents and adults in general. With age, however, increases the risk of complications such as sore, inflamed joints, otitis media, bronchitis or myocarditis. Particularly feared is the encephalitis (encephalitis). But it is one of the very rare rubella complications.
Rubella is usually mild in pregnant women too. The danger here is that even the unborn child gets infected. Especially in the first weeks of pregnancy can cause serious damage to the child.
Rubella vaccination
The best protection against rubella is vaccination. The Standing Vaccination Commission (STIKO) at the Robert Koch Institute recommends the rubella vaccine for all children, consisting of two vaccine doses. It is given in combination with the measles and mumps vaccines (measles-mumps-rubella vaccine, MMR vaccine).
The first vaccine dose is recommended for children between the ages of 11 and 14 months (the sooner the better). The second vaccine dose should be given between the ages of 15 and 23 months. There must be a gap of at least four weeks between the two doses.
The rubella vaccine is not only used to protect the vaccinated against infection. Above all, it should also prevent the spread of rubella viruses in the population. This protects even pregnant women who are not immune to the pathogen, as well as their unborn child.
More about the rubella-Vaccination and its possible side effects read in the article rubella vaccine.
Additional information
guidelines:
- Guideline “Laboratory Diagnosis of Pregnancy-Relevant Viral Infections” of the German Association for the Control of Viral Diseases (2014)