Testicular cancer is the most common malignancy in men between the ages of 25 and 45 years. He is generally treatable. Therefore, most patients can be cured. To be able to detect testicular cancer at an early stage, all men from puberty should periodically scan their testicles. Find out everything important on the subject: How can you recognize testicular cancer? What causes him? What treatment options are there? What are the chances of cure for testicular cancer?

Quick Overview
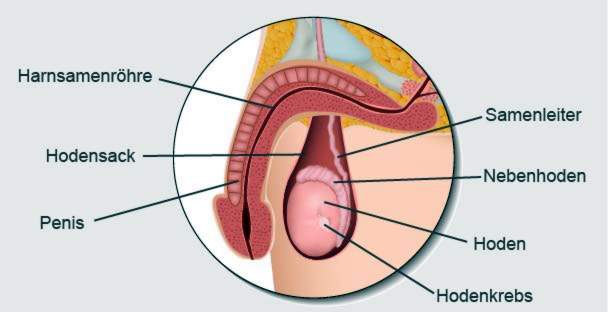
- What is testicular cancer? Malignant tumor of the testicular tissue. Mostly only one testicle is affected. The most common forms of testicular cancer are so-called seminomas, followed by non-seminomas.
- Frequency: Most common cancer in men between the ages of 25 and 45 years (median age of patients: 38 years) – Testicular cancer accounts for 20 to 30 percent of all cancers in this age group. Younger and older men get sick less often. Overall, testicular cancer is a rare cancer (approximately 4,000 new cases in Germany per year).
- symptoms: palpable, painless induration within the scrotum, enlarged testicles (with heaviness), enlarged, sore breasts, in advanced stages additional symptoms due to secondary tumors (metastases) such as coughing and chest pain in lung metastases
- Treatment: Removal of the affected testicle; thereafter depending on tumor stage and testicular cancer form monitoring strategy (“wait and watch”), chemotherapy or radiotherapy; possibly removal of affected lymph nodes
- Forecast: Testicular cancer is generally very treatable. Most patients can be cured.
Testicular Cancer: Symptoms & Early Detection
The same applies to testicular cancer (testicular carcinoma) as to other types of cancer: the sooner the malignant tumor is discovered and treated, the better the chance of recovery. But how do you recognize testicular cancer?
Tactile hardening
One of the common testicular cancer symptoms is a painless hardening within the scrotum: The surface of the testicle feels nodular or tubercular. Any man can even feel a hard knot in his testicles (possibly testicular cancer) if he regularly self-examines himself. It is important to compare the modified testicles with the second testicles. That’s because differences can be better detected.
In about 95 percent of all cases, testicular cancer affects only one of the two testes. In the remaining five percent of patients, cancer cells develop in both testes.
Increase in size and heaviness
If a testis enlarges, this is also a possible testicular cancer sign. Most patients report this symptom the first time they go to the doctor. This increase in size may be due to the tumor growth itself. On the other hand, the reason may be an accumulation of liquid (hydrocele or water breakage).
By increasing the size of the affected testicles feels difficult. This heaviness goes with some sufferers with one Pull which can radiate into the groin.
Pain
In some patients are Pain in the area of the testicle more testicular cancer symptoms. Bleeding within the cancerous tissue can cause stinging or squeezing. However, pain is rarely the first sign of testicular cancer.
In case of pain in the area of the testicle, one should not immediately think of testicular cancer! Usually it is a testicular inflammation (orchitis) or epididymitis (epididymitis) behind it. An examination with the urologist brings certainty.
In advanced testicular cancer, the lymph nodes in the posterior abdominal cavity increase. That can back pain cause.
breast growth
Some testicular tumors produce female hormones. For example, elevated levels of estrogen in the blood can be detected in some patients. The pregnancy hormone beta-human chorionic gonadotropin (β-HCG) is also produced by some testicular tumors. As a result of hormone production, the male’s breast enlarges (one or both sides). Doctors talk about one with this testicular cancer symptom real gynecomastiabecause the glandular tissue in the breast actually proliferates here. In contrast, gynecomastia describes a breast growth caused by fat deposition.
The β-HCG is also considered a major tumor marker. This is a blood count that is typical of some testicular cancers. It helps to diagnose testicular cancer and to assess the course of the disease.
The enlarged breasts can also pain.
Symptoms due to cancer colonies
If testicular cancer progresses, cancer cells can spread throughout the body via lymphatic and blood vessels and form new tumors somewhere. Such dislocations (metastases) of testicular cancer occur mainly in the lungs on. But it can also affect other organs, such as the brain, bones and liver. Depending on the affected organ corresponding complaints occur.
For example, lung metastases often cause coughing (sometimes with bloody sputum) and shortness of breath. Even chest pain is then common symptoms. Testicular cancerous lesions in the bones cause bone pain. Among other things, liver metastases can become noticeable through nausea, loss of appetite and unwanted weight loss. If cancer cells in the brain spread, neurological deficits can be added to the common signs of testicular cancer.
Testicular cancer: treatment
In principle, the following treatment measures are available for the testicular cancer therapy:
- surgery
- Surveillance strategy: “wait and see”
- Radiotherapy (radiation)
- chemotherapy
The attending physician will suggest a customized treatment plan to a testicular cancer patient. Patients should ask the physician to join the project “Second opinion testicular tumors” (www.zm-hodentumor.de) to participate. In this internet-based project, physicians can ask testicular cancer specialists to make a second assessment of a patient’s findings and planned therapy. This can significantly improve therapy planning, if necessary.
The first step of the testicular cancer treatment is usually surgery. The further treatment steps depend on the stage of the disease and the type of tumor (seminoma or non-seminoma – by far the most common forms of testicular cancer).
Testicular cancer: surgery
In testicular cancer surgery, the affected testes, epididymis and spermatic cord are surgically removed. Doctors speak of the Ablatorio testis or orchiectomy, In a few cases, a testicular cancer can also be operated so that part of the testicle is preserved. This can then continue to produce hormones. This procedure is especially useful for patients who only have one testicle. To be on the safe side, the operated testes usually have to be irradiated afterwards.
At the request of the patient, a granule-sized tissue sample can be taken from the other testicle during the procedure and examined immediately under the microscope. This is advisable because in approximately five percent of the patients also in the second testicle, pathologically altered cells can be found. In this case, this testicle can be mitentfernt same.
The remote testicle can be replaced by a prosthesis at the request of the patient. For this purpose, a silicone pad is used in the appropriate size and shape in the remaining scrotum. If chemotherapy is needed after the testicles have been removed, the testicular prosthesis is still to be used.
tumor stages
The removed testicular cancer tissue is examined histologically. Together with other examinations (such as computed tomography) it is possible to determine the stage of the disease (see below: examinations and diagnosis). There are roughly different tumor stages:
- Stage I: malignant tumor only in the testicle, no metastases.
- Stage II: infestation of adjacent (regional) lymph nodes, but no distant cancerous lesions (distant metastases); Depending on the size or number of affected lymph nodes, stage II is subdivided further (IIA, IIB, IIC).
- Stage III: also distant metastases present (such as in the lungs); depending on severity further subdivision (IIIA, IIIB, IIIC).
seminoma
The most common form of testicular cancer is the seminoma. In the early stage (stage I), the further treatment after the testicle removal is often limited to the monitoring strategy: The patient must have a regular check-up on whether the cancer has returned. At first, these follow-up examinations are very closely scheduled. Later, the time intervals between them can be increased.
To improve the prognosis, one can also have an early-stage seminoma after surgery Chemo- or radiotherapy to treat. If the seminoma is already advanced at the time the testicles are removed, patients receive either chemo- or radiotherapy after surgery for all cases. Which form of therapy is the best option in an individual case depends, among other things, on the exact tumor stage.
In principle, it is also possible to combine radiotherapy and chemotherapy. This therapy variant is currently being tested in clinical trials in a seminoma.
Read more about the treatment of seminoma and other important information about this most common testicular cancer form in the article Seminom.
Nonseminoma
Non-seminomas are the second most common type of testicular cancer after seminomas. Here, too, the treatment steps after the testicle removal depend on the tumor stage:
Testicular Cancer Stage I
At this early stage in non-seminomas (as in seminomas) after the testicle removal is usually enough monitoring strategy out: With the help of regular check-ups possible relapses can be detected and treated early.
By definition, testicular cancer is limited to the testes in stage I and has not yet spread to lymph nodes or other body regions. However, this can not be said with 100% certainty, despite modern imaging techniques such as computed tomography. Sometimes cancerous metastases are so small that they are not detected in imaging. Two factors may indicate such invisible (occult) metastases:
- When examining the extracted tumor tissue, it is found that the testicular cancer has broken into adjacent lymphoid or blood vessels. The risk of occult metastases then increases to about fifty percent.
- After tumor removal, the respective tumor markers in the blood do not fall off or even rise.
In such cases, there is an increased risk that the testicular cancer has already spread. For safety then after the testicle removal is not a surveillance strategy, but a chemotherapy (1 cycle) recommended: patients receive three chemotherapeutic agents for several days: cisplatin, etoposide and bleomycin (collectively referred to as PEB for short). It may also be advisable to remove the lymph nodes in the posterior abdomen (lymphadenectomy). Subsequently, the person concerned is closely monitored and controlled.
Testicular cancer stages IIA and IIB
In these two testicular cancer stages, lymph nodes are already affected and thus enlarged. Then there are two options for the further treatment after the testicle removal:
- Either the infested Lymph nodes surgically removed, possibly followed by a chemotherapy (if individual cancer cells should remain in the body).
- Or the patient receives immediately after the testicular operation three cycles of chemotherapy, After that you may still be afflicted Remove lymph nodes surgically.
Testicular cancer stages IIC and III
In these advanced nonseminomic stages, patients will be following the testicular removal three to four chemotherapy cycles treated. If there are still affected lymph nodes, they will be removed (lymphadenectomy).
Side effects of testicular cancer therapy
The chemotherapy Testicular cancer (and other forms of cancer) can have a number of side effects: The drugs (cytotoxic drugs) are very toxic to cells – not only for the testicular cancer cells, but also for healthy body cells such as platelets, blood cells and hair root cells. Possible side effects are therefore, for example, anemia, bleeding, hair loss, nausea and vomiting, loss of appetite, inflammation of the mucous membranes, hearing disorders and discomfort on the hands and feet. Cytostatic drugs also attack the immune system. Patients are therefore more susceptible to pathogens during treatment.
As a rule, these side effects disappear after completing chemotherapy. In addition, doctors can help with appropriate measures and tips to alleviate the undesirable effects of treatment (such as nausea remedies).
In a (suspected) lymph node involvement in the posterior abdomen, this region is often with a radiotherapy treated. The most common side effect here is mild nausea. It occurs several hours after the radiation and can be relieved with medication. Other potential side effects include transient diarrhea and skin irritation in the treatment area (such as redness, itching).
Testicular cancer: causes and risk factors
Testicular cancer (testicular carcinoma) in adult males is found in more than 90 percent of the germinal cells in the testes. you will be Germ cell tumors (germinal tumors) called. The small remainder do non-germinal tumors out. They arise from supporting and connective tissue of the testicle.
Germ cell tumors: seminomas and non-seminomas
The germ cell tumors are divided into two main groups: the seminomas and the non-seminomas.
One seminoma is the result of degenerated sperm stem cells (spermatogonia). It is the most common form of malignant germ cell tumor in the testes. The average age of the patients is around 40 years.
The term Nonseminoma includes all other germinal testicular cancer forms that arise from other tissue types. They include:
- Yolk sac tumor
- choriocarcinoma
- embryonic carcinoma
- Teratoma or the malignant form teratocarcinoma
Patients with a non-seminoma are on average 25 years old.
The precursor of seminomas and non-minors will be testicular intraepithelial neoplasia (TIN) called (intraepithelial = located within the covering tissue, neoplasia = neoplasm). The neoplasms originate from embryonic germ cells before birth. They rest in the testes and can later develop into testicular cancer.
Non-germinal tumors
Much rarer than the germ cell tumors are the non-germinal tumors (germinal tumors, gonadal stroma tumors). These are cell proliferations that arise from the supporting and connective tissue cells of the testicle. They are either benign or malignant. The most important representative of malignant germinal tumors is the Leydig cell testicular cancer, He comes from the Leydig cells. They produce the sex hormone testosterone and thus stimulate sperm production.
Non-germinal tumors are mainly found in children. In adult men, they are very rare (most likely in old age).
Why does testicular cancer arise?
The exact cause of testicular cancer is not yet known. However, researchers have identified some risk factors for its development in the past.
Former testicular cancer disease
An earlier testicular cancer disease is the most important risk factor: anyone who has had testicular cancer has a 30-fold increased risk of developing a malignant testicular tumor again.
Undescended testicles
Normally the two testicles migrate from the abdominal cavity into the scrotum during development of the fetus (sometimes even after birth). On the other hand, one testicle remains at one testicle elevation (Maldescensus testis) or both testicles remain either in the abdominal cavity or in the groin (abdominal or inguinal testes). Sometimes the testes can be found at the testicular entrance and can be pushed under pressure into the scrotum, but slides back immediately. Then one speaks of sliding horseshoe.
An undescended testicle increases the likelihood of developing testicular cancer. This risk still exists even when the undescended testicles have been surgically corrected: Thus, the testicular cancer risk is 2.75- to 8-fold higher in operated high height than in a normal testicular system. In particular, in the sliding horsetode the risk of degeneration depends on the duration of the misalignment. Above the scrotum, the body temperature at 35 to 37 degrees Celsius is significantly higher than in the scrotum (about 33 degrees Celsius). The higher temperature can damage the testicular tissue. Therefore, the risk of testicular cancer is increased at (previous) undescended testicles.
Wrong attachment of the urethra mouth
If the mouth of the urethra is below the glans (ie on the underside of the penis), doctors speak of hypospadias. Studies suggest that the risk of testicular cancer is increased by this miscarriage.
Hypospadias and undescended testicles appear to have a similar genetic cause. They therefore often come together. However, they can also occur separately.
Genetic factors
Studies have also shown that hereditary factors most probably influence the development of testicular cancer. Because the same tumor occurs frequently in some families. Affected brothers have an up to twelve-fold increased risk of developing testicular cancer as well. Even sons of sick fathers are statistically more likely to develop testicular carcinoma than sons of healthy fathers.
In addition, it has been found that testicular cancer is much more common in fair-skinned European-born men than in African-born men.
Estrogen excess in pregnancy
By far the most common form of testicular cancer (germ cell tumors) arises from a precursor called TIN (testicular intraepithelial neoplasia). It is based on germ cells that develop in the embryo before birth. One of the reasons for this is hormone imbalance during pregnancy, more precisely, an excess of female hormones (estrogens). This can most likely disrupt the testis development of the unborn child and lead to the precancerous TIN.
For example, a slight excess of estrogen is observed in pregnant women who are expecting the first child or twins or older than 30 years. Taking medicines with estrogens can increase the hormone levels in pregnant women. However, pregnant women today are hardly treated with hormones.
infertility
Even with a man unable to produce the testicular cancer risk is increased. Infertility is based either on underdeveloped testes (hypogonadism) or on a deficiency or complete absence of sperm in the seminal fluid (oligospermia or azoospermia).
The causes of infertility can be different. Sometimes it is the result of an orchitis caused by the mumps virus. Even deviations (anomalies) in the genome can make men infertile, for example, the Klinefelter syndrome.
External influences
Worldwide, the number of testicular cancer diseases has increased significantly in the last 20 years. Experts therefore suspect that external influences in childhood and early adulthood also favor the development of cancer. But that needs to be explored more closely.
Testicular cancer: diagnosis and examination
Men should regularly examine and feel their own testicles, especially between the ages of 20 and 40 years. Anyone diagnosing a change in the scrotum should quickly consult a urologist. This specialist in urinary and genital organs can clarify the suspicion of testicular cancer by means of a few examinations.
Doctor-patient conversation
First, the doctor talks in detail with the patient to raise his medical history (anamnesis). The doctor asks for any symptoms, for example:
- Have you noticed a hardening in the scrotum?
- Do you feel a feeling of heaviness at the said place or even pain?
- Have you noticed any other changes to you, such as a breast size increase?
In the conversation, the doctor will also clarify possible risk factors: Have you had a testicular tumor in the past? Did you have an undescended testicle? Is someone in your family suffering from testicular cancer? Every piece of information is important, even those that seem insignificant to the patient. For example, swelling in the groin, back pain or cough may indicate cancerous deposits (metastases) and thus an advanced testicular cancer.
Palpating testicles
The anamnesis interview is followed by a physical examination. Especially the bimanual examination of the testicles is important. In doing so, the doctor holds the testicle firmly with one hand while scanning it with the other for irregularities. In this way, both testicles are carefully examined, even if only one suspicious changes. The site comparison can provide important information (testicular cancer usually only affects one testicle alone). When palpation examination applies: Any enlargement or hardening in and on the testes is suspected tumor.
Tip: Every man should regularly feel his own testicles. So he can detect suspicious changes early and see a doctor. If it really is testicular cancer, an early diagnosis improves the chances of recovery!
How to proceed in the self-examination of the testicle, you will read in the review testicles.
Palpation of the breast
As part of the physical examination of the doctor is also suspected of testicular cancer in the chest of the man. The female hormones produced by a testicular tumor cause the mammary glands to swell painfully.
Ultrasonic
The ultrasound examination for the diagnosis of testicular cancer is carried out with a high-resolution probe. Typical are irregular areas that appear darker than the surrounding tissue. Even smaller and non-palpable testicular cancer foci can be detected in the ultrasound. The examination is carried out on both testes in order to be able to rule out a bilateral infestation.
blood test
If testicular cancer is suspected, a comprehensive examination of the blood is also important. The doctor wins it for a reference to the General condition of the patient and on the Function of individual organs, On the other hand, so-called tumor markers in blood. These are proteins that are either detectable only in the case of cancer or are produced in cancer patients in strikingly increased quantities.
One such tumor marker in testicular cancer is the alpha-fetoprotein (AFP), This protein is produced during pregnancy in the yolk sac of an unborn child. In adults, it is only produced in very small quantities of liver and intestinal cells. If a man has an elevated AFP value, this indicates testicular cancer – especially certain forms of non-seminomas (yolk sac tumor and embryonic carcinoma). For a seminoma, on the other hand, the AFP value is normal.
Another important tumor marker in testicular cancer is the beta-human chorionic gonadotropin (β-HCG), Its value is above all increased in choriocarcinoma (a form of non-seminoma), in a seminoma, however, only in about 20 percent of all cases.
The Lactate dehydrogenase (LDH) is an enzyme that also occurs in many body cells. It is only suitable as a complementary tumor marker (besides AFP and β-HCG) in testicular cancer.
The blood value of placental alkaline phosphatase (PLAP) is especially elevated at a seminoma. Since the value is also increased in almost all smokers, PLAP is only very limited as a tumor marker in testicular cancer.
These tumor markers are not elevated in every testicular cancer patient. Conversely, healthy persons may also have elevated values. The tumor markers alone therefore do not permit a reliable diagnosis. But they are suitable to assess the course of a testicular cancer disease. If, for example, the tumor markers rise again after a completed treatment, this can signal a relapse (recurrence).
CT and MRI
If the diagnosis of testicular cancer is confirmed, computed tomography (CT) provides information about the spread of the tumor: X-rays are used to produce detailed cross-sectional images of the pelvic, abdominal and thoracic cavities and possibly the head. On top of that, enlarged lymph nodes as well as testicular cancer metastases (dislocations of the tumor in other parts of the body) are generally easy to recognize. Typically, the patient is injected with a contrast agent prior to examination to improve imaging.
An alternative to CT is MRI (Magnetic Resonance Imaging, MRI): it also provides detailed cross-sectional images of the body’s interior, albeit using magnetic fields (not X-rays). The patient is therefore not exposed to radiation. An MRI is performed, for example, if the patient is allergic to the contrast agent that should be used in CT.
Exposure of the testicle
To ensure a testicular cancer diagnosis, the suspected testis is surgically exposed. The doctor then usually recognizes with the naked eye whether a malignant testicular tumor actually exists. If in doubt, he will take a tissue sample that will be examined for cancer cells during the procedure. If so, it will be checked if it is Seminom or non-Seminom. In the case of testicular cancer, the affected testis is immediately removed.
Testicular cancer: disease course and prognosis
Testicular cancer can usually be treated well and usually also be cured. Five years after a testicular cancer diagnosis still about 96 percent of patients (5-year survival).
This good prognosis is mainly due to the fact that in most patients the testicular carcinoma is detected at an early stage. The chances of success of the treatment are then high. However, if the cancer has already spread at the time of diagnosis, this worsens the chances of recovery. However, the prognosis in individual cases is also influenced, for example, by …
- what type of tumor is present (seminomas generally have a more favorable prognosis than non-seminomas)
- how well the patient responds to the therapy
- where metastases have already formed in the body (for lymph node and lung metastases the prognosis is usually more favorable than for metastases in liver, bone or head)
- how long after the last chemotherapy lasts until the cancer progresses again (the longer, the cheaper)
- which measured values the tumor markers have
Bullet fertility
Many patients fear by treating testicular cancer barren to become or no sexual desire to feel more. Most of the time, however, the attending physician can calm those affected: the majority of patients only have them unilateral testicular cancer, Then only the diseased testicles have to be removed. The remaining testes are usually sufficient to maintain sexuality and fertility. However, seed production may be somewhat impaired afterwards. In addition, there are men in whom sperm production is compromised even before the disease and treatment.
More importantly, the issues of fertility and sexual publishing are mostly for the (few) patients who are under bilateral testicular cancer suffer or from a previous illness already lost a testicle, The operation then attempts to remove only malignantly altered tumor tissue and to obtain as much testicular tissue as possible. However, if it is necessary to completely remove both testicles (or the only existing testes), the affected person can no longer produce children. The sex hormone testosterone is no longer produced. Its absence reduces sexual desire and erectile function.
Basically, all testicular cancer patients before the start of treatment recommended, your own Examine fertility allow. This is best done by analyzing a sample of ejaculation in the laboratory for the number, shape and buoyancy of the sperm (semen analysis). Alternatively, one can also measure the blood FSH (follicle-stimulating hormone): If it is increased, this may indicate a reduced sperm production.
Also, before the start of treatment, testicular cancer patients should consider whether they are safe Freeze sperm want to leave (cryopreservation). This will later enable artificial insemination if the patient is naturally unable to reproduce after the testicular cancer treatment. For the preservation (350, – to 650, – Euro) and storage (200, – to 450, – Euro per year) you usually have to pay yourself.
Tip: Patients should ask in advance in person at their own health insurance, if this does not take over the costs. Sometimes cash registers make an exception.
This after a testicular cancer surgery missing testosterone can be replaced by syringes, tablets, gel preparations or patches.
Testicular cancer: relapse
In order to be able to detect a possible testicular cancer relapse (relapse) at an early stage, successfully treated patients are regularly examined. At first, the check-ups are very tight. Later, the time intervals between them get longer. This is especially true when there are no symptoms and no signs of a possible relapse.
The likelihood of a testicular cancer relapse depends especially on Tumor stage at the first diagnosis and from the Type of first treatment from. For example, if testicular cancer is only monitored in the early stage after surgery (surveillance strategy), the risk of relapse is higher than with post-procedure chemotherapy.
If it comes to a relapse, then usually within the first two to three years after the first treatment. Later recurrences are rarer. The patients then receive a so-called Salvage chemotherapy: This is a high-dose chemo. It is much more effective than a normal dose of chemotherapy normally used in the initial treatment of testicular cancer. But she has more serious side effects. Unter anderem werden das Knochenmark und damit die Blutbildung bei der Hochdosis-Therapie viel starker geschädigt. Deshalb werden den Patienten meist blutbildende Stammzellen übertragen (Stammzelltransplantation):
Die Patienten bekommen zuerst eine normal dosierte Chemotherapie, um möglichst viele Krebszellen abzutöten. Dann verabreicht man ihnen Wachstumsfaktoren, welche die Blutbildung anregen. So entstehen ausreichend Stammzellen, die sich aus dem Blut des Patienten herausfiltern lassen. Nach der hochdosierten Chemotherapie (Salvage-Chemotherapie) werden den Patienten dann die entnommenen Blutstammzellen wieder über eine Vene zurückgegeben. Die Stammzellen siedeln sich im geschädigten Kncohenmark an und beginnen, neue Blutzellen zu produzieren.
Insgesamt gilt: Ein Rückfall ist bei Hodenkrebs eher selten. Auf die dann verabreichte Hochdosis-Chemotherapie sprechen 50 bis 70 Prozent der Patienten günstig an.
Additional information
Selbsthilfegruppe:
- Deutsche Krebsgesellschaft