A ganglion is also called Überbein. A somewhat misleading name: It is not an ossification, but a fluid-filled outward opening of a joint or tendon sheath. Mostly it forms in the hand. But it can also occur on the foot or knee. Apart from the fact that a ganglion does not look so pretty, it usually does not cause any discomfort. Read here, among other things, how a hypnotic arises, how to recognize it and how to get rid of it!

Summary
- What is a high leg (ganglion)? A fluid-filled, sac like cavity on the joint, usually on the hand, rarely on the knee, foot or spine
- symptoms: Prelastic buckling of a few millimeters to a few centimeters in diameter, possibly pressure pain, reduced mobility or numbness, but often no complaints
- Causes: Not known exactly. Probably connective tissue weakness and risk factors such as joint disease or increased joint strain play a role.
- Doctor treating: Orthopedist or surgeon
- Diagnosis: Patient talk, physical examination, possibly imaging techniques and fine needle aspiration
- Treatment: if necessary, only observation and physiotherapy, otherwise surgery or aspiration possible
- Forecast: usually favorable course, but ganglia often return
Ganglion: description
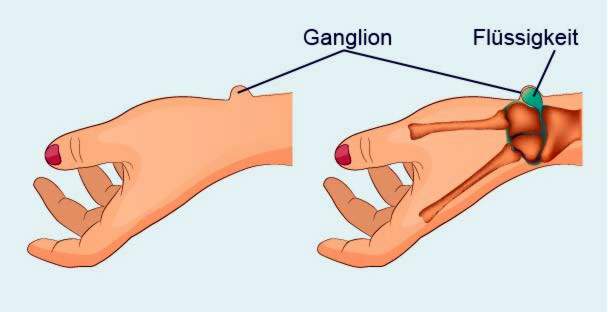
Ganglion is the medical term for a high leg. This term is a relic from the time when it was assumed that it was a bony structure. In fact, a ganglion is a cystic outgrowth, that is, a cavity filled with fluid, usually at joints (Arthrogen) arises. Ganglia are connected by a kind of spout to the joint, which is why they can hardly be moved.
Ganglia occur most frequently in the hand (in about 65 percent of cases): The ganglion arises here especially on the back of the hand. Sometimes, fingers or wrists are also affected. Less often, there is an overbone on the hips, knees, feet or spine.
Rarely can a ganglion also occur on the tendon sheaths (tendinogen). In this case we also speak of a tendon sheath ganglion. Another special form of the overbone is the so-called intraosseous ganglion, which forms in a bone. It therefore bulges inwards instead of outwards.
In principle, people of all ages can get a high leg, even children. Most often, however, it occurs between the ages of 20 and 30 years. Women are affected more often than men. Its reasons are its naturally weaker connective tissue and more flexible joint capsules.
Ganglion: symptoms
Affected people usually notice one bump on the wrist or the back of the hand, more rarely on other parts of the body. It can also form several overbites.
The “bump” on the wrist or other parts of the body is typical plump elastic, He has a diameter on average from a few millimeters to two centimeters, But there are also ganglia, which are up to eight inches tall. Some also remain so small that the person concerned does not even notice the protuberance and it is only discovered by accident.
Typically, a ganglion does not cause any Pain and makes itself otherwise hardly noticeable. However, depending on size and location, it can limit the mobility of the joints and muscles, or hurt when the person is leaning on it. The (pressure) pain can also radiate. The ganglion can also hurt when moved or touched.
If an over-leg presses on tendons, it can squeeze them and, due to the permanent load, possibly one inflammation (Tendonitis).
Numbness, tingling, or weakness in the hand can be an indication that the ganglion is one Nerve “disconnected”, Often the nerves are in so-called Annular ligament ganglia affected. These are small over-legs on the ring bands of the fingers, which can complicate the bending and stretching. But also wrist, or foot (back) are prone to squeezed nerves and vessels. The pressure on vessels can too bleeding to lead. Also, in the fluid-filled space of the ganglion infections spread.
Ganglion: causes and risk factors
The exact causes of a ganglion are not yet known. Several factors probably play a role in the development of an overbone. That could be for example one connective tissue be:
Around the joints lies (solid) connective tissue, the so-called joint capsule. This keeps the joint in position and ensures that it only moves in the desired direction. In the joint, a soft layer of connective tissue (synovial membrane) like a wallpaper clothes the joint cavity. In the joint cavity is gall-like fluid (“joint lubrication”) without which the bony parts of the joints would rub against each other.
In connective tissue weakness, in conjunction with an overstressing of the joint, synovial fluid may leak out of the joint cavity and collect in the surrounding soft tissue. This creates a ganglion, experts suggest.
To the Risk factors for a ganglion counting:
- increased joint loads as by repeated small injuries of the capsule and the ligaments
- Disorders of biomechanics of the joint or tendon
- Joint diseases and rheumatic diseases (such as osteoarthritis, lupus erythematosus, gout)
About ten percent of the patients suggest getting to the site of the ganglion before injured to have. In addition, in a ganglion, those are likely to stimulate connective tissue cells (Fibroblasts) the production of synovial fluid. Their components hyaluronic acid and so-called mucopolysaccharides form a viscous fluid, which then accumulates in the overbone.
In addition, probably also play Wear-related damage to the fabric a role in the formation of a ganglion.
Ganglion: examinations and diagnosis
Go to an orthopedist or surgeon if you suspect a ganglion. He may be able to exclude underlying diseases such as osteoarthritis as a trigger of Knubbels. The best way to find a doctor who has specialized in the affected body region, so for example, a hand surgeon with a high leg on the hand.
To clarify the suspected ganglion, the doctor usually proceeds as follows:
Collection of medical history: In conversation with the patient, the doctor inquires about the exact complaints as well as possible injuries and basic or previous illnesses. Possible questions of the doctor in this anamnesis interview are for example:
- When did you notice the swelling for the first time?
- Does the swelling affect the mobility of the affected part of the body or does it cause pain?
- Did you ever get hurt at the affected area?
- Did you have similar “Knubbel” before?
- Are there similar swellings elsewhere?
Physical examination: Afterwards, the doctor examines the swelling to be able to assess it more accurately. A ganglion feels like a ball of rubber, similar to a solid rubber ball. It can be moved only slightly by its anchoring to the joint or tendon sheath. In contrast to highly inflammatory processes, the affected region is neither overheated nor reddened. Maybe the doctor will take some photos for documentation.
In addition, he will examine blood circulation, motor skills and sensitivity in the area of the affected body region. For example, he can detect movement restrictions due to the ganglion, circulatory disorders and nerve damage. Also a “transillumination” of the swelling (transillumination) is possible: by illuminating the ganglion with a light source from the side, the doctor can determine whether the interior is fluid (reference to ganglion, cyst) or solid.
imaging: Imaging procedures are uncommon in ganglia. They are only used when the case is unclear and there is suspicion of a malignant process or arthritis, for example. Even if the doctor suspects a “hidden” ganglion, ultrasound and magnetic resonance tomography (magnetic resonance imaging, MRI) can confirm or invalidate this suspicion.
Fine-needle aspiration: For diagnostic as well as therapeutic purposes, the physician can ultrasonically pierce the ganglion with a very thin, hollow needle to extract fluid from within. This mostly viscous but clear fluid is then examined by a pathologist in the lab. This makes it possible to exclude inflammation or even malignant processes. Draining fluid from the ganglion causes it to visibly contract. But in most cases this is not a permanent solution.
Ganglion: treatment
If a ganglion causes no discomfort, it does not necessarily need to be treated. Some ganglia disappear after some time by themselves again.
However, many sufferers feel that they are overly bothersome or have discomfort (such as pain in certain movements, limited mobility). Then a treatment is advisable. Basically, there are three ways to treat an overbone: conservative treatment, aspiration, and surgery. Which method is used in an individual case depends on several factors, such as the position of the ganglion. The wishes of the patient are also taken into account in the planning of ganglion therapy.
The so-called Bible or hammer therapy is not recommended! This brute (self-therapy) method was once often used in ganglia. You try to smash the bumblebee with a bible or a hammer. Therefore, the name “Bible cyst” for ganglia. In the worst case, bones break.
Conservative treatment
A ganglion that does not affect the affected person can simply be observed at first. Maybe the overbone spontaneously forms spontaneously or by physiotherapy alone. Resting can prevent it from getting bigger. In addition, it is important to avoid stress on the affected joint. After about three months of conservative treatment, the doctor discusses with the patient in most cases, how the therapy should be continued.
aspiration
Aspiration, such as the doctor may have already used to diagnose, can also be used therapeutically. In this form of ganglion treatment, the doctor pricks with a fine hollow needle into the over-leg and sucks off the liquid contained (needle puncture). Usually, however, new fluid accumulates within a short time (ganglion recurrence).
Therefore, the doctor sometimes injects corticosteroids after aspiration (cortisone) into the “deflated” ganglion. It should prevent a renewed swelling.
Another possibility is the enzyme hyaluronidase to inject into the ganglion. It breaks down the main component of the contained liquid (hyaluronic acid). Thereafter, the doctor aspirates the liquid by aspiration.
surgery
The surgical removal of a ganglion is considered very promising when performed by an experienced specialist. The surgeon removes the over-leg and tries to close the joint in such a way that no liquid escapes. A ganglion surgery can in principle open (over a larger incision) or minimally invasive (arthroscopic). As a rule, only a local or regional anesthetic is necessary for the over-leg surgery.
In some cases, such as a ganglion finger, a ganglion wrist or a ganglion foot or a ganglion back of the foot, a so-called tourniquet may be applied during the procedure. It reduces blood flow to the affected area and thus the risk of major bleeding. Care must be taken to ensure that the ganglion is completely removed (without residues) and that important environmental structures such as vessels, nerves or tendons remain intact.
After surgery, the operated area should first be spared and sedated. The patient may need to wear a splint for some time. Accompanying physiotherapy can help prevent stiffening of the joint.
Complications of a ganglion surgery
Every tenth open surgery causes complications. On the other hand, arthroscopic procedures and aspiration procedures, with four or two percent, are much less likely to cause problems. Especially vascular (bleeding) and nerve injuries (deafness, paralysis) are more common in open surgery. In addition, there is a risk of infection, wound healing disorders and the development of Sudeck’s disease (a chronic pain syndrome). In addition, as with any surgery, a (small) scar remains.
Ganglion: Disease course and prognosis
A ganglion is a benign protuberance with a favorable course. It can spontaneously regress, but also enlarge. Mostly it causes no complaints. However, depending on the situation, it can cause pain or numbness or reduce the mobility of the affected joint.
If a ganglion has been treated successfully, there is a risk of recurrence (recurrence): a new ganglion may form in the same or another location. Surgery seems to be the most sustainable case of an overbone: Only in about one in five patients does a cystic protuberance form after an open surgery at the same site. In a minimally invasive operation, the risk of relapse is even lower. After aspiration treatment, half of the patients again develop an over-leg.
In order to prevent relapses, risk factors for ganglia should be reduced and the muscles should be relaxed and relaxed again and again during the day. This prevents overloading, the one ganglion can favor.