Colorectal cancer (colorectal carcinoma) is a malignant tumor of the colon or rectum. It usually arises from benign intestinal polyps. The only cure for colorectal cancer is surgery. Other methods such as chemotherapy or radiotherapy often support the treatment. Read here all important information on the topic: How to recognize bowel cancer? What are its causes and risk factors? How is colon cancer treated? How big are the chances of recovery?

Quick Overview
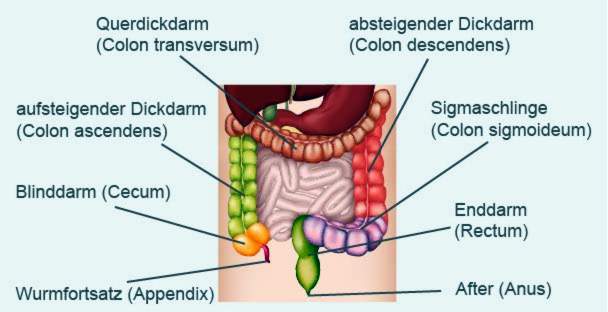
- What is colon cancer? Malignant tumor in the large intestine (colon carcinoma) or rectum (rectal carcinoma). In summary, doctors in colorectal cancer speak of a colorectal carcinoma.
- Frequency: In Germany, colon cancer is the second most common cancer in women and the third most common cancer in men. Every year, about 29,500 women and 33,500 men contract colon cancer. At diagnosis, patients are on average 73 years (men) and 75 years (women) old.
- symptoms: Colon cancer develops slowly, and usually stays for a long time without discomfort. Possible signs in the further course are altered bowel habits (diarrhea and / or constipation), blood in the stool, unwanted weight loss, anemia, possibly abdominal pain, mild fever, tiredness, poor performance.
- Causes and risk factors: poor diet (low fiber, high in meat and fat), physical inactivity, overweight, alcohol, nicotine, genetic factors, inflammatory bowel disease (especially ulcerative colitis), type 2 diabetes mellitus
- Treatment: Depends on several factors such as location, size and spread of the tumor. The most important therapy option is the operation. In support of further treatments can be initiated, such as chemotherapy or radiotherapy.
- Forecast: The early detection and treatment of colorectal cancer, the better the chances of recovery. If daughter tumors (metastases) have already formed in other body regions, the prognosis worsens.
Colon cancer: symptoms
Colon cancer usually goes unnoticed for a long time. Complaints only occur when the tumor has reached a certain size. Then he can interfere with the passage of food leftovers. As a result, the bowel movement changes (Constipation, diarrhea). Often there is also Blood in the stool.
Like any cancer, the tumor also weakens the entire body. Therefore, non-specific complaints can also be inefficiency, unwanted weight loss and optionally light fever occur. If the tumor has already spread to other organs at an advanced stage (metastases), further complaints may occur.
Below, you can read more about what you can detect colon cancer. But beware: The symptoms mentioned are not a clear sign of colorectal cancer, but may have other causes. But you should always have them checked out by a doctor. This is especially true when relatively young people experience potential colorectal cancer symptoms. Colon cancer is extremely rare in younger people.
Colon Cancer Symptoms: Modified bowel movements
Many patients suffer alternately under constipation and diarrheabecause the tumor narrows the intestine: The stool initially builds up in front of the tumor. Then it is liquefied by bacterial decomposition and excreted as sometimes foul-smelling diarrhea. This alternation of constipation (constipation) and diarrhea (diarrhea) is also called paradoxical diarrhea designated. It is a classic warning sign for colorectal cancer.
Some patients also suffer from repeated constipation or recurrent diarrhea.
If additionally unwanted stool is excreted at the departure of winds, this may also be an indication of colon cancer. Doctors speak of this Phenomenon of the “wrong friend”, It arises when the muscle tension of the anal sphincter is reduced. The reason for this can be a deep-seated colon cancer, which traverses the muscle and thus interferes with its function.
In general, any change in bowel habits that persists for more than three weeks should be clarified by a doctor for people over the age of 40 years.
Colon cancer symptoms: blood in the stool
A malignant tumor is not as stable as healthy tissue. That’s why he often bleeds. In colon cancer, this blood is excreted together with the stool. Thus, in the majority of colon cancer patients blood admixtures in the stool.
These blood enemas are sometimes visible to the naked eye, The color gives an indication of the location of the tumor: If the colon cancer is located in the area of the rectum, the blood in the stool appears red (fresh blood). In other cases, the stool is stained pitch-black by older (dark) blood. This so-called tarry stool indicates a bleeding in the upper digestive tract (stomach, duodenum). However, it can not be ruled out that Teerstuhl also occurs in a source of bleeding in the colon.
However, many colon cancer patients excrete so little blood that it does not stand out in the stool. These “Invisible” blood admixtures are also called occult blood designated. It can be detected with certain tests (eg Hämoccult test).
Despite its frequency, blood is in the stool no specific colorectal cancer signs, There may be other causes behind it. Most blood residues on the chair or toilet paper are due to hemorrhoids. Typically, the blood is then more likely to be bright red and stored in the stool. The blood in colorectal cancer, however, is usually mixed with the stool due to the bowel movements.
In addition to hemorrhoids, bleeding sources in the esophagus, stomach or duodenum are also possible causes of blood in the stool (for example, a gastric ulcer).
General colon cancer symptoms
Colorectal cancer can also cause the general condition of a person to deteriorate. For example, those affected feel unusual tired and weak and are not as powerful as usual, Also fever can be a sign of colon cancer.
Especially in advanced disease can anemia (Anemia) occur. It arises because the malignant intestinal tumor often bleeds. Iron is also lost with the blood. However, as iron is necessary for the formation of the red blood pigment (hemoglobin), it causes anemia due to iron deficiency (iron deficiency anemia). It manifests itself with symptoms such as paleness, poor performance, tiredness and, in severe cases, respiratory distress.
Another colorectal cancer indication is in advanced stages unwanted weight loss, Doctors here speak of a tumor cachexia: Due to the cancer, the body builds up a lot of fat and muscle mass. Thus, the patients are increasingly emaciated and emaciated.
Other colorectal cancer signs
If the colon cancer has spread to other parts of the body (metastasis), more discomfort may occur. He often forms secondary tumors in the liver (liver metastases). This can, for example, cause pain in the right upper abdomen, jaundice or increased liver function in the blood. Also lung metastases are not uncommon in colon cancer. You may be affected by wheezing or difficulty breathing.
But colon cancer can also continue to grow in the intestine. He may damage the intestinal wall or surrounding tissue. For example, a large tumor can narrow the intestine so that food remains can not pass through it. This is how you get started bowel obstruction (Ileus) – a serious complication of colon cancer.
Pain can also occur in colorectal cancer, for example spasmodic abdominal pain. Some patients also have pain during bowel movements.
In some cases, patients report of strong bowel sounds and flatulence, Both can of course also occur in healthy people. However, when these symptoms accumulate, sometimes they are signs of colorectal cancer.
With further growth, the tumor can break through the intestinal wall and one Peritonitis (peritonitis) cause. If the cancer cells in the abdominal cavity spread on the peritoneum, doctors speak of one peritoneal.
Colon cancer: rectal cancer
Rectal carcinoma (rectal cancer or rectal cancer) usually develops from cells of the mucous glands in the wall of the rectum (rectum). Then one speaks – considered in terms of histology – of a so-called adenocarcinoma.
Rarely developed rectal cancer (endemic) from other cell types. For example, when supportive tissue cells degenerate and become cancerous cells, they form sarcoma, In contrast, a neuroendocrine tumor emerges from so-called neuroendocrine cells. These come from the nervous system and release hormones or other messengers.
Rectal cancer is usually removed surgically. Depending on the stage of the tumor, patients additionally receive radiotherapy and / or chemotherapy.
Read more about this form of colon cancer in the article Rectal Cancer.
Colon cancer: causes and risk factors
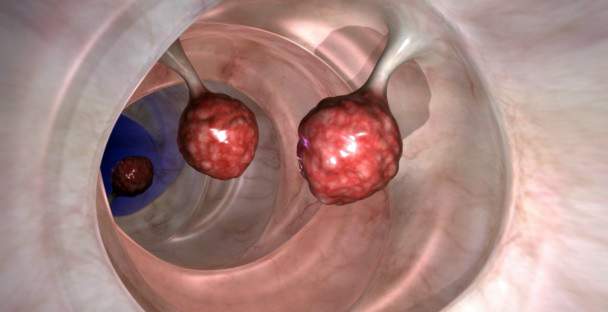
Colon cancer arises in most cases from benign growths of the intestinal mucosa. For many people, these so-called polyps harmless. Others, on the other hand, continue to develop colon cancer.
Intestinal polyps usually result from cells of the mucous glands in the intestinal wall. They are among the so-called adenomas. Colorectal cancer, which develops from such benign adenomas, belongs therefore to the adenocarcinomas (Carcinoma = cancerous tumor). Rarely, intestinal polyps and thus developing cancerous tumors from other cell types arise.
The development of normal intestinal mucosa on the polyp formation to the development of colorectal cancer is slow – it takes years. It is triggered by the current state of knowledge different risk factors, Among other things, certain nutritional and lifestyle habits as well as hereditary factors are among the possible causes of colorectal cancer.
Diet and lifestyle
A Low-fiber, high-fat and meat-rich diet (especially red meat and processed sausages) increases the risk of colorectal cancer. Such food passes through the intestine more slowly than plant-based, fiber-rich food. Thus, carcinogenic substances in the food remain in contact with the intestinal mucosa longer and can damage them, experts suggest.
lack of exercise and overweight also favor the development of colorectal cancer. Also Alcohol and nicotine increase the risk of colorectal cancer (and other cancers).
Genetic factors
In some cases, colon cancer is inheritable. For example, it can be observed that first-degree relatives (parents, children, siblings) of colorectal cancer patients are more likely to develop this type of cancer than other people.
First, there are genetic predispositions that do not directly increase the risk of colorectal cancer, but make those affected more susceptible to colorectal cancer risk factors (such as meat-rich diets). So here is the combination of heredity and lifestyle the trigger for the development of colon cancer.
On the other hand, there are gene mutations (mutations) that directly promote the formation of a malignant tumor in the intestine. In the meantime, some hereditary diseases are known that increase the risk of colorectal cancer. Two examples:
- HNPCC (Hereditary Non-polypous Colon Carcinoma Syndrome or Lynch Syndrome): This is the most common form of hereditary colon cancer. Due to mutations, various repair systems for the genetic material are defective here. This significantly increases the risk of colorectal cancer and other cancers (such as uterine, ovarian and stomach cancers).
- FAP (familial adenomatous polyposis, FAP): In this rare disease countless polyps form throughout the intestine. They are very likely to become colon cancer over the years. Therefore, sufferers must be regularly examined for colorectal cancer from childhood. Often, as a precaution, intestinal sections are surgically removed to prevent colon cancer in FAP.
Other risk factors for colorectal cancer
Age also has an important impact: the older someone is, the higher their risk of colorectal cancer. 90 percent of all colon carcinomas occur after the age of 50 years. However, the rarer genetic colorectal cancer often occurs at a young age. For example, people who develop colon cancer at the age of 30 usually find typical genetic changes.
The colorectal cancer risk is also elevated when someone is at one chronic inflammatory bowel disease suffers. Above all, people are affected Ulcerative colitisIn them, the colon is chronically inflamed. The more extensive the inflammation and the longer the disease duration, the higher the risk of colon cancer. Also at Crohn’s disease the risk of colon cancer may be increased. This is especially true when the chronic inflammation affects the large intestine (but it is usually limited to the last small intestine section).
People with the Type 2 diabetes (Type 2 diabetes mellitus) have elevated levels of insulin in the blood during the initial stages of the disease. In the opinion of doctors, these are responsible for the fact that the risk of colorectal cancer is about three times higher. Insulin generally promotes the growth and proliferation of cells – including cancer cells.
Pre-colon cancer protective factors
In addition to the mentioned risk factors for colorectal cancer, there are also influencing factors that protect against colon cancer. These include regular physical activity and a fiber-rich, low-meat diet. The movement and the fiber stimulate the intestinal movements. The food remains are transported faster through the intestine. For example, toxins in the stool can have less effect on the intestinal mucosa – the risk of bowel cancer falls.
Colon cancer: examinations and diagnosis
If you have a suspected colon cancer, you should first contact your family doctor. If a colonoscopy makes sense, he will refer you to a gastroenterologist.
The doctor will first talk to you in detail about your To raise medical history (Anamnese). He describes exactly your complaints. He also collects information that helps him better understand the likelihood of colorectal cancer. Possible questions of the doctor in the anamnesis interview are:
- Has your digestion changed (eg constipation or diarrhea)?
- Have you noticed any traces of blood in your stool?
- Are there colon cancer in your family?
- Is someone in your family suffering or suffering from other cancers, such as breast, ovarian or cervical cancer?
- Did you accidentally lose weight?
- Do you smoke and drink alcohol? How often do you eat meat?
- Is a diabetes known to you?
Physical examination
Next, the doctor will physically examine you. Among other things, he will listen to your stomach with the stethoscope and palpate with your hands. In colorectal cancer, palpation can sometimes be painful.
A particularly important investigation in case of suspected colorectal cancer is the so-called digital-rectal examination (DRU). The doctor scans the rectum with his finger. Not infrequently, colon cancer develops in this section.
Hemoccult test
The doctor often offers the patient a stool sample for the so-called hemoccult test (guaiac test). This test is used to examine if there is blood in the stool that is not visible to the naked eye (occult blood).
The stool sample is applied to the test paper and drizzled with a test solution. In the presence of certain blood components, the test field discolored. One positive test result states that blood may be in the stool, but not necessarily. If the patient has eaten a lot of meat, the test falsely indicates blood in the stool (false-positive result).
If there is actually blood in the stool, the hemoccult test does not say anything about where the blood came from. For example, it can also be positive for nosebleeds, bleeding gums or haemorrhoid bleeding.
On the other hand, the test can give false all-clear (false negative result). For example, if the patient drinks a lot of vitamin C (ascorbic acid), it may interfere with the test: the result may be negative, although there are actually blood stains in the stool.
The Hämoccult test is controversial due to these problems among doctors. He can provide a rough orientation at most. Therefore, an additional colonoscopy is performed almost always in cases of suspected colon cancer.
Colonoscopy (colonoscopy)
she is the one most meaningful examination in suspected colorectal cancer, The intestine is examined with a tubular instrument (endoscope) equipped with a small camera and a light source. The inside of the intestine can thus be illuminated and viewed via a monitor.
As part of the colonoscopy, the doctor can also remove intestinal polyps with a sling. In addition, it is possible to take tissue samples (biopsies) of suspicious areas of the intestinal mucosa. The tissue samples are examined histologically in the laboratory. This is how colon cancer can be reliably detected or excluded.
To prepare for the exam, the doctor gives the patient a laxative. Only when the intestine is emptied, he can be examined well at the colonoscopy.
Alternatives to colonoscopy
If a normal colonoscopy is not feasible for any reason, the doctor may opt for a virtual colonoscopy or a rectoscopy / sigmoidoscopy.
In the virtual colonoscopy a computed tomography (CT) is made. From their images, a computer can calculate and graphically display a three-dimensional image of the gut. In order for the intestinal wall to be reliably assessed, the patient must first empty his bowel thoroughly with laxatives (as in a normal colonoscopy).
A disadvantage of the virtual colonoscopy is that it does not provide as precise a result as the normal colonoscopy. In addition, no polyps or tissue samples can be removed during the examination. So, after that, a proper colonoscopy or surgical intervention may be necessary.
The rectoscopy is the reflection of the rectum with an endoscope. In the sigmoidoscopy In addition to the rectum, the intestine section (S-shaped small intestine loop) in front of it is also examined by means of an endoscope. In contrast to the normal colonoscopy, not the entire colon is examined here. The examination result is thus limited.
Further investigations in colorectal cancer
If the diagnosis of colon cancer is confirmed, further investigations must show how far the cancer has progressed (colorectal cancer stages: see below):
- Rectal ultrasound examination (ultrasonography): This can be used to determine how far the tumor has already spread in the intestinal wall.
- Ultrasound examination (sonography) of the abdomen: The ultrasound is used to search for daughter metastases, especially in the liver. Other abdominal organs (spleen, kidneys, pancreas) are also examined.
- Computed Tomography (CT): Again, one looks for colon cancer metastases, for example in the lungs or liver. Also helpful is the so-called CT angiography: Using contrast media and CT, the blood vessels can be displayed and assessed very accurately.
- Magnetic Resonance Imaging (MRI): Like CT, MRI allows a very accurate representation of various tissues and organs. Metastases can be identified here as well as the exact location and spread of the tumor (important for the operation). The advantage of MRI is that, in contrast to CT, it does not work with X-rays.
- X-ray of the ribcage: An x-ray thorax helps detect daughter metastases in the lungs.
In addition, the doctor regularly measures so-called colorectal cancer patients Tumor marker in the blood, Tumor markers are substances that are increasingly formed by tumors and released into the blood. Thus, in colon cancer, especially the “carcinoembryonic antigen” (CEA) in the blood may be increased. However, it is not suitable for the early detection of colon cancer (even healthy intestinal cells produce CEA). Instead, the CEA level helps to assess disease progression and treatment success:
After the surgical removal of the tumor, the CEA values decrease to the normal range. If there is a relapse (relapse), the value increases again. By regularly determining the CEA value, a relapse can be recognized early.
If there is a suspicion of hereditary colorectal cancer (HNPCC, FAP and other rare forms), a genetic counseling and examination, The genetic material of the patient is examined for characteristic genetic changes (mutations). If the genetic test actually diagnoses hereditary colorectal cancer, the doctor may also offer genetic counseling and genetic testing to close relatives (parents, siblings, children). This will determine if they also have a genetically increased risk of colorectal cancer. If so, regular check-ups with colonoscopy are useful.
Colorectal cancer stages
For the staging of colon cancer, two systems are common: There is initially the so-called TNM classification. It can be applied to almost all tumors and describes the spread of the tumor. Based on the TNM classification, the cancer can then be classified into certain colon cancer stages according to the UICC (Union international contre le cancer).
TNM classification
TNM is an abbreviation for the following three terms:
- T for tumor: This parameter indicates the tumor spread. It is based on the so-called infiltration depth (ie how deep the tumor has penetrated into the tissue).
- N for nodes (lymph nodes): This parameter specifies whether and how many lymph nodes are affected by the cancer cells.
- M for metastases (secondary tumors): This factor indicates whether and how many metastases are present in more distant body regions.
For each of these three categories a numerical value is given. The more advanced the disease, the larger the numerical value. The TNM classification for colorectal cancer is:
|
Tis |
Carcinoma in situ |
Carcinoma in situ (CIS) is an early form of colon cancer. The colon cancer is still in the uppermost tissue layer (epithelium). |
|
T1 |
Infestation of the submucosa |
The tumor has spread to the thin connective tissue layer (submucosa) below the intestinal mucosa. |
|
T2 |
Infestation of the muscularis propria |
The tumor extends even further into the muscle layer below the submucosa. |
|
T3 |
Infestation of subserosa and pericolic or perirectal adipose tissue |
The tumor has invaded all wall layers of the intestine and extends to the outer connective tissue layer (subserosa) or to the adjacent fatty tissue. |
|
T4 |
Infiltration of the peritoneum (T4a) or other organs / structures (T4b) |
The tumor has also affected the peritoneum or other organs. |
|
N0 |
No lymph node involvement |
|
|
N1 |
1-3 regional lymph nodes |
Regional lymph nodes are the lymph node station near the tumor |
|
N2a |
4-6 regional lymph nodes |
|
|
N2b |
≥7 regional lymph nodes |
|
|
M0 |
No distant metastases |
|
|
M1a |
Distant metastases: Only one organ affected |
A so-called peritoneal carcinomatosis is a widespread infestation of the peritoneum with cancer cells. |
|
M1b |
Distant metastases: More than one organ affected or peritoneal carcinomatosis |
Colon cancer stages according to UICC
The UICC colon cancer stages (Union international contre le cancer) are based on the TNM classification. Depending on the extent of tumor involvement, colon cancer is assigned to a specific UICC stage in each patient. Then the treatment is directed. In addition, the prognosis of the patient can be roughly estimated on the basis of the UICC stage.
Examples: A patient with an advanced tumor (T4) according to the TNM classification is still in UICC stage II, as long as there are no daughter colonies in lymph nodes or other organs (N0, MO). On the other hand, a patient with a proven distant metastasis (M1) is always in the severest colorectal cancer stage IV.
Here is an overview of all UICC colon cancer stages:
|
UICC stage: |
TNM classification |
|
0 |
Tis |
|
I |
to T2 if N0 and M0 |
|
II |
T3 to T4, when N0 and M0 |
|
III |
every T at N1 or N2 and M0 |
|
IV |
every T and every N, if M1 |
Colon cancer: treatment
If colon cancer is detected in time, that is, before it has formed daughter abductions in the body, it is often curable. The exact treatment of colorectal cancer depends first on which part of the intestine is affected. For example, there are fundamental differences between the treatment of colorectal cancer (colon cancer) and rectal cancer (rectal cancer). This section explains the treatment of colorectal cancer (colon carcinoma). How rectal cancer is treated, you will find in the text rectal cancer.
The exact treatment plan for colorectal cancer depends on a number of factors: It depends on the exact location of the tumor, how tall it is and whether it has already spread to other parts of the body (tumor stage). Also the age and the general condition of the patient influence the therapy planning.
Colon cancer: surgery
The most important method of treatment for colorectal cancer is surgery: The affected part of the intestine is cut out with a safety margin (ie surrounding tissue). The surgeon sews the remaining bowel ends together. So the patient has again a continuous intestine. Only very rarely in colon cancer permanent or temporary an artificial bowel (anus praeter, stoma) must be created.
Along with the infested bowel, the adjacent lymph nodes are also removed. Both – intestinal section and lymph nodes – are closely examined in the laboratory. In the case of the intestinal tissue, it is checked whether the tumor has also been cut out completely and into healthy tissue. In the extracted lymph nodes, it is checked whether cancer cells have already scattered there.
In early disease stages, a colon cancer surgery is usually sufficient as the sole treatment: By completely cutting out the tumor of the colon cancer is curable. In more advanced stages one also tries to remove the tumor as completely as possible. Also, secondary tumors such as liver metastases can often be surgically removed. In individual cases, this depends greatly on the location and number of metastases. In addition, in advanced colon cancer usually more treatments are needed.
Chemotherapy in colorectal cancer
In more advanced colorectal cancer (colon cancer) many patients receive chemotherapy in addition to surgery. In this case, the danger is very high that, despite complete removal of the tumor, relapse (recurrence) occurs: in many cases, they have already distributed individual cancer cells in the body. That’s why chemotherapy is needed:
The patient receives special anticancer drugs, so-called cytostatics. They inhibit the growth of cancer cells or damage them directly, causing them to perish. The cytostatics are administered periodically either as an infusion or in tablet form. The duration of the therapy is about half a year.
Cytostatics work on all fast growing cells. These include not only cancer cells, but also many healthy cells, such as in the mucous membrane of the digestive tract and hair root cells. Possible side effects of chemotherapy include nausea, vomiting, diarrhea and hair loss.
Radiotherapy for colorectal cancer
Radiation therapy plays a role in colorectal cancer, especially if the tumor is located in the rectum (rectal carcinoma). By contrast, it is not standard in colorectal cancer (colon carcinoma). It can only make sense, for example, to specifically combat metastases in the bones or brain.
Targeted drugs
In some cases, a targeted therapy is also initiated in advanced colorectal cancer, where the patient is given drugs that target specific features of the tumor. They are therefore only suitable for patients whose tumor has these characteristics. This can be determined by examining a sample of the tumor in the laboratory.
An example of targeted drugs are so-called EGF receptor antibody (like cetuximab or panitumumab): In nine out of ten cases of colon cancer, there are docking sites (receptors) for the epidermal growth factor (EGF) on the surface of the tumor cells. It promotes the growth of cancer cells.
This can be prevented with EGF receptor antibodies: The drugs occupy the docking sites of EGF. The growth factor can then no longer dock – tumor growth is slowed down.
Other targeted drugs that may be considered in certain cases of colon cancer are VEGF antibody (like bevacizumab): The abbreviation VEGF stands for “vascular endothelial growth factor”. This substance ensures that new blood vessels form (angiogenesis), which supply the tumor with nutrients and oxygen.
VEGF antibodies are so-called Angiogenesehemmer: They inhibit the growth factor VEGF and thus the formation of tumor-supplying blood vessels. The cancer does not get enough blood to spread further.
Colorectal cancer: disease course and prognosis
The course of the disease and the prognosis of colorectal cancer depend crucially on the stage of disease in which the tumor is detected and treated. The quality of surgical care also plays a key role. The treatment is followed by careful follow-up. It serves to detect a possible relapse (recurrence) as early as possible.
Colon cancer: follow-up visits
Der behandelnde Arzt wird für jeden Darmkrebs-Patienten einen individuellen Nachsorgeplan erstellen: Über einen Zeitraum von fünf Jahren soll der Patient in bestimmten Abständen zu Nachsorgeuntersuchungen erscheinen. Diese Untersuchungen umfassen zum Beispiel ein Arzt-Patienten-Gespräch, eine körperliche Untersuchung, die Bestimmung des Tumormarkers CEA im Blut, eine Darmspiegelung (Kolposkopie), Ultraschalluntersuchungen des Bauchraums sowie eine Computertomografie des Bauchraums und Brustkorbs. Wann welche Untersuchung ansteht, erfährt der Patient von seinem Arzt.
Darmkrebs: Heilungschancen
Ob Darmkrebs heilbar ist, hängt entscheidend vom Stadium der Erkrankung ab. Wenn der Tumor frühzeitig entdeckt und behandelt wird, ist er gut heilbar. Darmkrebs-Heilungschancen sinken aber zunehmend, je weiter fortgeschritten der Tumor ist. Dabei ist bei einem flächigen Befall des Bauchfells (Peritonealkarzinose) die mittlere Überlebenszeit der Patienten noch niedriger als bei anderen Metastasen (zum Beispiel in der Leber).
Darmkrebs: Lebenserwartung
Die Darmkrebs-Lebenserwartung hat sich in den letzten Jahren erhöht. Das liegt zum einen am Vorsorgeprogramm, das eingeführt wurde: Ab einem bestimmten Alter sind regelmäßige Darmkrebs-Vorsorgeuntersuchungen vorgesehen. So lässt sich Darmkrebs oft schon in frühen Stadien entdecken. Zum anderen tragen auch verbesserte Therapiemöglichkeiten zu einer gesteigerten Lebenserwartung bei Darmkrebs-Patienten bei.
Generell hängt die Darmkrebs-Lebenserwartung vom Erkrankungsstadium ab. Sie wird üblicherweise mit der sogenannten Fünf-Jahres-Überlebensrate angegeben. Darunter versteht man jenen Anteil der Patienten, der fünf Jahre nach der Diagnose noch am Leben ist. Voraussetzung dafür ist natürlich, dass eine Behandlung stattgefunden hat. Für Dickdarmkrebs (Kolonkarzinom) und Mastdarmkrebs (Rektumkarzinom) betragen die Fünf-Jahres-Überlebensraten etwa:
|
UICC-Stadium |
Dickdarmkrebs |
Mastdarmkrebs |
|
UICC-Stadium I |
95 Prozent |
95 Prozent |
|
UICC-Stadium II |
90 Prozent |
85 Prozent |
|
UICC-Stadium III |
65 Prozent |
55 Prozent |
|
UICC-Stadium IV |
5 Prozent |
5 Prozent |
Bitte bedenken Sie, dass es sich dabei um statistische Mittelwerte handelt. Die Prognose im Einzelfall kann zum Teil erheblich von diesen Werten abweichen.
Darmkrebs: Endstadium
Betroffene mit Darmkrebs im höchsten Stadium (Stadium IV) haben mit einer Fünf-Jahres-Überlebensrate von nur etwa fünf Prozent leider eine sehr schlechte Prognose. In dieser Situation ist eine Heilung (kurativer Therapieansatz) in der Regel nicht mehr möglich. Die Patienten erhalten dann eine palliative Behandlung. Sie zielt vor allem darauf ab, die Beschwerden des Patienten zu lindern und so seine Lebensqualität zu verbessern. Manchmal wird auch versucht, die Überlebenszeit zu verlängern, und zwar mittels Chemotherapie: Darmkrebs-Patienten müssen sich aber bewusst sein, dass die Chemotherapie sie nicht heilen wird. Die Lebenserwartung beträgt in diesem Stadium ohne Behandlung etwa 12 Monate und mit Behandlung (Chemotherapie) bis zu 24 Monate.
Darmkrebsvorsorge
Darmkrebs wird oft erst erkannt, wenn er schon weiter fortgeschritten ist. Dann sind die Heilungschancen aber nicht mehr so gut wie in frühen Krebsstadien. Deshalb sind Vorsorgeuntersuchungen sehr wichtig. Das gilt besonders, wenn jemand bekannte Risikofaktoren für ein kolorektales Karzinom aufweist wie Übergewicht oder Darmkrebs-Erkrankungen in der Familie.
Im Rahmen der gesetzlichen Darmkrebsvorsorge zahlen die Krankenkassen für Patienten ab 50 Jahren bestimmte Untersuchungen in bestimmten Zeitabständen. Dazu zählen zum Beispiel eine Untersuchung des Stuhls auf “verstecktes” (okkultes) Blut sowie die Darmspiegelung.
Wann Sie einen gesetzlichen Anspruch auf solche Darmkrebs-Vorsorgeuntersuchungen haben, erfahren Sie im Beitrag Darmkrebsvorsorge.).
Additional information
guidelines:
- Leitlinie “Kolorektales Karzinom” der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (2017)
- Patientenleitlinie “Früherkennung von Darmkrebs” der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (2017)
- Patientenleitlinie “Darmkrebs im frühen Stadium” der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (2017)
- Patientenleitlinie “Darmkrebs im fortgeschrittenen Stadium” der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (2017)
Selbsthilfegruppen:
- Deutsche ILCO e.V. – Bundesweit organisierte Selbsthilfevereinigung von Stomaträgern und von Menschen mit Darmkrebs
- Deutsche Krebshilfe