Syphilis is an infectious disease. It is triggered by a bacterium and transmitted mainly in unprotected sexual intercourse. Typical first symptoms are ulcers of the genital organs and lymph node swelling. In the further course, the bacteria can cause severe organ damage and even lead to death. Read everything important about symptoms, infection, treatment and chances of recovery of syphilis!

Quick Overview
- What is syphilis? A bacterial infectious disease that is transmitted almost exclusively sexually. It is also called lues, lues venera, hard chancre or “French disease” (Maladie française).
- Frequency: The number of cases of syphilis fell sharply since the late 1970s, before starting to increase again in 2001. Most patients are men: in 2012, more than ten out of every 100,000 men contracted syphilis. The women affected less than one in 100,000.
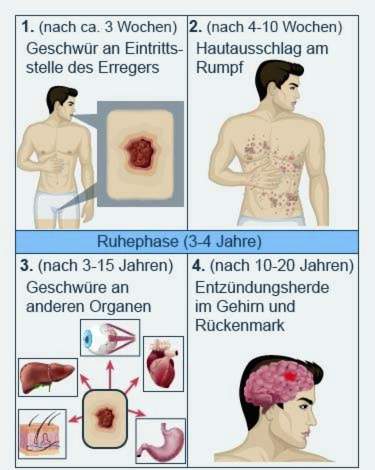
- symptoms: very variable and depending on the stage of the disease; initially painless ulcers at the point of entry of the pathogen and swollen lymph nodes; in stage 2 a variety of skin symptoms; in the third stage infestation of internal organs; Stage 4 Inflammation in the central nervous system (brain and spinal cord).
- Infection: usually by unprotected sex, less often by direct contact with infected blood (such as the joint use of drug cutlery). In addition, infected pregnant women can transmit the pathogen to the child (congenital syphilis).
- Treatment: Antibiotics (preferably penicillin)
- Forecast: Early syphilis stages can usually be cured with antibiotics. Without therapy, the disease sometimes heals on its own. But it can also be chronic and cause serious organ damage or even death.
- Watch out: Even after a healed infection can be infected again with syphilis bacteria!
Syphilis: symptoms
Infection with syphilis (lues, hard chancre) is asymptomatic in about half of all patients. This means that the infected do not develop any complaints. The other half of those infected have syphilis symptoms. These can vary greatly and vary from patient to patient.
Syphilis symptoms in men and women
Basically, syphilis symptoms can affect both women and men alike. Only the point at which the first sign of the infection develops varies: a painless, fluid-secreting nodule. The small ulcer arises at the entry point of the syphilis pathogen. In men, this is usually on the penis (preferably on the glans) and in women very often on the labia.
Another possible gender difference concerns hair loss, which can occur in later stages of the disease. There are indications that it is more common in men than in women.
Apart from that, syphilis generally occurs in both sexes four stages, The first two stages will also early syphilis called, the last two late syphilis, The time interval between the individual stages and their severity can vary considerably from patient to patient. It can also happen that individual syphilis stages are barely noticeable or even completely absent.
Syphilis symptoms in the 1st stage
The first sign of syphilis appears on average three weeks after the infection: at the point of entry of the pathogen forms small, stout ulcer, It is called “ulcus durum” or “primary effect”. As mentioned above, the small nodule in men is usually found on the penis and in women on the labia or in the vagina. At these points, it causes little or no pain.
In people who contract syphilis via oral sex, the ulcer often develops on the lips, in the oral cavity or in the throat. In an infection via anal intercourse, it forms on the anus or in the rectum. These syphilis nodules outside the genital area can be painful.
Initially, the nodule is a small, reddish spot. Within a week or two, it develops into a sharply defined, flat ulcer. It is yellowish and has a rough edge wall. It often secretes a colorless fluid that contains a great many syphilis pathogens. So it is highly infectious.
Over the following weeks swell the lymph nodes in the vicinity of the ulcer. They do not hurt and feel hard.
The ulcer at the entry point of the syphilis pathogen heals spontaneously (by itself) within four to six weeks. Lymph node swelling may persist for months. Without treatment, the first stage of syphilis (primary stage) can progress to the next stage.
Syphilis symptoms in the 2nd stage
About four to ten weeks after the infection, the second stage of syphilis (secondary stage) may occur. This happens when the pathogen spreads through the blood and lymph channels in the body.
Initial syphilis symptoms at this stage are flu-like ailments such as Fever, fatigue, headache, muscle and joint pain, More are developing hard lymph node swelling.
In the further course forms a skin rash (Exanthem), which can be very variable: typically show first slightly reddish, itchy spots, mainly on the trunk. After a few days, stains may develop into tough nodules (papules). They can, like the ulcers, open and get wet. Again, the leaking fluid is again highly contagious.
At the base of the neck, after the skin has healed, the color pigments of the skin disappear (depigmentation). Back remains the pale “Collar of Venus“.
Possible syphilis symptoms in this second stage of the disease are also Mucosal changes in the oral cavity: It can form various plaques (red, furrowed, whitish, etc.). In addition, the Swell almonds.
In the anus region sometimes form flat, lobulated tissue growths.
Many patients start the Hair in places to fail, Physicians call this as Alopecia syphilitica.
Although the second stage of syphilis is favored by the skin and mucous membranes, all organ systems are affected by the disease! This can be expressed, for example, in anemia, liver swelling and headache.
The syphilis symptoms of the second stage (secondary stage) can decay after a few weekswithout leaving any traces (like scars). But you can return several times (Recurrence = recurrence, relapse). The symptoms are less pronounced from time to time, and the skin symptoms are increasingly limited to a smaller area.
Resting phase (latency)
After the second stage of syphilis, the disease can become a longer standstill come. This can last up to ten years (on average, it takes three to four years). There are no symptoms of syphilis during this time. The pathogen is still in the body, however, so there is still a risk of infection. At some point, the syphilis can break out again – now as so-called late syphilis (3rd and 4th stage).
Syphilis symptoms in the third stage
The third or tertiary stage is characterized by symptoms of syphilis, which can affect not only the skin and mucous membranes but also internal organs (such as skeleton, nervous system, eyes, etc.). Everywhere in the body can now be called gums arise. These are slow-growing nodules that can break and form one or more ulcers. The tissue in the ulcer usually dies off (necrosis).
The name “gums” comes from the fact that the tissue nodes contain a thin, stringy (rubbery) and inflammatory secretion.
It is particularly dangerous when the syphilis the Wall of the main artery (aorta) damages, Doctors here speak of “mesaortitis luica”. It can form a Wandaussackung (aneurysm). At this point, the aortic wall is very thin and can easily burst. Then there is danger to life! The aorta carries a lot of blood. If it breaks, you can bleed inside within a short time. This can happen even decades after the infection with syphilis.
Stage 4 syphilis symptoms
If the syphilis is not treated, it may take about ten to twenty years after infection Inflammations in the central nervous system (Brain and spinal cord) develop. Then one speaks of Neurolues or Neurosyphilis. The symptoms of syphilis depend on which part of the brain and / or spinal cord is affected.
So can in an infestation of the Rückenmar Reflections fail and the Motion coordination disturbed be. Also paresthesias (like skin tingling), stinging pain in lower abdomen and legs as well impotence are possible. In addition, many patients may require emptying No longer control the bladder and intestine.
Some syphilis patients develop meningitis with damage to the cranial nerves. That’s what doctors call “syphilitic meningitis”. Possible consequences are for example deafness, dizziness, Paralysis of the eye muscles and blurred vision.
The syphilis pathogens infect the brain, resulting in a chronic progressive encephalitis (encephalitis). It is called Progressive paralysis and can trigger a variety of symptoms. The victims show, for example Changes in her personality, develop Concentration and memory disorders and become gradual accordingly. paralysis are possible as well as epileptic seizures, delusions and depressions, Without treatment, progressive paralysis leads to death within four to five years.
Congenital syphilis: symptoms
Many infants infected with syphilis in the womb die during pregnancy (Miscarriage, stillbirth) or shortly after birth. Others are born prematurely (premature birth).
Infected newborns are at first often inconspicuous, Syphilis symptoms rarely occur right after birth, such as respiratory problems (neonatal respiratory distress syndrome), tissue swelling (edema), enlarged liver and spleen, jaundice, anemia, and skin conditions.
Many of the small patients show signs of syphilis from the 3rd to the 10th week of life. These include:
- Fever and swollen lymph nodes
- variable skin lesions (usually on palms and soles of the feet) and mucous ulcers
- broad-base, wart-shaped skin elevations (condylomata lata), especially in the skin folds (anal and genital region, armpits, etc.)
- Tissue swelling (edema)
- Enlargement of the liver
- Enlargement of the spleen
- jaundice
- paleness
- punctate skin bleeding (petechiae)
- Inflammation of the nasal mucosa (rhinitis, “cold”)
- Intestinal inflammation (enteritis)
- Laryngitis (laryngitis)
- Decreasing drinking on breast or bottle
A Meningitis (Meningitis) as a result of congenital syphilis (syphilis connata or syphilis connata) usually manifests itself between the 3rd and 6th month of life (refusal to drink, cry or whimper, respiratory disorder, etc.). Further signs that syphilis has affected the central nervous system are, for example seizures and “hydrocephalus“(Hydrocephalus).
All of these syphilis symptoms in newborns and infants are termed “Lues connata precoxWithout treatment, the disease passes sooner or later to the next stage of the disease after the second year of life (“Lues connata tarda“):
There are now Syphilis signs on various organs on. Some examples:
- “Saddle nose” as well as changes to the palate, forehead and shins, swelling at the knee joints
- Corneal inflammation of the eyes (with photophobia, eye pain and vision problems to blindness)
- Deafness or deafness
- Malformations of the teeth (“barrel teeth”)
- small cracks in the skin and mucous membranes (rhagades), such as torn corners of the mouth
- Seizures, loss of cranial nerves etc. in case of nervous system involvement
At this stage, syphilis patients are no longer infectious.
Syphilis: Contagion & Causes
The cause of the so-called French disease is the bacterium Treponema pallidum, It will especially with unprotected intercourse from one infected person to another. Also through oral and anal intercourse a syphilis infection is possible. Particularly at risk are people with frequently changing sexual partners.
The Syphilis Bacteria can also by mere Kiss be transmitted. This can happen, for example, if the patient has a small blister / ulcer in the oral cavity and the partner has a tiny injury in the mucous membrane.
Also possible is a syphilis transmission through contaminated blood in a blood transfusion. In Germany, however, all blood products undergo a syphilis test before being given to a patient. In this country threatens this way as no risk of infection.
For drug addicts, there is another possibility of infection: You can get infected with syphilis, if they are infected with the injecting equipment (like needles) and so get in direct contact with infected blood.
There is also a congenital form of syphilis (Syphilis connata or congenital syphilis): Pregnant women who are infected with syphilis can transmit the pathogen to the unborn baby from the 5th month of pregnancy. This risk is especially high in early disease stages. If the woman is infected only during pregnancy, the pathogen almost always passes to the unborn child.
Syphilis and HIV often occur together. This is due to the fact that the skin ulcers in early syphilis stages are easy entry portals for the AIDS pathogen. Both diseases can influence each other negatively in their course.
Syphilis: incubation period
Incubation time is the time interval between the infection with a pathogen and the appearance of the first symptoms. In syphilis, this period can be between ten and 90 days. On average, however, the disease breaks out within two to three weeks.
Duration of infectivity
Stage 1 patients are highly contagious. Slightly lower is the risk of infection in the second syphilis stage. From the third stage of the disease, there is no longer a risk that patients will infect other people with the syphilis pathogen.
Syphilis: treatment
Syphilis therapy can often be done on an outpatient basis. Sometimes, however, inpatient treatment in the hospital is necessary. This is especially true in Neurolues (neurosyphilis) and congenital syphilis.
Syphilis is usually associated with penicillin (Benzathine benzylpenicillin). The pathogen is very sensitive to this antibiotic and has not yet become resistant (insensitive). The duration and dosage of the antibiotic treatment depend on the stage of the disease:
At a early syphilis (first and second stage of the disease), the doctor usually injects the patient Single dose of penicillin, Those who can not tolerate the active ingredient will receive another antibiotic. Often then, for example Tablets with doxycycline or erythromycin prescribed. They must be taken daily for two weeks. Alternatively, in these early stages of syphilis, the antibiotic Ceftriaxone as a short infusion administered once a day for more than 10 days.
A late syphilis (except neurosyphilis) is also preferably treated with penicillin. But then you are three penicillin injections each at intervals of several days needed. Again, in case of intolerance to one another antibiotic are avoided (doxycycline, erythromycin, ceftriaxone). The duration of treatment is then longer than for premature syphilis (e.g., doxycycline tablets over 28 days).
At a neurosyphilis even higher doses of antibiotics and hospital treatment are needed. Mostly, the patient is daily for two weeks high-dose penicillin directly into a vein administered. For penicillin intolerance, ceftriaxone (as an infusion) or doxycycline (in tablet form) may be given.
In addition, individual symptoms of neurosyphilis are specifically treated. For example, the doctor may relieve epileptic seizures with antispasmodic drugs.
Although some patients can prove that the syphilis pathogen has affected the central nervous system, but there are no symptoms. However, this asymptomatic neurosyphilis is treated as well as one that causes discomfort.
Side effect of the therapy
From the second stage of syphilis patients receive once before the first antibiotic dose cortisone, From this stage of the disease, the number of syphilis pathogens in the body is so high that the antibiotic therapy, the so-called Jarisch-Herxheimer reaction can trigger:
Due to the antibiotic treatment, large amounts of syphilis bacteria disintegrate in a short time. The body can react very violently to the released bacteria toxins (toxins). Within two to eight hours after receiving the antibiotics, those affected get fever, chills and headaches. In addition, new skin rashes can occur and existing rashes worsen.
This Jarisch-Herxheimer reaction occurs only at the first penicillin administration. It can be prevented if a cortisone is given half an hour or even before the antibiotic.
Regular check-ups
The success of syphilis treatment is monitored in several follow-up visits. At certain intervals (every few months), the attending physician will examine the patient’s blood for the type and amount of antibodies to the syphilis pathogen. In neurosyphilis also the cerebrospinal fluid (CSF) must be examined. How often and at what intervals check-ups in individual cases are advisable, patients learn from their doctor.
Co-treat partners
Syphilis patients can infect other people until the third stage of the disease, especially during intercourse. Therefore, in the first syphilis stage, all sexual partners of the previous three months should be advised, examined and, if necessary, treated with antibiotics by a physician. For stage 2 or early-stage (latency) syphilis, the same is recommended for all sex partners over the past two years.
Syphilis therapy in pregnant women
In all stages of the disease, syphilis should be used in pregnancy penicillin be treated.
If the woman has a penicillin allergy, doctors recommend one specific immunotherapy (Hyposensitization): The patient is given gradually increasing amounts of penicillin (starting with a very small dose). So her hypersensitive immune system is slowly getting used to it.
Many other antibiotics for syphilis treatment are unsuitable during pregnancy. Some may endanger the unborn baby (like doxycycline), others may damage the liver and cause gestosis (“pregnancy poisoning”) (erythromycin-estolate). In exceptional cases, syphilis in pregnancy can be treated with the antibiotic ceftriaxone.
Therapy of congenital syphilis
Newborns born with syphilis receive for two weeks penicillin directly into a vein. If the baby is also infected with HIV, the antibiotic may be given longer.
Syphilis: examinations and diagnosis
If syphilis is suspected, the doctor first collects the medical history of the patient (anamnesis). Among other things, he gives a detailed account of the symptoms that occur, asks how long they have already existed and whether there are any pre- or underlying diseases (such as HIV infection). In addition, the doctor inquires about the sexual life of the patient. As uncomfortable as such questions are for some people affected – the doctor needs the information to be able to make the right diagnosis as quickly as possible.
In the next step, the doctor tries to prove the syphilis pathogen directly or indirectly:
In the early stages, the bacteria in large numbers in the liquidSecretion of skin ulcers discover. A special microscopy technique is used (dark field microscopy).
Specific antibodies in the blood can be detected after the pathogen has entered the bloodstream. For this Screening test Various test methods are used, for example the Treponema pallidum hemagglutination test (TPHA). He shows a positive result two to three weeks after the infection, which usually lasts a lifetime. Then the patient is very likely to have syphilis.
Syphilis rapid tests are also suitable as a screening test for specific antibodies against the pathogen.
The result of screening tests is not one hundred percent sure. Even if it turns out to be positive, that’s why Confirmatory test with another method (such as a fluorescence Treponema antibody absorption test, FTA-ABS test).
If the diagnosis of “syphilis” is established, the doctor must still find out whether it is an old infection or an active infection requiring treatment. This is the suitable VDRL test (Venereal Disease Research Laboratory-test). It detects antibodies that form the immune system in syphilis, but also in other diseases (such as malaria, HIV). A positive test result is thus generally an indication of tissue destruction and inflammatory processes. If confirmed syphilis, the test can say something about the disease activity.
A syphilis infection can become active again after a long symptom-free resting phase (latency phase) and cause discomfort (reactivation). On the other hand, you can re-infect with syphilis after a successfully healed infection (reinfection). From the results of the antibody determination can not be read whether it is a reactivation or reinfection.
If a neurosyphilis is suspected, the doctor will also become one Sample of cerebrospinal fluid remove (CSF). It is tested in the laboratory for specific antibodies against Lues bacteria.
Often the doctor still leads further investigations by. Among other things, they serve to rule out comorbidities. For example, some syphilis patients still suffer from other sexually transmitted diseases, such as HIV, hepatitis B or chlamydia.
Syphilis is notifiable
Doctors must report any evidence of the syphilis pathogen to the responsible health department. This applies both to the direct detection (smear of skin ulcers) and the indirect detection (specific antibodies against syphilis bacteria). The name of the patient is not given to the health department.
Syphilis: disease course and prognosis
Antibiotics are very effective in syphilis: thanks to these drugs, the first two stages of the disease are almost 100 percent curable. Even in the third stage, the penicillin therapy can heal the infection in most cases. However, existing organ damage can generally not be reversed.
Without treatment, syphilis heals spontaneously in about every third patient (early stages). In the others, the disease progresses and becomes chronic. In advanced stages organs are permanently damaged. About every 10th patient dies of untreated syphilis.
In HIV patients, syphilis is often atypical and more severe than in HIV-negative patients. In addition, they develop more often neurosyphilis.
Syphilis: prevention
You can especially prevent syphilis Safe sex: Always use condoms during sexual intercourse. In oral sex, it is recommended to use a scarf to protect against syphilis and other sexually transmitted diseases.
Such protective measures are especially important if someone changes the sexual partner more often. You can significantly reduce the risk of syphilis, but not completely eliminate it. Namely, the syphilis pathogen can also be transmitted by kissing or simply touching, for example, when the infected person has mouth ulcers and the partner has tiny skin or mucosal injuries.
Attention should also be paid to items and materials used with the Blood or infectious rash from syphilis patients in early stages. These would be for example syringes, towels and bandages. They should not be reused. In normal social contacts but no special precautions (disinfection, etc.) are necessary – Syphilis patients must not be avoided!
As part of the prenatal care Among other things, the blood of the expectant mother is examined for syphilis. If the test is positive, the pregnant woman should be promptly treated with penicillin. The antibiotic also reaches the child through the placenta. It is therefore treated. This can prevent or at least curb a childish infection.
Also the blood of blood donors becomes one syphilisTest to avoid transmission by blood transfusions.
Additional information
guidelines:
- Guideline “Diagnosis and Treatment of Syphilis” of the German STI Society e. V. (2014)