Skin cancer is a generic term for various malignant (malignant) diseases of the skin. The most common is “white skin cancer”. Second is the far more dangerous black skin cancer. Symptoms and therapy of skin cancer depend on the form. In general, however, it is important for a successful treatment to detect skin cancer at an early stage. Read more about the topic: What does skin cancer look like? What are the causes? How is he diagnosed and treated? How good is skin cancer curable?

Quick Overview
- What is skin cancer? Collective term for various malignant (malignant) skin diseases. Every year more than 293,000 people in Germany become ill with skin cancer. The most common is “white skin cancer” followed by “black skin cancer”.
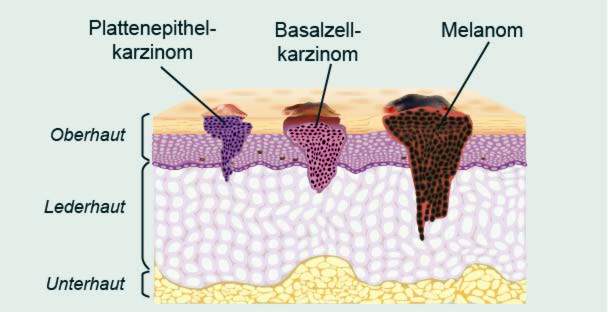
- Forms of skin cancer: White skin cancer (basal cell carcinoma and squamous cell carcinoma), black skin cancer (malignant melanoma), rare forms of skin cancer (such as Merkel cell carcinoma, Kaposi’s sarcoma, Dermatofibrosarcoma protuberans)
- symptoms: very different depending on skin cancer form and subtypes. For example, black skin cancer often manifests itself as a dark, irregular-shaped pimple that may be either flat or nodular. Basal cell cancer often begins as a waxy nodule that sinks in the middle and alternately heals and bleeds again. But there are also dark, yellowish or ulcerated basaliomas.
- Causes & Risk Factors: In white and black skin cancer especially UV light (sun, solarium, etc.); other risk factors depending on skin cancer form for example, genetic predisposition, hereditary diseases and chemicals. For rare forms of skin cancer (Kaposi’s sarcoma etc.), among other viral infections.
- Treatment: depends on the skin cancer form and the tumor stage. Standard method is an operation. Alternatively or additionally, other therapies can be used, such as radiotherapy (radiation), chemotherapy, photodynamic therapy or immunotherapy.
- Forecast: If skin cancer (of any kind) is detected and treated early, the chances of recovery are generally high. The more advanced a tumor already is, the worse the prognosis. This is especially true for black skin cancer.
Skin cancer: symptoms
The chances of a cure for skin cancer are the better, the earlier the tumor is discovered and treated. But how do you recognize skin cancer? The answer depends on the exact form of skin cancer. In general, the signs of dangerous malignant melanoma (black skin cancer) are easier to recognize than, for example, “white skin cancer”. Malignant melanoma develops from pigment-forming skin cells (melanocytes) and therefore causes dark-colored skin changes. However, the manifestations of black skin cancer are sometimes very different. In “white skin cancer” (basal cell carcinoma and squamous cell carcinoma) the lesions are usually lighter.
For all forms of skin cancer: The skin cancer symptoms are limited to the skin at an early stage. As soon as the cancer cells spread in the body, further complaints can develop.
Black skin cancer: symptoms
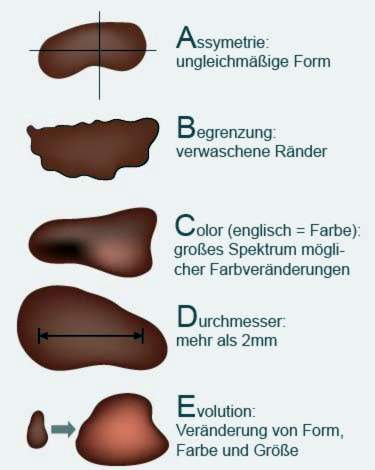
Black skin cancer (malignant melanoma) can look like a simple pigment (liver spot, birthmark). Based on the so-called ABCD rule, it can be estimated whether a dark mark is actually a harmless pigment or possibly a skin cancer. Read more in the section “Skin cancer screening”.
In essence, there are the following Manifestations of malignant melanomas:
Superficial Spreading Melanoma (SSM): Superficial spreading melanoma is the most common form of black skin cancer. Symptoms: Flat, sometimes nodular skin lesions, often sharply demarcated by healthy skin. The color can vary from brown, gray, pink to blue-black. Rarely, some areas appear whitish. The SSM develops within one to four years preferably on the back, chest and extremities.
Nodular melanoma (NM): Nodular (nodular) melanoma is the most aggressive form of black skin cancer. Symptoms: Like SSM, nodular melanoma often develops on the back, chest and extremities. It quickly (within a few months) develops a raised, nodular and often bleeding tumor of blue to dark brown color. He is growing very deep. Therefore, this form of black skin cancer has the worst prognosis of all melanomas.
Lentigo maligna melanoma (LMM): Lentigo maligna melanoma develops slowly over years or decades on the basis of the precancerous lesion Lentigo maligna. Especially the elderly get sick with this form of black skin cancer. Preferred locations include sun-exposed areas such as the face, neck, arms, and hands.
Acrolentiginous melanoma (ALM): Of the four types of melanoma mentioned here, ALM is the rarest form of black skin cancer. Symptoms: The acrolentiginous melanoma often forms blurred, multi-colored spots on the extremities (akrene), ie in the area of the palms, soles of the feet, fingers and toes, especially under the nails. It can be mistaken for a nail injury, a nail fungus or a wart.
Besides these main forms, there are even rarer ones special shapes of black skin cancer such as amelanotic melanoma (AMM) or choroidal melanoma.
Spiny cell cancer: symptoms
The appearance of squamous cell carcinoma (squamous cell carcinoma, spinalioma) often resembles that of actinic keratosis in the initial stage. It often starts with one reddish-yellowish cornification (Hyperkeratosis), usually not without one small bleeding can be replaced. On the edge, the skin is often slightly red due to inflammation.
Advanced forms of acicular cancer discolor due to increasing cornification whitish, become thick and spread out. Later skin cancer symptoms are warty-humped skin growths, which are firmly fused with the ground. They feel rough like coarse sandpaper. If one tries to relieve these cornifications, the skin starts to bleed.
Spinaliomas are often found on the ear edge or on the face (also on the lips). They can arise on healthy skin as well as in scars or chronic wounds.
Basal cell cancer: symptoms
Most form basal cell carcinomas (basaliomas) in the so-called centrofacial area, ie in the face between the hairline and upper lip, Often you can find them at one, too auricle, on the hairy scalp and in lower third of the face, Somewhat less common are basal cell carcinomas of the trunk, arms or legs. Basal cell carcinomas do not appear on the oral and genital mucosa, the palms and soles of the feet.
This form of white skin cancer is very diverse in its appearance. The beginning is usually only a few millimeters large, shiny translucent or waxy Nodules (papules), In part, even the first telangiectasia can be seen on the surface. These are the finest blood vessels visible to the naked eye. Shaving or scratching often causes a light, bloody crust on the papules. Over the course of months and years, the surface of the papules sinks in the middle – it creates one Trough with a small pearl-like rim, This indicates that the tumor is growing. On the rim you can see tiny blood vessels. Typically, this wound has not healed after weeks: Alternately, she heals and bleeds.
This nodular (nodular) basal cell carcinoma is the most common variant of basal cell cancer. Other manifestations include:
- Superficial basalioma: This type of basalioma is often overlooked because it resembles inflammatory skin conditions such as psoriasis. Most commonly it occurs on the trunk, arms and legs.
- Pigmented basalioma: This type of basal cell carcinoma is heavily pigmented and therefore darkened. It can therefore be mistaken for black skin cancer (malignant melanoma).
- Scleroderma Basalioma: Basal cell carcinoma looks like a yellowish deposit and is often difficult to differentiate from healthy skin. Sometimes this shape is reminiscent of scar tissue. Nodules are hardly recognizable.
- Exulcerating basal cell growth: In the face, there is often an ulcerous decay of the basalioma. If deeper tissue layers are destroyed, doctors speak of the destructively growing basalioma.
Recognize skin cancer: tips
The skin is constantly changing. There are always spots and other changes. Only very rarely is it actually skin cancer. Signs of a malignant skin tumor can also easily be confused with harmless changes. Therefore, have your family doctor or a dermatologist explain which symptoms typically cause skin cancer and how to recognize it. The doctor will also tell you after a review of your skin may on moles that you should keep in mind because they may develop from skin cancer. You can also view pictures of skin cancer cases in books and the internet. This helps you to better assess changes in your skin.
Skin cancer: cancers
Roughly speaking, there are three groups of skin cancers: white skin cancer, black skin cancer, and some rare forms of skin cancer (such as Kaposi’s sarcoma, Merkel’s carcinoma, and Dermatofibrosarcoma protuberans).
The white skin cancer
The term “white skin cancer” (or “light skin cancer”) summarizes various forms of skin cancer: basal cell carcinoma (basal cell carcinoma, basalioma) and squamous cell carcinoma (squamous cell carcinoma, spinal or squamous cell carcinoma). An early form of spiny cell cancer is actinic keratosis.
White skin cancer is by far the most common form of malignant skin cancer. It is less dangerous than black skin cancer because, unlike it, it has no or hardly any daughter metastases in other parts of the body. The white skin cancer can therefore usually completely remove and is rarely fatal.
More about white skin cancer and its main agent – basal cell carcinoma – read in the article White Skin Cancer.
Spiny cell or squamous cell carcinoma
Prickly cell carcinoma (spinal or carcinoma of the squamous epithelium) is the disease of people over the age of 60 years. Affected are usually body parts that are often exposed to the sun. These are, for example, face, ears, backs of the hands and forearms.
Squamous cell carcinoma grows more aggressively than basal cell carcinoma: the malignant tumor gradually destroys the surrounding tissue. If not detected and treated early enough, it can cause metastases in other parts of the body. This complicates the treatment and worsens the prognosis. Out of 1,000 patients, around 40 to 50 die from this type of skin cancer (for comparison: basal cell cancer ends fatally in only about one in 1,000 patients).
Read all about the causes, symptoms, treatment and prognosis of the spinal myoma in the Beirag squamous cell carcinoma.
Actinic keratosis
Actinic keratosis – as well as Bowen’s disease (Bowen’s disease) – is a possible precursor of squamous cell carcinoma. It is accompanied by sharply limited redness, which feels like sandpaper when touched. These skin areas can later also verhornen. Sometimes they remain inconspicuous for years or even for life. It may also develop into a squamous cell carcinoma.
Whether that happens or not can not be predicted. For safety’s sake, therefore, actinic keratosis should always be treated. For example, one can surgically remove the lesions, “freeze” them with liquid nitrogen, remove them with laser or corrosive solutions or treat them with a special cream / ointment.
Learn more about this widespread early form of squamous cell carcinoma in the Beirag actinic keratosis.
Black Skincancer
Black skin cancer (malignant melanoma) can develop on all parts of the body – even those that are barely exposed to the sun (such as the genital area, hairy scalp, sole of the foot, under the nails). It is significantly less common than white skin cancer: Altogether, about 328 out of every 100,000 people suffer from skin cancer each year. At around 290 of them, the diagnosis is “white skin cancer.” The remaining approximately 38 patients have malignant melanoma. The mean age of onset of these patients is 64 years (men) and 58 years (women).
Despite the lower prevalence, black skin cancer is much more feared than white skin cancer. It is more aggressive and spreads much faster in the body. The exact course of the disease depends, among other things, on the type of black skin cancer. The different types of melanoma differ in their aggressiveness.
Read all about the causes, symptoms, diagnosis, therapy and prognosis of malignant melanoma in the article Malignant melanoma.
Kaposi’s sarcoma
Kaposi’s sarcoma is a rare form of skin cancer that also mucous membranes and internal organs may affect. It occurs in different variants on. For example, in addition to the classic form of illness, there is the HIV-associated Kaposi’s sarcoma: It develops in people whose immune system is weakened due to HIV infection.
In addition, this type of skin cancer is often seen in patients whose immune system has to be suppressed due to medical reasons (iatrogenic immunosuppression). This is necessary after an organ transplant. The fourth disease variant is the so-called endemic Kaposi’s sarcoma. It occurs in tropical Africa mainly in children and young adults.
The different disease variants differ in their aggressiveness and treatment. Read more about it in the article Kaposi’s sarcoma.
Skin cancer: treatment
How the skin cancer therapy looks in each case depends on several factors. In particular, what type of skin cancer is involved and how advanced the tumor is already play a role. Also the age of the patient and the general state of health are taken into consideration in the therapy planning.
White skin cancer: treatment
For the treatment of the two forms of white skin cancer, basalioma and spinalioma, various procedures are available. The best Erfoglsaussichten has an operation. If this standard therapy is not possible or not sufficient, alternative or additional methods of skin cancer treatment can be considered (radiotherapy, photodynamic therapy, etc.).
surgery
During surgery, the surgeon removes the cancer tumor as completely as possible – along with a seam of apparently healthy tissue all around. So the chance is higher, that you really “catch” all cancer cells. To check this, the removed piece of skin is examined histologically under the microscope. If, despite everything, suspicious cell changes are found in the supposedly healthy border area, surgery must be performed again and further skin tissue must be excised. This is repeated until the tissue removed under the microscope really turns out to be healthy.
This approach to surgical skin cancer treatment will microscopic-controlled surgery or micrographic surgery called. Its purpose is to make sure that you have actually “caught” all the cancer cells around the tumor site.
With a very deep basal or spinal irregularity, so much tissue must be removed that the result often leads to cosmetic problems. Then, after completion of the skin cancer treatment, some skin from another body region can be transplanted to this site (skin grafting).
For very superficial basaliomas or spinal analomas, it is often sufficient to scratch out the cancerous cells to some extent (curettage). This means that the doctor scrapes the diseased tissue with a special medical instrument.
In certain cases, as skin cancer therapy is also a so-called Cold surgery (cryotherapy) possible. The changed skin areas are briefly treated with liquid nitrogen (“iced”). Inside the cells ice crystals form, which destroy the cells. The method is used for example in spiny cell cancer and its precursor (actinic keratosis).
radiotherapy
Skin cancer irradiation by radiation (radiotherapy) is mainly used when the tumor is very large or unfavorable located (near the eyes). Even in elderly patients, for whom an operation would be too stressful, a basalioma or spinalioma can instead be irradiated.
In this case, very high-energy X-rays are usually directed at the tumor in several sessions, which cause the cancer cells to die. The treating physician focuses the rays as precisely as possible on the tumor in order to minimize the risk of surrounding healthy tissue.
Photodynamic Therapy (PDT)
Superficial basal cell carcinoma (basal cell carcinoma) and actinic keratosis can also be treated with photodynamic therapy (PDT). Here, the changed skin areas are first treated with a special drug, which makes the tissue more sensitive to light. Subsequently, the area is irradiated with very long-wave light (no X-rays). It causes the tumor cells to die.
Sunbathing must be avoided in the period of photodynamic therapy!
chemotherapy
Sometimes white skin cancer is also treated with chemotherapy (outpatient or inpatient). Patients receive special drugs that inhibit the division and proliferation of cancer cells (cytostatics).
In the systemic chemotherapy The cytostatics are administered internally (for example as a tablet or infusion) so that they can be effective throughout the body. This form of skin cancer treatment is considered for basal cell cancers when the tumor can not be operated on or multiple tumors are present. In squamous cell carcinoma (spinalioma), it may become necessary if the tumor is inoperable or has already metastasized. Chemotherapy may be combined with radiation in this case.
In the local chemotherapy the cytostatics are used as an ointment directly at the site of the tumor. The effect of this skin cancer treatment is therefore localized (as opposed to systemic chemotherapy). But the risk for side effects is lower. Local chemotherapy can be used for superficial basal cell carcinoma and actinic keratosis.
immunotherapy
Immunotherapy (immunomodulatory therapy) is a newer possibility of skin cancer treatment in certain cases of basalioma or actinic keratosis. In this case, a cream with the active ingredient imiquimod is applied regularly over several weeks on the affected skin. Imiquimod activates the immune system of the skin, which then attacks the tumor cells in a targeted manner. Visible and with the naked eye not yet recognizable tumor areas are eliminated painlessly. Scars are not left behind in this skin cancer therapy. Since long-term results are still outstanding, it can not be ruled out that higher relapse rates occur than with surgical therapy.
Black skin cancer: treatment
Even more than in white skin cancer, the treatment at the tumor stage is based on black skin cancer. Malignant melanoma forms early metastases (metastases). A total of five melanoma stages (some with subgroups) are distinguished. The scale ranges from stage 0 (= superficial, limited tumor without metastases) to stage IV (= tumor, which has already formed metastases in other organs).
surgery
In all stages of black skin cancer, surgery is the treatment of choice. The tumor is removed as completely as possible with a hem of healthy tissue. How deeply cut into healthy tissue depends on the size of the tumor.
If the melanoma is more than a millimeter in diameter, then a tissue sample from the sentinel lymph node taken. This is the lymph node closest to the tumor in the downstream area of the lymph. He is being examined for cancer cells. As soon as individual cancer cells separate from the melanoma and scatter in the body, the sentinel lymph node is usually the first to be affected. If this is indeed the case, it is removed – usually together with adjacent lymph nodes. In addition, further treatments are usually recommended to support the success of the therapy. This can be, for example, an immunotherapy with interferon (interferon therapy), radiation or chemotherapy.
interferon therapy
The active ingredient interferon-alpha can influence the immune system to support the treatment of skin cancer: as an injection it activates certain immune cells (killer cells), which attack and destroy the cancer cells. Interferon treatment is often used when the malignant melanoma has exceeded a certain size or has already formed metastases: After surgical removal of all visible growths, interferon therapy can eliminate any micrometastases (invisible colonizations). This should increase the chances of recovery.
Radiation and chemotherapy
In more advanced black skin cancer, radiotherapy may be followed by surgery. Affected lymph nodes as well as daughter colonies in distant organs (distant metastases) can be treated like this. Irradiation can also be useful if the malignant tumor can not be completely removed during the operation.
However, radiation can also be used as a surrogate for surgery: For example, if the patient is too old for surgery or the tumor is not operable, it is often irradiated instead.
Occasionally, the operative skin cancer treatment is supported with chemotherapy: The administered anticancer drugs (cytostatics) to eliminate distant metastases.
Targeted therapy (“targeted therapy”)
A new possibility of skin cancer therapy in advanced malignant melanoma is the administration of drugs that specifically target cancer cells: The active ingredients contained (such as dabrafenib) can inhibit the proliferation of cancer cells and thus reduce the tumor. But this only works if the cancer cells show a certain genetic change. So this has to be clarified beforehand.
Targeted therapies have one great advantage: Traditional treatments such as chemotherapy or radiotherapy can not differentiate between healthy cells and cancer cells. So it also damaged healthy cells, causing corresponding side effects (hair loss, etc.). In contrast, targeted therapies are directed only against selected targets of cancer cells. Healthy cells are thus spared.
Rare forms of skin cancer: treatment
For the Kaposi’s sarcoma There is no standard therapy scheme that is widely recognized. In therapy planning, individual factors as well as the disease variant are taken into account. For example, classical Kaposi’s sarcoma usually requires radiation therapy to eliminate the tumor. In some cases, chemotherapy is also used, for example when the tumor is very large. There is also the possibility of immunotherapy with interferons.
In HIV-associated Kaposi’s sarcoma, the use of HIV drugs (as a combined antiretroviral therapy, cART) plays an important role: in patients who have not been treated with a cART in the onset of skin cancer, the tumor often ceases its growth, as soon as the HIV medication is started. Sometimes the Kaposi syndrome even disappears completely. If skin cancer first develops during HIV treatment, it must be checked for its efficacy. In advanced skin cancer satellites, antiretroviral treatment is combined with chemotherapy.
A Kaposi’s sarcoma, which develops in drug-suppressed immune system, often formed by itself, as soon as the drugs (immunosuppressants) are discontinued. If this is not possible, it may be sufficient to reduce the dose of the drugs. In addition, the tumor can be irradiated.
The Merkel cell carcinoma is usually removed surgically. Subsequently, the tumor area and the adjacent lymph nodes should be irradiated. Chemotherapy can also be effective in this form of skin cancer.
Also at Dermatofibrosarcoma protuberans (DFSP) If possible surgery is performed: The tumor is cut out together with a safety margin (ie together with a hem of demonstrably healthy tissue). If surgery is not possible, the skin cancer treatment is often done by radiation. A newer option for DFSP treatment is targeted therapy with imatinib. This drug inhibits tumor growth. However, it is only used in certain cases, for example if the tumor is not operable or already well advanced, or returns after a successful initial treatment.
Skin cancer: causes and risk factors
The most important cause of skin cancer is UV light. In addition, we now know more risk factors. However, the exact mechanism of carcinogenesis is still not clear.
White skin cancer: causes
Is the skin repeated ultraviolet rays (UV light) exposed to increased risk of white skin cancer. This does not apply to both the UV rays in sunlight and in the solarium. Skin cancer is a possible long-term consequence in both cases. In addition to the solarium, other artificial UV sources pose a skin cancer risk. These include UV devices for phototherapy (such as eczema or psoriasis) or for curing of plastic (nail salon, dentist).
UV light refers to electromagnetic radiation with a wavelength of 100 to 400 nanometers (nm). In fact, there are three different types of UV rays:
- UV-A: Wavelength between 315 and 400 nm; In the solarium, it tans the skin and makes the skin age prematurely.
- UV-B: Wavelength between 280 and 315 nm; ensures the sun tans the skin.
- UV-C: Wavelength between 100 and 280 nm; is almost completely filtered out of the sunlight by the ozone layer.
The tan results from the skin’s increased production of the brown dye (pigment) melanin – as protection against the high-energy UV rays. If the radiation is too strong, it causes burns such as redness and pain (sunburn).
But even without these visible consequences UV radiation damages the skin, more precisely the genome of the skin cells. If the cells fail to repair this damage, they can degenerate and become cancer cells become. This can happen only years or decades after repeated or intense sun exposure – the skin forgets no UV damage and no sunburn!
Skin cancer: Particularly bright skin types at risk
How much sun a person tolerates is very different. The brighter the skin type, the less self-protection the skin has since less melanin (skin pigment) is produced. Europeans distinguish between four types of skin:
- Skin type I: Sunburns develop very quickly. Solar radiation hardly leads to a tanning (“Celtic type”).
- Skin Type II: Sunburns are common, tanning is slow (“light-skinned European type”).
- Skin type III: Sunburns occur only occasionally, the tanning works well (“dark-skinned European type”).
- Skin Type IV: Sunburns are very rare, a good suntan is available even without significant sun exposure (“Mediterranean type”).
Other causes of white skin cancer
Repeated, unprotected UV exposure is the main cause of basal cell carcinoma and squamous cell carcinoma. In addition, other factors can promote the development of white skin cancer:
In some families, basal cell cancer is more common. Apparently there is one genetic predisposition for this skin cancer type. Both basal cell and spiny cell cancers can be affected by exposure to various Fabrics and chemicals as arsenic and by-products of petroleum processing are favored. There are also some hereditary diseasesthat increase the risk of white skin cancer (such as xeroderma pigmentosum).
People with white matter are also more susceptible to white skin cancer weakened immune system, If, for example, after an organ transplant, the immune system has to be suppressed by medication, the risk of skin cancer increases.
Rarely, white skin cancer develops as a result of chronic wounds or scars (such as burn scars).
Black skin cancer: causes
The main cause of black skin cancer is also UV light: Repeated sunburns (especially in childhood) can cause malignant melanoma. There is also a certain hereditary predisposition for this dangerous form of skin cancer. This is supported by the increased occurrence of black skin cancer in some families. The light skin types I and II are significantly more frequently affected by black skin cancer.
In addition, some risk factors for black skin cancer, which also play a role in white skin cancer. These include some hereditary diseases (like Xeroderma pigmentosum) as well as a weakened immune system (about after organ transplantation due to the intake of drugs zru inhibition of the immune system).
An increased risk of disease also carry people with a previous melanoma disease: Such a return of black skin cancer usually occurs in the first five years after the removal of the first tumor.
at aircrew the risk of malignant melanoma is also slightly elevated.
Black skin cancer & birthmark / liver spot
In some cases, a mole or birthmark causes malignant melanoma (black skin cancer). Leberfleck beziehungsweise Muttermal sollte man vor allem dann im Auge behalten, wenn jemand besonders viele davon hat: Wer mehr als 40 oder 50 solcher Pigmentmale besitzt, sollte diese regelmäßig vom Hautarzt begutachten lassen.
Meistens entsteht das Maligne Melanom aber “aus dem Nichts” heraus, also auf normaler Haut ohne Pigmentmale.
Ein Muttermal (Nävus) ist eine gutartige, helle oder dunkle Hautwucherung, die angeboren oder erworben ist. Ein Leberfleck (Pigmentnävus) ist eine braune Hautveränderung, die sich aus pigmentbildenden Hautzellen (Melanozyten) entwickelt. Umgangssprachlich werden Muttermal und Leberfleck aber synonym verwendet (als Begriffe mit gleicher Bedeutung).
Seltene Formen von Hautkrebs: Ursachen
Für die Entstehung des Kaposi-Sarkoms hat die UV-Strahlung keine oder kaum eine Bedeutung. Das Gleiche gilt beim Merkelzellkarzinom und beim Dermatofibrosarcoma protuberans (DFSP). Bei diesen sehr seltenen Formen von Hautkrebs spielen andere Risikofaktoren eine Rolle:
So sind am Auftreten des Kaposi-Sarkoms bestimmte Herpesviren beteiligt (humanes Herpesvirus 8, HHV-8). Eine Infektion mit diesen Viren allein kann aber nicht den Hautkrebs verursachen. Vielmehr müssen weitere Faktoren hinzukommen (etwa genetische Faktoren).
Die genauen Ursachen des Merkelzellkarzinoms sind unklar. Allerdings scheinen auch hier bestimmte Viren an der Krebsentstehung mitzuwirken.
Wie es zu einem Dermatofibrosarcoma protuberans kommen kann, weiß man nicht. Bislang sind keien Risikofaktoren für diesen Hautkrebs-Typ bekannt.
Warum nimmt Hautkrebs zu?
Die Weltgesundheitsorganisation WHO schätzt, dass weltweit pro Jahr zwei bis drei Millionen Menschen neu an weißem Hautkrebs und 250.000 Menschen neu an schwarzem Hautkrebs erkranken. Dabei steigen die Erkrankungszahlen seit Jahrzehnten an. Verantwortlich dafür ist vermutlich ein zu sorgloser Umgang mit UV-Strahlung, etwa beim Sonnenbaden oder in Solarien. Vor allem intensive Sonneneinstrahlung und Sonnenbrände in der Kindheit erhöhen deutlich das Hautkrebs-Risiko.
Hautkrebs: Untersuchungen und Diagnose
Manche Menschen scheuen den Gang zum Arzt. Doch wie bei kaum einer anderen Krebsart ist es bei Hautkrebs entscheidend für die Prognose, wie früh der Tumor entdeckt und behandelt wird. Wenn Sie eine auffällige Hautstelle an sich entdecken, sollten Sie diese deshalb vom Dermatologists abklären lassen. Er kann feststellen, ob es sich tatsächlich um Hautkrebs handelt.
Survey of the medical history
Als erstes wird der Arzt im Gespräch mit Ihnen Ihre Krankengeschichte erheben (Anamnese). Er erkundigt sich nach entdeckten Hautveränderungen, eventuellen Beschwerden sowie möglichen Vorerkrankungen. Häufige Fragen sind etwa:
- What complaints do you have?
- Wann ist Ihnen die verdächtige Hautstelle zum ersten Mal aufgefallen?
- Blutet oder juckt die auffällige Stelle?
- Which medications do you take?
- Gibt oder gab es ähnliche Beschwerden in Ihrer Familie, zum Beispiel bei Eltern, Geschwistern oder Kindern?
- Sind bei Ihnen irgendwelche Hauterkrankungen wie beispielsweise Schuppenflechte bekannt?
- Halten Sie sich privat oder aus beruflichen Gründen viel in der Sonne auf?
- Gehen Sie regelmäßig ins Solarium?
investigations
Im nächsten Schritt untersucht der Hautarzt die auffällige Hautstelle gründlich mit einem Auflichtmikroskop (Dermatoskop). Möglicherweise möchte er sich zudem die restliche Haut ebenfalls ansehen, um diese auf Auffälligkeiten zu überprüfen.
Sollte der Hautarzt einen Verdacht auf Hautkrebs haben, wird er weitergehende Untersuchungen veranlassen. Dazu gehört vor allem die Entnahme einer tissue sample: Unter lokaler Betäubung wird die verdächtige Hautstelle samt Sicherheitsabstand entfernt. Das Gewebe wird im Labor von einem Pathologen feingeweblich (histologisch) genau untersucht. So lässt sich feststellen, ob tatsächlich Hautkrebs vorliegt. In diesem Fall schließen sich weitere Untersuchungen an:
- Imaging procedures wie Röntgen, die Computertomografie (CT), Kernspintomografie (MRT) oder Ultraschall (Sonografie) können zeigen, ob und wie weit sich der Krebs schon im Körper ausgebreitet hat (Metastasenbildung). Dies ist für die Wahl der richtigen Therapie sehr wichtig.
- blood tests sagen etwas über den Allgemeinzustand des Patienten und die Funktion wichtiger Organe im Körper aus. Dies ist unter anderem wichtig, um das Risiko einer Narkose (bei der Operation) abschätzen zu können.
- The Skelettszintigrafie (Knochenszintigrafie) ist eine nuklearmedizinische Untersuchung, mit der sich Knochenmetastasen aufspüren lassen.
Hautkrebs-Screening (Früherkennung)
Die gesetzlichen Krankenkassen bezahlen allen Versicherten ab dem 35. Lebensjahr alle zwei Jahre eine Untersuchung zur Hautkrebs-Früherkennung (Hautkrebs-Screening). Dabei untersucht ein speziell geschulter Arzt die gesamte Hautoberfläche. Ziel der Hautkrebs-Vorsorge ist es, bösartige Veränderungen der Haut frühzeitig aufzudecken. Dann liegen die Heilungschancen nämlich bei fast 100 Prozent.
Die Genehmigung für das Hautkrebs-Screening erhält ein Arzt durch die Teilnahme an einem speziellen Trainingsprogramm. Das Hautkrebs-Screening wird also meist von Allgemeinärzten mit entsprechender Ausbildung oder von Hautärzten (Dermatologen) durchgeführt.
Wie läuft das Hautkrebs-Screening ab?
Das Hautkrebs-Screening ist vollkommen schmerzfrei. Der Arzt begutachtet Ihre Haut am gesamten Körper (einschließlich Kopfhaut) im Hinblick auf verdächtige Veränderungen.
Wenn sich der Allgemeinarzt bei einer Hautstelle nicht ganz sicher ist, überweist er Sie zur Sicherheit an einen Hautarzt. Der wiederholt das Hautkrebs-Screening. Dies ist aber kein Anlass zur Beunruhigung, denn meistens gibt der Hautarzt Entwarnung.
Auffällige Hautstellen sieht sich der Hautarzt mit einer speziellen Lupe (Dermatoskop) genauer an. Ergibt sich der Verdacht auf Hautkrebs, wird er eventuell eine Gewebeprobe (Biopsie) nehmen oder die auffällige Hautstelle unter lokaler Betäubung komplett entfernen und in ein Labor einschicken. Die sorgfältige feingewebliche Untersuchung des Gewebes bringt Gewissheit, ob es sich tatsächlich um Hautkrebs handelt. Sehr oft stellt sich aber heraus, dass es nur eine harmlose Hautveränderung ist.
Das Hautkrebs-Screening beinhaltet außerdem auch ein Beratungsgespräch über die Gefahr von UV-Strahlung (Sonne, Solarien).
Eigener Beitrag zum Hautkrebs-Screening
Hautkrebs und dessen Vorstufen lassen sich oftmals ohne aufwendige Hilfsmittel erkennen. Jeder Laie kann dazu beitragen. Entscheidend für die eigene Hautkrebs-Früherkennung ist es, die Haut regelmäßig nach Veränderungen zu untersuchen. Die Haut kann man nur dann gut untersuchen, wenn man sie gut sehen kann. Die Untersuchung sollte deshalb in einem hellen, gut beleuchteten Raum stattfinden.
Dabei sollte man vor allem auf jene Hautbereiche achten, auf welche die Sonne scheint, da hier Hautkrebs viel häufiger entsteht. An Körperpartien wie dem Rücken kann ein Spiegel oder die Untersuchung durch einen Bekannten/den Partner hilfreich sein. Besonders wichtig bei der Hautkrebs Früherkennung ist es, auf Veränderungen zu achten, die auf Schwarzen Hautkrebs hindeuten könnten, da dieser besonders gefährlich ist. Ausgerechnet dieser gefährliche Krebs tritt häufig auch auf Körperpartien auf, die dem Sonnenlicht nur selten ausgesetzt sind.
Wie kann man ein Malignes Melanom erkennen?
Bei der Früherkennung von schwarzem Hautkrebs kann die sogenannte ABCD-Regel hilfreich sein. Sie dient als Orientierung bei der Beurteilung von dunklen Hautflecken (Muttermal, Pigmentmal):
A (Asymmetrie): Wenn ein dunkler Hautfleck nicht rund oder oval, sondern asymmetrisch ist, sollte man ihn von einem Arzt begutachten lassen.
B (Begrenzung): Ein Muttermal ist normalerweise scharf von der umgebenden Haut abgegrenzt. Hat der Fleck dagegen Ausläufer in die umgebende Haut oder wirkt unscharf, verwaschen, könnte möglicherweise Hautkrebs dahinter stecken.
C (Colour = Farbe): Wenn ein Hautfleck verschiedene Farbtöne aufweist (beispielsweise hellbraun und tiefschwarz), ist dies auffällig. Ein Hautkrebs-Screening bringt Gewissheit.
D (Durchmesser): Jedes Muttermal, das einen Durchmesser von mehr als zwei Millimetern hat, muss beobachtet werden.
Wann sollten Sie zum Arzt gehen?
Die Eigenuntersuchung ist für die Hautkrebs-Früherkennung sehr wichtig. In Zweifelsfällen sollten Sie so bald wie möglich zum Arzt gehen. In folgenden Situationen ist ein Arztbesuch dringend empfehlenswert:
- Ein Pigmentfleck ist nach den Kriterien der ABCD-Regel auffällig oder verändert sich in Form, Farbe oder Größe.
- Ein Pigmentfleck beginnt zu brennen, zu jucken oder zu bluten.
- Es bilden sich raue Hautstellen oder Krusten. Dies kann auf weißen Hautkrebs hinweisen. Besondere Achtsamkeit sollte man den sonnenexponierten Stellen (Gesicht, Handrücken etc.) schenken.
- Wenn Sie überdurchschnittlich viele (mehr als 40) Pigmentflecken (Muttermale) haben, sollten diese grundsätzlich regelmäßig untersucht werden.
- Sie bemerken weiße Stellen am Zungenrand oder in der Mundschleimhaut.
Hautkrebs: Krankheitsverlauf und Prognose
Der Verlauf der Erkrankung hängt unter anderem davon ab, um welche Art von Hautkrebs es sich handelt. Während manche Tumoren nur langsam wachsen, breiten sich andere schnell aus und bilden frühzeitig Metastasen. Das erschwert die Behandlung von Hautkrebs. Die Heilungschancen verschlechtern sich ebenfalls mit dem Wachstum und der Ausbreitung des Tumors. Generell gilt: Die Heilungschancen bei Hautkrebs sind umso besser, je frühzeitiger der bösartige Tumor entdeckt und behandelt wird. Im Folgenden finden Sie nähere Informationen zu Verlauf der wichtigsten Formen von Hautkrebs, Heilungschancen und Prognose.
Basalzellkrebs
Der Basalzellkrebs wächst nur langsam, Außerdem verursacht er nur selten Absiedlungen (Metastasen) in anderen Organen. Das gilt auch noch in weit fortgeschrittenen Tumorstadien, wenn große Hautgebiete (zum Beispiel die gesamte Nase) vom Krebs zerstört wurden. Insgesamt hat das Basaliom deshalb eine gute Prognose: Es ist gut behandelbar, sodass bis zu 95 Prozent der Patienten wieder ganz gesund werden. Todesfälle sind selten: Nur ungefähr einer von 1.000 Patienten stirbt an der Krebserkrankung.
Rückfallrisiko: Regelmäßige Nachsorgeuntersuchungen nach Abschluss der Behandlung sind sehr wichtig. Bei mehr als vier von zehn Patienten bilden sich nämlich innerhalb der ersten drei Jahre nach Erstdiagnose weitere Basaliome. Geht man gewissenhaft zur Kontrolle, können diese neuen Tumoren frühzeitig entdeckt und behandelt werden. In welchen Abständen die Nachsorgeuntersuchungen sinnvoll sind, hängt vom Einzelfall ab. Der behandelnde Arzt wird jedem Patienten passende Termine vorschlagen. Experten empfehlen derzeit, diese Nachsorge nicht zeitlich zu begrenzen.
Stachelzellkrebs
Stachelzellkrebs wächst aggressiver als der Basalzellkrebs. Er zerstört dabei nach und nach das umliegende Gewebe. Unbehandelt kann sich ein Spinaliom im Körper ausbreiten und Metastasen in Lymphknoten und anderen Organen bilden. Das beeinflusst die Prognose: Wird Stachelzellkrebs entdeckt, bevor er Metastasen gebildet hat, ist er meist gut behandelbar. Sobald Tochterabsiedelungen auftreten, sinken die Heilungschancen. Statistisch gesehen endet die Krebserkrankung bei 40 bis 50 von 1.000 Patienten tödlich.
Rückfallrisiko: Wie beim Basaliom werden auch beim Spinaliom nach Abschluss der Therapie regelmäßige Kontrolluntersuchungen empfohlen (für mindestens fünf Jahre). Etwa die Hälfte der Betroffenen entwickelt nämlich innerhalb von fünf Jahren nach der Erstdiagnose einen neuen Tumor.
Schwarzer Hautkrebs
Die verschiedenen Typen von Schwarzem Hautkrebs zeigen unterschiedliche Verläufe: Manche Melanomtypen wachsen längere Zeit an der Hautoberfläche und lassen sich deshalb recht gut behandeln. Andere Typen dringen schnell in tiefere Gewebeschichten vor und breiten sich bald über Blut- und Lymphbahn im Körper aus. So bilden sich schon frühzeitig Metastasen. Die betroffenen Patienten können unbehandelt innerhalb weniger Monate sterben.
Abgesehen vom Melanomtyp beeinflusst auch das Tumorstadium zum Zeitpunkt der Diagnose die Heilungschancen. In Deutschland wird mehr als die Hälfte aller Malignen Melanome in einem frühen Stadium entdeckt. Fast alle der betroffenen Patienten können geheilt werden. Je später der Schwarze Hautkrebs aber entdeckt und behandelt wird, desto schlechter sind die Aussichten auf Heilung und desto höher ist das Sterberisiko. Generell gilt: Innerhalb von zehn Jahren nach der Diagnose “Malignes Melanom” sterben 15 bis 20 von 100 männlichen Patienten und 10 bis 15 von 100 weiblichen Patienten.
Rückfallrisiko: Wer schon einmal an Schwarzem Hautkrebs erkrankt ist, hat ein erhöhtes Risiko, erneut ein gefährliches Melanom zu entwickeln (Zweittumor). Deshalb sind die regelmäßigen Kontrolluntersuchungen nach Abschluss der Behandlung sehr wichtig. Diese Nachsorge bei Schwarzem Hautkrebs sollte sich über zehn Jahre erstrecken.
Additional information
guidelines:
- S3-Leitlinie “Prävention von Hautkrebs” der Arbeitsgemeinschaft Dermatologische Prävention (2014)
- Leitlinie “Diagnostik, Therapie und Nachsorge des Melanoms” der Deutschen Krebsgesellschaft und der Deutschen Dermatologische Gesellschaft (2018)
- Patientenleitlinie “Melanom” der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e. V., der Deutschen Krebsgesellschaft e. V. und der Deutschen Krebshilfe e. V. (2014)
Selbsthilfe:
- Deutsche Krebshilfe