Depression is a serious mental illness. The patients feel very depressed, lose their interests and are exhausted and impotent. The disease persists for a long time and usually does not improve on its own without treatment. How do you recognize depression, how does it develop and what therapies help? Read all important information about it here!

Depression: Short overview
- Main symptoms: deep depression, loss of interest, listlessness
- Besides symptoms: et al Insomnia, self-doubt, guilt, difficulty concentrating
- Therapy: various forms of psychotherapy and medications (antidepressants)
- Causes: partial genetic predisposition, mental injuries, disturbed messenger metabolism in the brain, stress
- Suicide risk: 10 to 15 percent of patients take their own lives. A therapy protects!
Depression – Symptoms
Depression is a serious mental illness that should be treated professionally. Unlike sadness and listlessness, which are part of life, depression does not disappear after a while and does not improve by distraction or encouragement.
Three main symptoms of depression
How to recognize depression Typical are the following three main symptoms:
Depressed mood: Those affected suffer very much from a deep depression. The depressive mood is almost uninterrupted, severe and lasting for at least two weeks.
Inner emptiness and loss of interests: A characteristic symptom of depression is also that the affected person feels neither joy nor other feelings. Inwardly, he feels empty and emotional. The interest in social contacts, work and hobbies expires. Attempted encouragement by the fellow humans have no effect. Even positive experiences do not improve the mood. Everything seems hopeless to them, so some lose the will to live.
Listlessness and tiredness: Coping with everyday tasks is difficult or even impossible for depressed people. They feel constantly mentally and physically exhausted. Even getting up in the morning becomes a feat, so that some people do not leave the bed because of their depression. Tiredness becomes normal.
Side symptoms of depression
Also typical for depression are the following secondary symptoms:
- strong self-doubt
- Guilt feelings and self-blame
- Concentration and attention disorders
- extreme need for sleep or insomnia
- strong restlessness and inner agitation
- Loss of sexual interest
Depression symptoms in men
In men depression is less often diagnosed. In part, it is because they often express themselves differently than women with depression. Aggression, severe irritability, low impulse control and low stress tolerance are common side effects. They take more risks than usual, for example driving cars way too fast. Often they consume more alcohol than usual or smoke more. They reproach their fellow human beings and are dissatisfied with themselves and the world. One reason could be that they feel the depressive feelings as weak and unmanly and therefore live out differently.
Attention, suicidal!
The negative thoughts can become so strong in severe depression that suicidal thoughts arise. In some depressive people, the risk of suicide is very high. About ten to fifteen percent of patients with depression die from suicide.
Searching for help! If you think of suicide yourself, or believe it could be the case with a relative, seek help without hesitation. The seemingly hopeless situation is a symptom of depression that can be overcome with the right support. First aid for depression and suicidal thoughts nationwide in the telephone counseling on 0800-1110111 and 0800-1110222. This is anonymous, free and accessible around the clock. The German Depressionsliga offers offers of self-help groups under www.depressionsliga.de.
Self-test for depression
Do you have the impression that you may be suffering from depression? Important notes are provided by online self-tests, such as the renowned Goldberg Test, developed by the psychiatrist Ivan K. Goldberg. Important: Such a self-test can not replace the diagnosis by a doctor or therapist. Be sure to seek help if the test gives this recommendation.
Physical symptoms in depression
Depression is often associated with physical complaints that have no identifiable organic cause. Such symptoms are called somatic. Typical physical symptoms include:
- Cardiovascular disorders
- Head and back pain
- Stomach and intestinal problems,
- sleep disorders
- anorexia
- rare also stronger appetite
- a morning low
- sexual aversion
somatization disorder
Sometimes the physical symptoms are so prominent that the depression is not immediately recognized. Physicians then speak of a somatic syndrome. The physical symptoms appear in phases and resolve with the treatment of depression again.
If the doctor does not find any organic cause for the symptoms, he can reveal the hidden depression as the actual cause by asking questions. If so, he will diagnose a so-called somatization disorder. This does not mean that the patients only imagine the symptoms, but only that the depression manifests itself in physical form.
Delusions and hallucinations of depression
A major depressive episode is sometimes accompanied by delusions and hallucinations. For example, the patients suffer from persecutory delusions or obsessional thoughts. Such delusional depressions are particularly difficult to treat. Besides antidepressants, antipsychotic medications are also used.
Sadness or depression?
Depression symptoms may be similar to those of deep grief. But there are crucial differences. This includes that in contrast to depression in a bereavement, the depressed mood does not always remain the same. Most mourners, despite their loss, are able to laugh and feel joy in between. People can not do that with depression.
In addition, the mood of mourners usually improves with time. Grief can recur abruptly due to the thought of loss. But gradually a mourning person will increasingly enjoy beautiful experiences again. The support of friends and family can be a comfort to him. In some cases, however, a mourning reaction turns into depression.
Depression – treatment
Every third person develops depression in the course of his life, says the statistics. A speedy treatment is then important, because those affected suffer greatly from their condition. In addition, therapy becomes more difficult and the risk of the disease becoming chronic increases.
Depending on the severity of the disease, depression is usually treated with psychotherapy, antidepressant medication, or a combination of both. The combination therapy is especially indicated for chronic and recurrent depression. Even with severe depression experts recommend a combination of both treatment approaches.
Psychotherapy for depression
For people with depression, there are many psychotherapeutic offers. At present, however, the coffers only cover the costs of cognitive behavioral therapy and so-called psychodynamic psychotherapies.
psychotherapy
Psychotherapy requires patient patience and commitment over a period of months. However, those who get involved can often overcome their depression in the long term and improve their overall psychological stability.
Cognitive behavioral therapy
In a cognitive behavioral therapy, the patient, with the therapist’s help, seeks ways to find out from the depression. Among other things, negative thoughts, patterns and beliefs are uncovered, checked for their correctness and, if necessary, replaced by new, more positive ways of thinking.
Psychodynamic psychotherapy
Psychodynamic psychotherapy is based on the idea that depression is often triggered by loss and excruciating experiences that could not be properly processed. These should be processed during the course of therapy. Psychodynamic psychotherapies include classical psychoanalysis as well as deep psychological psychotherapy.
Other types of psychotherapy for depression
Interpersonal Therapy (IPT) is a short-term therapy developed specifically for the treatment of depressive illness. She combines therapeutic concepts from behavior therapy and psychodynamic therapy. An important therapeutic goal is to learn skills and strategies for dealing with conflicts that contribute to the onset or maintenance of depression.
However, the costs for the ITP are not yet covered by the funds. This also applies to other forms of therapy such as systemic therapy, family therapy, Gestalt therapy or art therapy. However, they are often offered as supportive therapies for inpatient treatment.
This also applies to supplementary therapeutic measures such as psychoeducation, occupational therapy, groups of relatives, the learning of relaxation techniques as well as body and movement-related therapies.
Depression: drug therapy
Antidepressants can successfully treat the symptoms of depression. However, the effect often sets in only after weeks. The drugs are usually prescribed for more severe depression, or when the patient is opposed to psychotherapy.
However, there is no guarantee that the drugs will produce their desired effect. Each person responds differently to the active ingredients: some benefit greatly, in others, they hardly work, or the patients get especially the side effects felt.
If the medication is discontinued, there is a risk of relapse – especially if it happens abruptly. Therefore, do not stop taking antidepressants yourself, but discuss the procedure with your doctor!
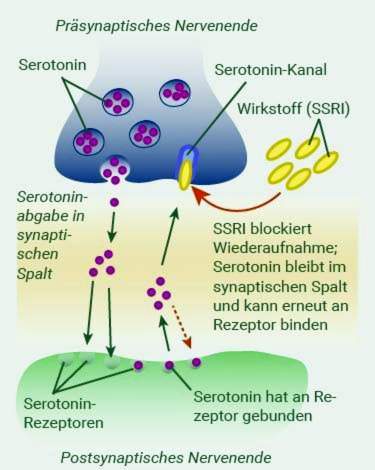
Selective serotonin reuptake inhibitors (SSRI)
Selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs) are currently being used to treat depression. They increase the level of “happiness hormone” serotonin in the brain and have a mood-enhancing effect. The drugs have significantly fewer side effects than older drugs. Typical side effects include nausea, inner restlessness and sexual dysfunction.
Tricyclic antidepressants
Tricyclic antidepressants are among the oldest drugs used for depression. However, they have strong side effects such as dry mouth, tremors, tiredness and constipation. Especially in older people can also heart arrhythmia and increased heart rate occur. Tricyclic antidepressants are therefore almost only prescribed if newer drugs do not work.
Monoamine oxidase inhibitors
The monoamine oxidase inhibitors (MAO) have long been used against depression. They have similar side effects as the tricyclic antidepressants. Special care should be taken with tranylcypromine. This ingredient requires a strict low tyramine diet. Tyramine is included in dairy products, wine and sausages, for example. If the patient does not avoid tyramine-rich foods, serious side effects such as hypertension may occur.
Other medicines for depression
Although lithium is not a classic antidepressant, it is often used as a mood stabilizer in depression. It should also reduce the risk of suicide.
St. John’s wort is a herbal remedy that can help especially in mild to moderate depression. The interactions with other drugs are problematic. For example, it reduces the effects of contraceptive hormone preparations.
Electroconvulsive therapy
With the help of electroconvulsive therapy can be treated in many cases, a depression in which fail medication and psychotherapy. Under short anesthesia by current impulses a short “epileptic seizure” is triggered. This idea may be frightening. In fact, the patient is unaware of the procedure and the risks are low.
wax therapy
For the wake therapy, patients need to stay awake for the second half of the night or the entire night. Although this method can not cure the depression, it can temporarily relieve the symptoms. Patients feel well for the first time in a long time, if only for a short time. Not only is this a tremendous relief, it also gives them the hope of actually overcoming their depression.
Depression – help for self-help
Recent studies have come to the conclusion that also offers of help without direct therapist contact can be helpful. One possibility is instructions for self-help. Those affected can read themselves a lot of information and have only occasional contact with an expert who supports them. This can help, for example, to bridge the waiting period until therapy.
Internet-based therapies and apps
Another alternative is professional advice over the internet. Therapy is performed using a special computer program. Meanwhile, there are also so-called depression apps and chatbots, which facilitate the management of depression. They are based on elements of Cognitive Behavioral Therapy.
Sport as an antidepressant
Out of the house, out of the depression! In depression, experts also recommend regular physical training. This can significantly reduce depressive symptoms – both in the short term and in the longer term. In fact, regular exercise can work just as well as an antidepressant. Explanations are the reduction of stress and possibly a change of messenger substances such as serotonin and norepinephrine.
However, the psychological effect of sport could have even greater impact: Patients come from the spiral of listlessness and withdrawal. They experience that they can do something for their own emotional well-being. Self-esteem is strengthened and hopelessness repressed. Those who do sports in a group also benefit from the sense of community and social contact, which usually gets less and less in depression.
Inpatient or outpatient therapy for depression?
A mild or moderate depressive phase can often be treated by outpatient psychotherapy. The hospitalization in a clinic is necessary especially for a severe depression. Medication, a variety of psychotherapeutic therapies and intensive care in the clinic help the patient to return to a structured daily routine.
If there is a high risk of suicide, depressive people can also be admitted to a clinic against their will.
Dealing with depressed relatives
Do you have the impression that a person close to you suffers from depression? Then you should encourage him to talk to a doctor about it. If the person concerned is lacking motivation, you may be able to take over the organization and possibly even accompany it. It is important to act fast! Because a depression usually does not disappear by itself. It tends to get worse if left untreated.
But also take care of yourself: supporting a depressed relative is extremely exhausting. The gloomy mood, listlessness and the loss of interest – even to partners, family and friends – can affect your own zest for life very much. Normally, a relationship is based on mutual give and take. But now you have to give patience, attention and support without getting back much. And maybe without the situation improving quickly.
This is stressful and frustrating. It is therefore normal for relatives to feel helpless and resourceful while feeling guilty. Admit these feelings. Not only your relative is affected by the disease, but you too!
As family members, they should therefore seek help. First, find out about the clinical picture of depression. A deeper understanding of the disease’s backgrounds and mechanisms is very important for proper management of the disease. Only then can you understand that a depressed person is unable to pull himself together and that encouragement attempts can not help.
Assistance sessions also give family support groups. Offers can be found on the pages of Federal Association of Relatives of Mentally Diseased People e.V. at www.bapk.de.
What you can do to help your loved ones and protect yourself from burnout, read in the text Depression – Relatives.
Depression: causes and risk factors
How depression develops is still not fully understood. However, it is assumed that there are always several factors interacting – internal and external. These include biological, genetic and psychosocial triggers. The size of the influence of the different factors varies from case to case.

Genetic influences
Twins and adoption studies have shown that depression also has a genetic root. The risk of developing depression is higher if other blood relatives are already ill. This is especially true when they became ill at an early age.
For example, if an identical twin suffers from depression, in about 40 percent of cases, the other develops depression. In dizygotic twins, this happens about half as often, so in 20 percent of cases. To a certain extent, depression is inheritable.
Vulnerability – susceptibility to depression
Vulnerability describes how vulnerable a person is to a mental disorder.
In people with high vulnerability, little stress can cause depression. But if the vulnerability is low, people can cope well with very stressful events. Such people are called resilient, so resilient. It is not only the objective severity of the burden that determines whether a person suffers from depression.
Significant influence also has the experience that a person has made in his life. For example, people who have had traumatic experiences such as abuse or neglect in their childhood have a particularly high risk of developing depression. However, it is also decisive what skills a person has acquired to cope with stressful situations.
Disturbed messenger metabolism in the brain
Nerve cells in the brain communicate with each other via electrical impulses and messenger substances, so-called neurotransmitters. There is evidence that this so-called brain metabolism is altered during depression.
For example, a disturbed noradrenaline or serotonin level in the brain tissue could be responsible for depression. If these are not in balance, this interferes with the exchange between the nerve cells. And that in turn affects feelings and thoughts negatively.

The fact that neurotransmitters in the brain actually play a role in depression is supported by the effects of antidepressant drugs such as serotonin reuptake inhibitors. However, this hypothesis does not explain why it usually takes weeks for the drugs to work.
Misregulated stress hormones
Other explanations suggest a dysregulation of the stress hormones epinephrine, norepinephrine and cortisol for depression. In particular, it has been found in depressed people an increased cortisol levels. This can be the trigger for, but also the result of depression.
Stress as a trigger
In fact, it is known that stress plays a crucial role in the onset of depression. Conversely, depression also causes stress itself. For example, by the loss of quality of life, but also when the profession can no longer be exercised or tensions with the social environment occur.
Some live hares are per se associated with increased stress. These include, for example, the puberty or the entry into the pension. In such phases, the risk of depression increases.
Even drastic life events are stressful. These include negative experiences such as job loss, separation or a serious illness. However, even positive events cause stress: Even with a promotion, the birth of a child or a wedding increases the likelihood of developing depression.
In fact, people with depression often report difficult events before the onset of the disease. In many cases, depression also appears from nowhere.
Negative thought patterns
It is not always the fate or the genes: The personal attitude to life has an impact on the risk of depression. People who think badly of themselves and about the world and see black for the future are more likely to get sick. However, good self-esteem and optimism protect against depression. You can do something about it: negative thinking patterns and ideas can be positively changed through appropriate exercises.
Female gender
Women are about twice as likely to suffer from depression as men. One possible explanation is that women are more vulnerable to hormonal fluctuations, such as menstruation.
Strong hormonal changes also bring with it a pregnancy that leads to a pregnancy depression in some women. The so-called postpartum depression or postpartum depression also affects many women.
Low socioeconomic status is also a risk factor for depression – and more women live in poverty than men.
In addition, depression is more rarely detected in men. Some are afraid to show weakness and seek help. But they also have atypical symptoms such as aggressive and excessive behavior.
Physical illnesses and depression
Some physical illnesses can also contribute to depression. Especially diseases of the brain and hormonal disorders such as hypothyroidism or hyperthyroidism affect the emotional world. In Cushing’s syndrome, for example, excessive amounts of cortisol are released in the adrenal cortex. The consequence is often a depressive phase.
Heavy and chronic diseases are also a constant burden on the psyche. Thus, people who suffer from cancer, severe cardiovascular diseases but also diabetes, often develop depression. It is also possible that the drugs used for treatment or associated with the disease physiological processes increase the risk of depression.
Conversely, depression can adversely affect the course of such diseases or, in some cases, promote their development. With such a combination of physical and mental illnesses, it is always important to treat mental and physical suffering equally.
Depression and somatoform disorders
In addition, depressions favor so-called somatoform disorders. These are chronic complaints for which no organic cause can be found. These include above all pain, for example in the back, stomach or joints. But also indigestion, heart problems or respiratory problems can be somatoform.
Additional mental illness
People with depression often suffer from other mental disorders. Again, it is important to recognize both diseases and treat them accordingly. These include
- anxiety disorders
- obsessive-compulsive disorder
- alcoholism
- personality disorders
- eating disorder
Winter depression: lack of light as a trigger
Some people are depressed only in the dark season – but every year. Depression in winter is one of the seasonal affective disorders (SAD = seasonal affective disorders). Symptoms such as lack of drive, loss of interest and depression are largely consistent with those of a classic depression, but are usually mild. Typical for a Witerdepression are also a pronounced need for sleep and cravings for sweets. That is why people with winter depression usually gain weight in the winter months.
The cause of the disorder is thought to be the lack of daylight, to which some people are particularly sensitive. In the dark, the body releases large quantities of the sleep hormone melatonin. Not only does this hormone make you tired, it also depresses your mood.

The most important therapy for the prevention and treatment of winter depression is light therapy. It reduces depressive phases, especially during winter depression. For this purpose, the patient sits for two weeks before sunrise and after sunset for 30 to 60 minutes in front of a device that exudes strong artificial daylight. If this is not enough, additional medication and psychotherapy can help.
If you want to know more about the topic, now read the article Winter Depression.
Medicines and drugs
Taking certain medications can also affect the mood. These include cardiovascular drugs such as beta-blockers, but also cortisone and related substances, hormonal contraceptives and some neurological medications such as antiepileptic drugs and Parkinson’s drugs.
Even drugs such as alcohol, cannabis and other substances that affect the psyche may favor the onset of depression.
Who suffers from depression?
People can get depression at any age. According to the Federal Health Survey, around three million people in Germany currently suffer from depression. Depression is so common – and they can affect anyone.
Depression in children and adolescents
Depression also affects young people: about one to two percent of pre-primary and primary school children and between three and ten percent of young people suffer from it. In rare cases, even very young children get sick. In children, however, depression is often not recognized.
How do depression manifest in children? Symptoms such as sadness and withdrawal are quickly classified in children as a hypersensitivity that comes naturally. Depression is also often different in children than in adults. Some get tantrums, others are extremely affectionate. Even smaller children are often difficult to describe their feelings. They then complain, for example, about stomachache or headaches, although actually the soul suffers.
For teenagers, melancholy and moodiness are also considered as normal side effects of this developmental phase. This may indeed be the case, but the cause is not infrequently also a depression requiring treatment. Because puberty as a time of upheaval with hormonal turbulence and stress makes young people particularly vulnerable to depression.
The relapse rate is particularly high in children and adolescents with depression. Because the mental disorder can permanently change the functions of the brain, which is still developing. That’s why fast and effective therapy is particularly important for young people. Help can be provided to children and adolescents specialized psychotherapists. In addition to a cognitive behavioral therapy, family therapy involving the family environment may be useful. For small children there is the offer of a play therapy.
If you want to know more about how depression manifests itself in children and adolescents and how to help them, read the article Depression in children and adolescents.
Age depression
For many people, aging is a process that primarily involves losses: retirement from work plunges many into emptiness and the feeling that they are no longer needed. The partner or good friends die. Physical fitness decreases and illnesses occur. All these changes strain and cause stress. That’s why the risk of depression increases with age. About 15 percent of people over 65 suffer from it. But this is often overlooked: 40 percent of the age depression remains undiagnosed.
Social withdrawal, exhaustion and depression are quickly misinterpreted as a result of natural aging processes. Even symptoms such as lack of concentration and forgetfulness are often rashly classified as incipient senile dementia.
It can be recovered with the help of an appropriate treatment even in old age many joie de vivre. Zur Therapie der Altersdepression eignen sich Antidepressiva ebenso wie eine Psychotherapie.
Wenn Sie mehr darüber erfahren möchten, wie sich Depressionen bei alten Menschen äußern und was man dagegen tun kann, lesen Sie den Beitrag Altersdepression.
Depression: Untersuchungen und Diagnose
Fürchten Sie an einer Depression zu leiden, sollten Sie dringend einen Arzt, Psychiater oder Psychotherapeuten kontaktieren. Eine Depression ist eine ernstzunehmende Erkrankung, die möglichst frühzeitig behandelt werden sollte. Je eher die Therapie beginnt, desto besser stehen die Heilungschancen.
Untersuchungen zur Depression
Als ersten Ansprechpartner können Sie Ihren Hausarzt aufsuchen. Dieser kann aufgrund von körperlichen Untersuchungen und einem ausführlichen Gespräch den Verdacht überprüfen. Folgende Fragen könnte der Hausarzt Ihnen in einem Erstgespräch stellen. Sie zielen auf Symptome ab, die typisch für Depressionen sind.
- War Ihre Stimmung in den letzten Wochen oft niedergeschlagen oder gedrückt?
- Haben Sie sich in letzter Zeit oft freudlos gefühlt?
- Waren Sie in letzter Zeit häufig antriebslos und müde?
- Hatten Sie in letzter Zeit gehäuft Selbstzweifel, Schuldgefühle oder negative Gedanken?
- Leiden Sie unter Schlafstörungen?
- Hatten Sie in letzter Zeit Schwierigkeiten, sich zu konzentrieren?
- Hat sich in letzter Zeit Ihr Appetit verändert?
- Wie lange dauern diese Symptome schon an?
Körperliche Auslöser
Schwieriger ist die Diagnose, wenn vor allem körperliche Symptome im Vordergrund stehen. Viele Patienten klagen über Kopf-, Rücken- oder Bauchschmerzen sowie Herz-Kreislauf-Probleme. Über körperliche Symptome zu reden, fällt vielen leichter, da diese gesellschaftlich akzeptierter sind als psychische Erkrankungen. Vor allem Männer betonen häufig stärker die körperlichen Anzeichen und gehen weniger auf ihre seelischen Symptome ein.
Physical examinations
Körperliche Ursachen der Symptome lassen sich anhand verschiedener Untersuchungen ausschließen. Dazu gehört eine Blutuntersuchung, unter Umständen auch eine Computertomografie (CT) des Gehirns. Denn auch ein niedriger Blutzuckerspiegel, Mangel an Vitamin B12, eine Demenz, eine Schilddrüsenunterfunktion sowie Veränderungen im Gehirn können depressive Symptome auslösen.
Die Diagnose Depression ist unwahrscheinlich, wenn manische Phasen auftreten, die eher auf eine Bipolare Störung hinweisen. Zudem kann auch ein Missbrauch von psychoaktiven Substanzen, beispielsweise Drogen, Symptome verursachen, die sonst an eine Depression denken lassen würden..
Bestätigt sich der Verdacht der Depressionserkrankung, wird der Arzt den Patienten an eine spezialisierte Klinik oder einen ambulanten Psychiater oder Psychotherapeuten überweisen.
Depressionen und andere Erkrankungen
Depressionen treten häufig in Kombination mit verschiedenen anderen psychischen Krankheiten und Störungen auf. Es ist wichtig, diese bei Depressiven zu erkennen. Denn die Therapie kann nur dann erfolgreich sein, wenn auch die anderen seelischen Probleme behandelt werden. Zu den seelischen Begleiterkrankungen von Depressionen gehören:
- Angst- oder Panikstörungen
- Suchterkrankungen
- Essstörungen
- Persönlichkeitsstörungen
- Demenzerkrankungen
Auch manche körperlichen Krankheiten gehen häufig mit Depressionen einher. Dabei scheinen körperliche und psychische Belastung sich gegenseitig zu verstärken. Dazu zählen vor allem
- Herz-Kreislauf-Erkrankungen
- Diabetes
Diagnose Depression
Die Diagnose einer behandlungsbedürftigen (klinischen) Depression erfolgt nach Ausschluss anderer Ursachen auf Basis der Internationalen Klassifikation von Krankheiten, ICD 10. Depressionen werden attestiert, wenn der Patient mindestens zwei der drei Hauptsymptome (depressive Stimmung, Intersaen- und Freudverlust, Antriebslosigkeit) und eines der Nebensymptome über mehr als zwei Wochen zeigt. Depressionen werden abhängig von der Zahl und der schwere der Symptome in drei Schweregrade eingeteilt: leicht, mittel und schwer (Major Depression).
Depression – Definitionen und Begriffsklärungen
Was man unter einer Depression versteht, hat sich im Laufe der Zeit mehrfach grundlegend verändert. Da auch veraltete Vorstellungen von Depression noch vielfach gebräuchlich sind, ist das verwirrend.
Definition der Depression heute
Experten klassifizieren heute eine depressive Episode nach ihrem Schweregrad und Verlauf als leichte, mittelschwere oder schwere Depression.
Von einer depressiven Episode spricht man, wenn mindestens über die Dauer von zwei Wochen zwei der drei Hauptsymptome (Niedergeschlagenheit, Interessenverlust und verminderter Antrieb) und zwei der sieben Zusatzsymptome (beispielsweise Schuldgefühle, Schlafstörungen oder Konzentrationsprobleme) auftreten. Im englischsprachigen Raum wird die depressive Episode als „major depression“ bezeichnet.
Endogene und exogene Depression
Noch vor einigen Jahren hat man Depressionen abhängig von den vermuteten Ursachen unterteilt: in endogene und exogene Depressionen. Diese Begriffe sind heute in der Fachwelt nicht mehr üblich, aber sonst noch weit verbreitet.
Unter einer „endogenen Depression“ verstand man eine Depression ohne erkennbaren äußeren Auslöser oder organische Ursache. Erklärt wurde dies durch veränderte Stoffwechselprozesse im Gehirn, beispielsweise aufgrund einer entsprechenden genetischen Veranlagung.
Schien ein konkreter Auslöser erkennbar, sprach man von einer „exogenen Depression“. Häufig wurde auch der Begriff „reaktive Depression“ oder auch „depressive Reaktion“ verwendet. Wenn als Ursache einer reaktiven Depression eine seelische Belastung angenommen wurde, bezeichnete man dies als “psychogene Depression“.
Depression oder Anpassungsstörung?
Heute spricht man von Anpassungsstörungen, wenn aktuelle seelische Belastungen eine Depression auslösen. Das kann der Tod eines geliebten Menschen oder Arbeitslosigkeit sein.
In solchen Fällen sind zwar depressive Symptome wie Trauer, Hoffnungslosigkeit und Antriebslosigkeit eine natürliche Reaktion. Bei manchen Menschen nehmen sie jedoch überhand. Häufig treten dann auch zusätzlich Störungen im Sozialverhalten auf.
Die Symptome einer Anpassungsstörung klingen meist spätestens nach sechs Monaten wieder ab. Die Störung kann jedoch auch in eine langfristige Depression übergehen.
Rezidivierende depressive Störung
Bei rund zwei Drittel der Patienten treten Depressionen wiederholt auf. Zwischen den Episoden können Monate liegen, aber auch viele Jahre.
Flackern die Depressionen immer wieder auf, ist das für die Patienten schwer zu ertragen. Ihr Leben wird stark eingeschränkt. Häufig können sie ihren Beruf nicht mehr ausüben. Auch ihre sozialen Beziehungen leiden unter den depressiven Phasen und können daran zerbrechen.
Je häufiger depressive Phasen auftreten, desto wahrscheinlicher wird ein weiterer Rückfall. Für Frauen ist die Wahrscheinlichkeit, dass die Depression wiederkehrt, höher als für Männer. Auch für Patienten, die jung oder erst im höheren Lebensalter an einer Depression erkranken, ist das Risiko erhöht.
Chronische Depressionen und Dysthymia
Bei manchen Menschen verläuft die Depression nicht in Phasen, sondern sie leiden durchgehend unter depressiven Symptomen. Allerdings sind die Beschwerden meist weniger stark ausgeprägt als bei einem episodischen Verlauf. Mediziner bezeichnen das dann als Dysthymia. Kennzeichnend ist, dass die Betroffenen über einen Zeitraum von mindestens zwei Jahren durchgängig oder regelmäßig unter depressiven Symptomen leiden.
Die möglichen Auslöser sind vielfältig. Untersuchungen zeigen jedoch, dass Patienten mit chronischen Depressionen häufiger als andere Depressionspatienten traumatische Erfahrungen wie Missbrauch gemacht haben.
Diese Form der Depression wird häufig nicht erkannt – sogar den Betroffenen selbst erscheint ihre niedergedrückte Stimmung inzwischen häufig normal. Das erschwert ihnen auch die Erkenntnis, tatsächlich krank zu sein. Trotzdem beeinträchtigt auch eine weniger starke chronische Depression erheblich Lebensqualität, Leistungsfähigkeit und soziale Beziehungen der Patienten. Sie sollte daher unbedingt behandelt werden. Auch hier kann eine Kognitive Verhaltenstherapie helfen. Noch wirksamer sind bei dieser Depressionsform aber Medikamente.
Wenn Sie mehr zum Thema Dysthymia erfahren möchten, wie sie sich auswirkt und was man dagegen tun kann, lesen Sie den Text Dysthymia.
Bipolare Störung
Sobald neben den depressiven auch manische Phasen auftauchen, liegt eine Bipolare Störung vor. Auch diese gehört zu den Affektiven Störungen, ist aber streng genommen keine Depression. Die Betroffenen pendeln dann zwischen zwei emotionalen Polen: Niedergeschlagenheit und Antriebslosigkeit einerseits und extremer Euphorie, Selbstüberschätzung und übertriebenem Aktionismus andererseits. Eine bipolare Störung ist oft schwerer zu behandeln als eine klassische Depression.
Agitierte Depression
Eine agitierte Depression äußert sich in ängstlicher Getriebenheit. Die Betroffenen laufen unruhig umher und klagen über Luftnot und Herzrasen. Eine agitierte Depression wird daher auch als „Jammerdepression“ bezeichnet.
Während Depressive sonst eher Schwierigkeiten haben, sich zu irgendeiner Handlung aufzuraffen, haben Menschen mit agitierter Depression einen ständigen Bewegungsdrang. Ihr Verhalten ist hektisch und ziellos.
Atypische Depression
Im Unterschied zur klassischen Ausprägung einer Depression lässt sich die Stimmung bei der atypischen Depression durch positive Ereignisse verbessern. Weitere Anzeichen sind gesteigerter Appetit und ein starkes Bedürfnis, tagsüber zu schlafen. Die Betroffenen geben sich häufig sehr theatralisch und sind leicht zu kränken.
Die atypische Depression ist nicht selten. Etwa 13 bis 36 Prozent der depressiven Patienten sind davon betroffen. Diese depressive Störung tritt überwiegend bei Frauen auf.
Depression: Krankheitsverlauf und Prognose
Depressionen verlaufen von individuell ganz unterschiedlich. Den meisten Menschen, die unter einer Depression leiden, kann aber durch eine konsequente Behandlung gut geholfen werden. Das gilt auch für ältere Menschen! Die Therapie ermöglicht es, depressive Episoden zu durchbrechen oder vollkommen abklingen zu lassen. Eine Depression heilen ist also möglich!
Unbehandelt ist die Wahrscheinlichkeit allerdings hoch, dass eine Depression über Monate oder Jahre bestehen bleibt. Das gilt insbesondere für schwere Depressionen. Je früher die Behandlung begonnen wird, desto besser sind die Aussichten.
Ein Drittel der Betroffenen erlebt nur einmal im Leben eine depressive Episode. Die Chancen dafür stehen besonders gut, wenn sie frühzeitig adäquat behandelt werden. Mit jedem Rückfall steigt allerdings die Wahrscheinlichkeit, dass weitere depressive Phasen auftreten. Besonders schwer zu heilen sind chronische Depressionen. Sie werden nicht selten zum lebenslangen Begleiter und bedürfen ständiger Behandlung.
Suizidrisiko bei Depressionen
Etwa zehn bis fünfzehn Prozent der Menschen mit Depressionen nehmen sich das Leben. Für Patienten mit einer chronischen oder sehr schweren Depression ist diese Gefahr besonders hoch.
Eine Komorbidität, beispielsweise mit einer Angststörung, erschwert oft die Behandlung der Depression. Bei Patienten, die zusätzlich an einer Angststörung leiden, entwickelt sich die Erkrankung häufig ungünstig. Ebenso ungünstig ist es, wenn eine Depression bereits in jungen Jahren auftritt, und wenn der Patient keine ausreichende eine soziale Unterstützung hat.
Additional information
book recommendations
- Positives Denken lernen: Wie Sie durch positive Gedanken Ihr Wohlbefinden steigern Taschenbuch (Markus Pfeil, 2017, CreateSpace Independent Publishing Plattform)
guidelines
- S3-Leitlinie und Nationale VersorgungsLeitlinie (NVL) „Unipolare Depression“ der Deutschen Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde (Stand: 2015)
Support Groups
- Deutsche Depressionsliga e.V.
- Deutsche Depressionshilfe