Measles are a highly contagious, feverish viral infection. It usually begins with flu-like symptoms before the typical measles rash develops. In most cases, measles cure easily on their own. Sometimes it comes to complications such as otitis, pneumonia or a dangerous brain inflammation. Particularly susceptible are children under the age of five and adults. Read everything important about measles here!

Quick Overview
- What are measles? Highly contagious viral infection that is distributed worldwide. It is one of the “teething troubles”, although increasingly also adolescents and adults get sick.
- Infection: Droplet infection, direct contact with infectious nasal or pharyngeal secretions of patients (e.g., by sharing cutlery)
- symptoms: In the first stage flu-like symptoms, a first fever, and whitish patches on the oral mucosa (Koplik spots). In the second stage, the typical measles rash (red, blurred patches from the ears) and a second fever.
- Treatment: Bed rest, protection, possibly fever-reducing measures (such as antipyretic drugs, calf wrap), cough medicine, antibiotics (with additional bacterial infection)
- Possible complications: e.g. Middle ear infection, pneumonia, bronchitis, diarrhea, pseudo-Krupp (Krupp’s syndrome), encephalitis (encephalitis); Long-term consequence: chronic brain inflammation (subacute sclerosing panencephalitis, SSPE)
- Forecast: Measles usually heal easily. Complications occur in this country in 10 to 20 percent of patients. About one in every 1,000 people can die.
Measles: infection
The transmission of the measles viruses takes place on the one hand droplet infection: Infected people spread tiny, virus-containing saliva droplets in the ambient air when talking, coughing and sneezing. Other people can inhale these: Once the viruses in the saliva droplets have contact with the mucous membranes in the airways, they can infect the new “victim”. Incidentally, measles viruses can survive in the air for up to two hours!
On the other hand, one can also get by with measles direct contact with infectious secretions from the nose and throat of infected infected. This happens, for example, when you use the cutlery or drinking glass of patients.
Measles viruses are extremely contagious! Out of every 100 people who had no measles and who have not been vaccinated against it, 95 contracted contact with measles viruses.
How long are measles patients contagious?
Anyone who has become infected with measles is already contagious three to five days before the onset of the typical measles rash and up to four days later. The greatest is the contagiousness immediately before the eruption of the rash.
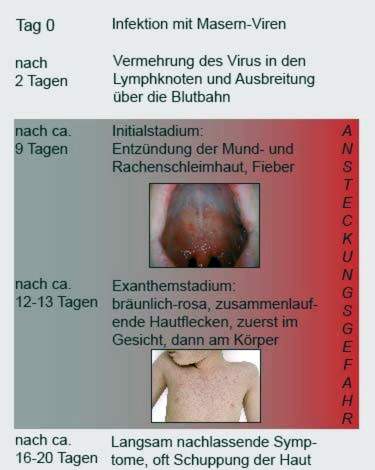
Measles: incubation period
The time between infection with a pathogen and the onset of the first symptoms is called the incubation period. It is usually eight to ten days for measles. The typical measles rash (second disease stage) usually occurs two weeks after infection.
Measles: symptoms
Measles in two disease stages with two fever episodes and other symptoms:
Precursor stage (prodromal stage): The disease starts with moderate fever, runny nose, sore throat and dry cough. The face is bloated. Also fatigue, headache and abdominal pain, constipation or diarrhea and conjunctivitis with photophobia are possible symptoms. The so-called Koplik patches on the oral mucosa are typical in the early stages of measles: these are circumscribed, small, red spots with a white center (“lime splash spots”). They form on the cheek mucosa in the area of the molars as of the second or third day of illness. From the 3rd day the entire oral and pharyngeal mucosa becomes red. In addition, the fever rises sharply.
The precursor stage lasts about three to four days. Towards the end, the fever initially drops again.
Main stage (exanthema stage): In this disease phase, the fever rises again steeply. It develops the typical measles rash: irregular, three to six millimeters large, initially bright red spots that flow into each other. They first form behind the ears and then spread out over the whole body. Only palms and soles are left out. Within days, the spots become darker, brownish-purple.
After four to seven days, the Masen patches will fade again, in the same order in which they occurred (starting from the ears). This fading is often associated with a dandruff. At the same time, the other complaints sound as well.
It takes about two weeks for the patient to recover. But the immune system is weakened even longer: For about six weeks there is an increased susceptibility to other infections.
Mitigated measles
In newborns who still have measles antibodies in their mothers, a measles infection is usually attenuated. Such “mitigated measles” can sometimes be observed in other people. These include patients who have not received the full measles vaccine and therefore have weak, incomplete protection. With mitigated measles the typical rash is not fully developed. This can make the diagnosis more difficult. Nevertheless, those affected are contagious.
Measles: complications
Occasionally, a measles infection involves complications. Due to the multi-week immune deficiency other pathogens such as bacteria easy game. It is most commonly associated with measles Otitis (Otitis media), bronchitis, lung infection (Pneumonia) and Diarrhea diseases.
Also possible is a strong inflammation of the laryngeal mucosa. Doctors also speak of Krupp syndrome or pseudo-group, Those affected especially have attacks of dry, barking coughing and difficulty breathing (even short of breath), especially at night.
Rarely are foudroyant (toxic) measles: The affected patients get, among other things, high fever and skin and mucous membrane bleeding. The mortality from this measles complication is high!
Another rare but dreaded complication is one encephalitis (Encephalitis). About four to seven days after the onset of the measles rash, she becomes aware of headaches, fever and disturbances of consciousness (even coma). About 10 to 20 percent of the patient die. In another 20 to 30 percent, measles-related encephalitis causes permanent damage to the central nervous system.
Very rarely on average six to eight years after the measles infection, an always fatal, late complication occurs – a chronic inflammation of the brain, which is known as subacute sclerosing panencephalitis (SSPE) refers to: measles viruses that invade the brain multiply, causing irreversible nerve damage. First, behavioral changes show up. In the further course, neurological disorders such as muscle twitching and seizures as well as nerve breakdowns are added. In the end stage, all brain functions fail – the patient dies.
Of 100,000 measles patients four to eleven get a SSPE. Particularly vulnerable to this fatal sequel of measles are children under five years old. There are an estimated 20 to 60 SSPE cases per 100,000 measles patients in this age group.
In people whose immune system is suppressed by medication or other disease (immunosuppression) or has a congenital defect, the measles may be quite weak on the outside. The measles rash may be missing or atypical. However, there is the Danger of severe organ complications, This includes a progressive form of pneumonia (Giant cell pneumonia). Sometimes a special type of encephalitis develops (Measles Inclusion Body Encephalitis, MIBE): It causes death in about three out of ten patients.
Measles: causes and risk factors
Measles are caused by the highly contagious measles virus. The pathogen belongs to the paromyxovirus family and is distributed worldwide.
Of particular importance is the disease in African and Asian developing countries: measles are among the ten most common infectious diseases and often end in death.
In Germany, the number of measles illness has decreased since the introduction of the measles vaccine. For some years now, it has been less than 2,000 cases per year for the most part. However, there are always temporary regional or nationwide measles outbreaks. In addition, it has been observed for some years that increasingly adolescents and (young) adults get “teething troubles”.
Measles: examinations and diagnosis
The disease symptoms, especially the rash, give the physician important evidence of measles. However, there are some diseases with similar symptoms, namely rubella, marigold and scarlet fever. To prevent confusion, therefore, a laboratory examination must confirm the measles suspicion. Various tests are possible, with evidence of antibodies against measles viruses being the most common:
- Detection of Specific Antibodies to the Measles Virus: fastest and safest diagnostic method. As sample material blood of the patient is used (in suspected brain inflammation possibly nerve water = cerebrospinal fluid). The test is usually positive as soon as the typical measles rash appears. But sometimes the antibodies are not detectable yet.
- Detection of the viral genome (measles virus RNA): For this purpose, a urine sample, saliva sample, tooth bag fluid or a throat swab is taken. The viral genetic traces found therein are amplified by means of the polymerase chain reaction (PCR) and can thus be clearly identified.
- Cultivation of measles viruses: For this purpose, sample material (urine sample, saliva sample, etc.) is exposed to optimal growth conditions in order to culture the contained pathogens. That’s how they can be identified. This procedure is very time-consuming and is only done in special cases (eg in patients with suppressed immune system).
Measles are notifiable!
Measles belong to the notifiable diseases. As soon as first symptoms indicate measles, the doctor should be consulted. The suspicion, the actual illness and also the death of measles must be reported by the doctor to the responsible health authority (with the name of the patient).
If measles or a proven infection is suspected, those affected must keep away from community facilities (schools, day-care centers, etc.). This also applies to employees of such facilities. Patients may be re-admitted no earlier than five days after the eruption of the measles rash.
Measles: treatment
There is no specific therapy for measles. But they can alleviate the symptoms and support the healing process. This includes bed rest in the acute disease phase and physical conservation, If the eyes of the patient are sensitive to light, the hospital room should be something darkened be – direct light on the patient should be avoided. Also make sure that the room well ventilated and not stuffy.
Experts recommend measles patients, to drink enough – especially with fever and sweating. Instead of a few large protions should be distributed over the day several small meals be consumed.
For example, help against the fever Wadenwickel and if necessary antipyretic drugs, The use of the medication should be discussed with a doctor first. The same is true if you cough medicine Want to use (cough remover or cough blocker).
The fever and painkiller acetylsalicylic acid (ASA) is not suitable for children. Otherwise, the rare but life-threatening Reye Syndrome can develop in conjunction with feverish infections!
In an additional infection with bacteria (such as middle ear or pneumonia), the doctor prescribes mostly antibiotics.
If the measles cause Krupp syndrome or encephalitis is one Treatment in the hospital necessary!
Measles: disease course and prognosis
Measles heal easily in most patients. In 10 to 20 percent of cases, however, complications occur. Affected are above all children under five years and adults over 20 years. Such measles complications can also be fatal. This is especially true for brain inflammation that develops either shortly after infection or as late complications years later. According to the World Health Organization (WHO), the death rate for measles in developed countries such as Germany is up to 0.1 percent (1 death per 1,000 measles patients). In developing countries, it can be significantly higher, for example due to malnutrition.
Lifelong immunity
You can get measles only once in your life: Anyone who has survived an infection is protected for life against a renewed infection with measles viruses. In the case of infection, the immune system forms specific antibodies against the pathogen. Part of it remains in the body after healing. If it comes later to a renewed contact with measles viruses, the antibodies become immediately active and eliminate the intruder.
Pregnant women who have antibodies to measles transfer them to the unborn child via the umbilical cord. The maternal antibodies remain in the child’s body until a few months after birth and thus prevent an infection. This so-called nest protection continues until about the sixth month of life.
Measles vaccination
Measles can cause rare but serious complications, including deaths. Therefore, the Standing Committee on Vaccination (STIKO) at the Robert Koch Institute (RKI) recommends that all infants, toddlers as well as unvaccinated adults be vaccinated against measles.
On July 17, 2019, the Federal Cabinet decided to take measles. Accordingly, a measles vaccine is prescribed for children who attend childcare. The same applies to school children. But even adults who work in community facilities such as teachers, kindergarten teachers and medical staff, are subject to vaccination, if they have not already undergone the measles. Likewise refugees who live in a refugee shelter.
The measles vaccine is a so-called live vaccine, It therefore contains attenuated measles viruses that have lost all or part of their pathogenic effects. Nevertheless, the immune system reacts with the formation of specific antibodies against the measles virus (therefore, the measles vaccine is a so-called active vaccination). This antibody production takes some time, but after four to six weeks, the specific antibodies in the blood are detectable.
But the measles vaccine can develop its full protective effect two vaccine doses necessary: The first dose is usually given to infants between the ages of 11 and 14 months. The second should be given between 15 and 23 months (at the earliest four weeks after the first dose of vaccine).
The measles vaccine is usually given together with the mumps and rubella vaccines. This combination vaccination is known by the abbreviation MMR vaccine.
Also, adults who are not subject to vaccination should, according to STIKO’s recommendation, make up for the measles vaccination of the MMR vaccine in the form of a single dose, provided that
- they have not received such a vaccine (or all recommended vaccine doses) as a child or
- It is unclear whether they have been vaccinated (unclear vaccination status).
This is especially true for Adults after 1970 were born. In this age group many are neither vaccinated nor have they undergone the measles as a child. Measles cause more serious complications in adults than in children.
Possible side effects of measles vaccine
The measles vaccine is generally well tolerated. Sometimes it comes at the injection site to redness, swelling and pain. In addition, adjacent lymph nodes can swell. Also, an increased body temperature, fatigue, headache and gastrointestinal discomfort are possible. Such complaints are only temporary and will soon be over.
In about five percent of the vaccinees usually develop in the second week after the so-called vaccine. This is used to describe attenuated measles symptoms such as moderate fever, a mild rash and respiratory ailments. These vaccines are not contagious!
Post-exposure vaccination
If unprotected people have had contact with a measles patient, they can get vaccinated up to three days later. This can usually prevent a disease outbreak. For this “emergency” vaccine, the combination vaccine against measles, mumps and rubella (MMR vaccination) recommended.
In immunocompromised people, the postexpositional measles vaccine can also by means of passive immunization done: Two to six days after the (suspected) infection are already injected antibodies against measles viruses. This provides the vaccinee with immediate protection as opposed to “normal” (active) measles vaccination. However, this only lasts for a limited time: the “foreign” antibodies are gradually broken down by the immune system.
Pregnant women and children under the age of six months may also receive passive immunization after measles infection. The active one measles-Vaccination is not allowed during pregnancy (no live vaccines! 9 and not approved for children under six years.
Additional information
guidelines:
RKI guidebook “Measles” of the Robert Koch Institute (2014)