The Gastric bypass (gastric bypass) refers to a surgical procedure in which a large part of the stomach and the small intestine are bypassed in obese people and thus eliminated. It remains only a small gastric remnant, the patients feel therefore already after very small amounts of food a feeling of satiety. The result is a fast and significant weight loss. Find out everything about the operation, its advantages and risks here!
What is a gastric bypass?
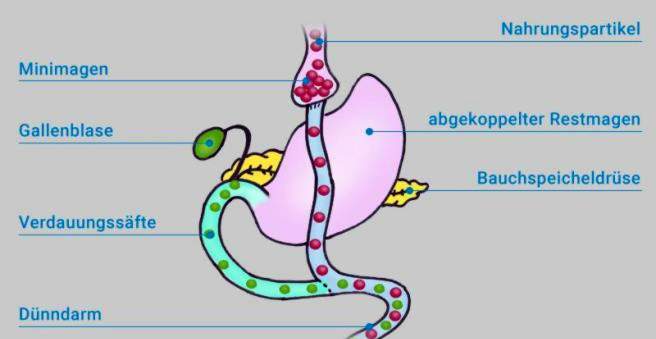
The gastric bypass (more precisely, Roux-en-Y gastric bypass) is a very commonly used method of obesity surgery with the aim of weight loss. The name derives from the name of the Swiss surgeon “Roux”, who developed the basic technique of the procedure. The “Y” stands for the shape in which the intestinal sections are joined together, namely Y-shaped.
The success of gastric bypass is based on two principles:
- a stomach reduction to reduce the amounts of food (restriction)
- the elimination of the important upper small intestine portion (duodenum), whereby the digestive juices important for the food splitting mix later with the chyme (worse nutrient absorption = malabsorption)
The weight loss after a gastric bypass is very effective and reliable, but it is provided with some lifelong restrictions: patients with a Reoux-en-Y bypass tolerate only very small meals, because the remaining after surgery residual stomach (“stomach pouch”) only has a very small volume. In addition, the poorer nutrient utilization requires that patients take certain dietary supplements and vitamins (especially vitamin B12, trace elements and protein preparations) for life, in order to avoid any deficiency symptoms. Since some of the nutrients remain undigested, fermentation processes in the large intestine can increasingly occur. The surgery can hardly be reversed after successful weight loss.
Preparation for gastric bypass
Before surgery, pathological changes in the stomach must be ruled out. For example, the stomach is examined for diseases such as gastritis or gastric ulcer and a possible germ colonization with the bacterium “Helicobacter pylori”, which can cause stomach ulcers. In addition to a gastroscopy and the examination of gastric juice, an ultrasound of the upper abdomen is also used, with which gallstones can be detected. These should be removed as part of the gastric bypass surgery, as they can lead to inflammation of the gallbladder and bile duct.
Course of gastric bypass surgery
The gastric bypass surgery takes about 90 to 150 minutes depending on the patient and is performed under general anesthesia. The procedure usually requires hospitalization of about one day prior to surgery (surgical and anesthetic preparation) plus five to seven days thereafter. After gastric bypass surgery, you will not be able to work for about three weeks.
The gastric bypass is today almost exclusively performed as a so-called minimally invasive surgery. This technique, also known as the “keyhole method”, does not require a large abdominal incision. Instead, the instruments and a small camera are inserted into the abdomen via several skin incisions about two centimeters in size. Overall, minimally invasive surgery has a lower surgical risk than open surgery and is therefore particularly suitable for obese patients, who are in any case more vulnerable to complications during and after surgery.
The gastric bypass surgery consists of several stages:
- After initiating general anesthesia, the surgeon inserts the instruments and a camera with a light source into the abdomen through several skin incisions. Thereafter, a gas (usually CO2) is introduced into the abdominal cavity, so that the abdominal wall lifts slightly from the organs and thus the surgeon has more space in the abdominal cavity and a better view of the organs.
- First, the stomach just below the esophagus is separated by a so-called stapler (“Stapler”). The stapler cuts and staples at the same time, so that the cut edges are immediately closed. Thus, at the end of the esophagus only a small remaining stomach remains (the so-called gastric pouch or stomach pocket). It has a volume of less than 50 milliliters. The rest of the stomach remains in the body, but is closed at the top and so to speak “shut down”.
- Next, a section through the small intestine in the area of the so-called jejunum (“jejunum”). The lower cut end is now pulled up and sewn to the stomach pouch. Therefore, the compound is also called Gastrojejunale anastomosis.
- Now further below the remaining, cut end of the jejunum with the third small intestine section (“ileum”) is sutured, so that the shape of a “Y” is formed (Y anastomosis). Here only the digestive juices from the duodenum (bile and pancreatic secretions) mix with the chyme.
For whom a gastric bypass is suitable
The gastric bypass is suitable for people with a body mass index (BMI) above 40 kg / m² (obesity grade III or obesity permagna). In any case, the precondition for gastric bypass surgery is that all non-surgical measures have not shown sufficient success even after six to twelve months. These measures include, for example, professional nutritional counseling, exercise training and behavioral therapy (Multimodal Concept for Obesity, MMK). For the gastric bypass surgery should be at least 18 and not more than 65 years old, the operation in individual cases, even in younger or elderly people is possible.
A gastric bypass is particularly recommended for people whose overweight is mainly due to a high consumption of high-calorie food (sweets, fats) and sweet drinks. Because these are now split worse and therefore can be used by the body only to a small extent and stored as body fat.
If there are already metabolic diseases such as diabetes mellitus, high blood pressure or a sleep apnea syndrome due to the excess weight, a gastric bypass may be useful from a BMI of 35 kg / m².
For whom a gastric bypass is not suitable
Various physical and mental illnesses speak against an obesity operation such as gastric bypass. Especially after previous operations or malformations of the stomach, gastric ulcers and addictions as well as untreated eating disorders such as binge eating or bulimia, no gastric bypass should be used. Even pregnant women have to do without a gastric bypass.
Effectiveness of gastric bypass surgery
Gastric bypass is a very effective procedure, but few patients achieve normal weight (BMI ≤ 25 kg / m²). Studies have shown that with a gastric bypass in the long term, a weight loss of about 60 to 70 percent of the overweight is possible, ie the weight that separates the person from the normal weight.
The weight loss after gastric bypass surgery has in addition to the purely cosmetic effect, especially beneficial effects on the metabolism. For example, the intervention in many cases, an existing diabetes mellitus (diabetes mellitus) greatly improved and sometimes even cured. In many cases, blood glucose levels drop even shortly after surgery, although the patient has not lost significant weight. The reasons are not yet clear. It is believed that the operation will initiate various hormonal changes (for example, the hormones ghrelin, glucagon, GIP, etc.), which have a beneficial effect on the metabolism.
Benefits of gastric bypass over other procedures
Because gastric bypass surgery combines two principles (restriction and malabsorption, see above), the procedure is extremely effective and is particularly effective when patients are overweight resulting from excessive intake of high calorie liquid or soft foods. For these so-called “sweet-eater” alone would be a reduction of the gastric volume, as it is achieved by the gastric band, the gastric balloon or the tube stomach, not enough.
side effects
The gastric bypass is associated with some side effects. How strong these are will vary individually and therefore can not be predicted with certainty. The important ones include:
Indigestion due to malabsorption: Flatulence, abdominal pain, nausea, feeling of fullness
Iron deficiency and anemia (anemia): Normally, a large part of the food-grade iron is taken up in the duodenum. Since the gas is bypassed the food at the duodenum, iron absorption is difficult. The iron deficiency is prevented by an additional gift of iron.
Vitamin B12 deficiency (special form of anemia): Vitamin B12 is taken up on the last section of the small intestine (terminal ileum). But this is an adjuvant, the so-called intrinsic factor (“intrinsic factor”) required, which is formed by the stomach. Gastric bypasses, however, the food is passed by the stomach and thus formed less intrinsic factor. Vitamin B12 must therefore be regularly injected into the muscle as a syringe to the vein. There are also vitamin B-12 preparations available that are absorbed directly through the oral mucosa (sublingual application). Their effectiveness is still discussed.
Vitamin D deficiency: Why it can come with a gastric bypass to a vitamin D deficiency, is not yet clear. Vitamin D can be easily supplemented with food (orally).
Dumping syndrome: A dumping syndrome (dulling syndrome) is a series of symptoms (dizziness, nausea, sweating, or palpitations) that can result from instantaneous (fall-like) depletion of food from the esophagus to the small intestine. For the stomach pouch is missing the lower gastric sphincter (porter). The porridge attracts in the small intestine by osmotic forces water from the surrounding tissue and the blood vessels. This reduces the volume of fluid in the circulation, which can lead to a fall in blood pressure. A dumping syndrome occurs mainly after very sugary drinks or fatty foods.
Gastric ulcer in the stomach pouch: After gastric bypass surgery, the risk of gastric ulcer is increased in gastric pouch. Help is provided by acid-reducing medications, so-called proton pump inhibitors (PPIs), which must be taken permanently if gastric ulcer develops after gastric bypass surgery.
Loss of muscle mass: A fast weight loss is often associated with a loss of muscle mass because the organism tries to balance the relative lack of carbohydrates by breaking down body protein (especially from less stressed muscle cells). Regular exercise can stop this effect. For overweight people, above all, joint-sparing sports such as light weight training, cycling, swimming or aqua-jogging are advisable.
Gastric bypass: risks and complications
Gastric bypass is a major abdominal surgery that severely changes the normal anatomy of the gastrointestinal system. Basically, the surgical risk is low, but complications can not be ruled out, as with all surgical procedures. Non-specific operational risks include:
- anesthesia complications
- Organ and vascular injuries with bleeding
- Infections of internal and external wounds
- Leakage of artificial organ connections (anastomoses) with the risk of peritonitis (peritonitis)
- wound healing
- Disorders of normal gastrointestinal movements (intestinal atony)
Gastric bypass: diet after surgery
People with a gastric bypass must follow the following nutritional rules for life, to avoid digestive problems:
- Chew food very well
- eat small portions
- Avoid very sugary foods and drinks
- refrain from very long-fiber meat or vegetables
- Take a dietary supplement (see above)
Medicines after gastric bypass
Some medications are absorbed by the body after a gastric bypass with altered dynamics or in a lesser amount. Many medications therefore require dose adjustments by the physician.
Gastric bypass: cost
The costs of a gastric bypass vary considerably depending on the clinic. They are between about 6,500 and 15,000 euros. The gastric bypass is currently not a regular benefit of the statutory health insurance. That means the cost of gastric bypass only be accepted on request and only under certain conditions. Inform yourself before the application in detail about the necessary conditions!