A heart attack (myocardial infarction) occurs when a blood vessel of the heart muscle (coronary artery) closes. The muscle is then cut off from the oxygen supply and can no longer do its job. A heart attack can be life threatening! Therefore, it is important to recognize the symptoms of a heart attack as early as possible. Here you read all important information about warning signals, causes and treatment options and first aid for heart attack.

Heart attack: short overview
- Typical symptoms: severe pain in the left chest / behind the sternum, shortness of breath, anxiety / anxiety; Warning, the symptoms in women can be different (dizziness, vomiting) than in men!
- First aid: Call the emergency doctor, calm the sick, lift up the upper body, loosen tight clothing (tie, collar, etc.), if there is no consciousness and lack of breathing immediate revival!
- Risk factors: High blood pressure, high cholesterol, overweight, little exercise, diabetes, smoking
- Reason: usually a blood clot that clogs a coronary artery
- Important investigations: ECG, cardiac ultrasound, blood tests, cardiac catheterization
- Treatment options: Expansion of the constricted heart vessel (balloon dilation) and insertion of a stent within the framework of a PTCA, dissolution of the blood clot (lysis therapy), other medications, bypass surgery
- Prevention: healthy lifestyle, regular exercise, healthy body weight
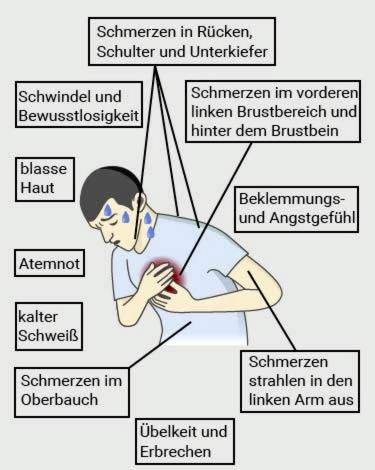
Heart attack: symptoms
In a heart attack, there is no time to lose. The sooner he is recognized and treated, the greater the chances of survival. That’s why you should have the slightest suspicion and first symptoms of myocardial infarction dial the emergency call (Tel. 112) – also at night or on weekends!
However, to be able to react quickly, one must know the heart attack symptoms in man and woman. But beware: not always the typical signs show. In addition, a woman’s heart attack symptoms are often different than a man’s.
That’s how you can detect a heart attack
Classical signs of heart attack (“heart attack”) are sudden severe pain in the chest, in the front left chest or behind the breastbone. The pain can be oppressive, stinging or burning. They stop according to German Heart Foundation for at least five minutes. Sometimes they also radiate to other regions of the body. Pain in the arm (especially on the left), in the upper abdomen, in the back, in the shoulder or in the jaw can also be a warning signal for a heart attack.
Other typical heart attack symptoms are:
- Tightness or tightness: Affected people often describe this strong feeling of constriction as “an elephant is standing on my chest”.
- Anxiety to death anxiety: The strong fear is often accompanied by cold sweat, a pale complexion and cold skin.
- sudden severe respiratory distress, unconsciousness or severe dizziness: These nonspecific symptoms can have many causes, including a heart attack. More often, they occur in women.
- Nausea and vomiting: These symptoms, which are present in many diseases, are a possible sign of a heart attack, especially in women. This is especially true when those affected have not previously experienced such complaints.
The heart attack symptoms also depend on which coronary vessel is affected. For example, occlusions of the right coronary artery often lead to the so-called posterior wall infarction. They rather cause Complaints in the upper abdomen, If, on the other hand, the left coronary artery is closed, a frontal infarction results. Here are the Pain rather in the chest area localized.
In some cases, a heart attack is painless. Such a “mute infarction” is especially common in patients with diabetes mellitus and in older people.
Divergent heart attack symptoms in women
Not always the symptoms described above in heart attack. Women often have different symptoms. While about the majority of affected men feel the classic chest pain, only about one-third of women experience it. In addition, patients often report one Pressure or tightness in the chest instead of severe chest pain.
Besides, they are much more nonspecific complaints Signs of heart attack in the woman. These include about Shortness of breath, nausea and vomitingsuch as Complaints in the upper abdomen.
Such symptoms are often not immediately identified as heart attack symptoms and taken little seriously. Therefore, women with heart attacks come on average one hour later to the clinic as affected men (calculated from onset of the first heart attack signs). However, fast medical care is vital.
Myocardial Infarction: Harbingers
Many heart attacks occur “out of the blue”. There was previously no evidence that the occlusion of a coronary artery is imminent.
In the other cases, signs herald the heart attack. Many patients suffer from coronary heart disease (CHD) decades before (unnoticed). The coronary arteries are becoming increasingly narrow due to calcification (atherosclerosis). This affects more and more the circulation of the heart muscle. This can be recognized, for example, from physical strain or emotional arousal Chest pain and / or respiratory distress occur. After the end of the stress the symptoms disappear again within minutes.
Doctors are talking about “chest tightness(Angina pectoris), which can develop into a heart attack at any time, especially if the duration and intensity of anginal attacks increases, taking special care with chest pain and / or respiratory distress, even under the least strain even at rest – these are serious harbingers of an impending heart attack. Call the ambulance immediately in such cases!
Heart attack: causes and risk factors
A heart attack is usually caused by a blood clot, the one Cardiovascular blocked, The coronary vessels are those vessels that supply the heart muscle with blood and oxygen. In most cases, the artery in question is already narrowed beforehand by deposits (plaques) on the inner wall. These consist of fats and lime. Such arteriosclerosis (arteriosclerosis) in the area of the coronary arteries is Coronary heart disease (KHK) called.
The plaques can crack and break. Then platelets (platelets) are immediately deposited to seal the cracks. It releases messenger substances that attract more platelets – it forms a blood clot (thrombus). If this clot completely clogs the vessel in question, it leads to a heart attack: The heart muscle section, which is mainly supplied by this coronary artery, does not get enough oxygen. He can then die within a few hours. In the worst case, the patient dies from the heart attack (acute cardiac death).
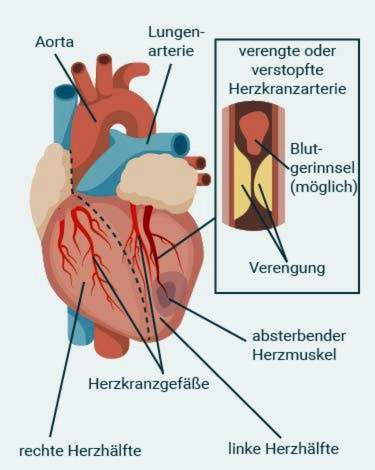
Coronary artery disease is considered the leading cause of myocardial infarction. Only very rarely are other causes of myocardial infarction, for example spasms of the coronary arteries.
Risk factors for heart attack
Although certain factors are not direct causes of myocardial infarction, they increase the risk of infarction. These include, in particular, those risk factors which favor the above-described deposits on the inner wall of the coronary arteries (arteriosclerosis).
Some of these risk factors can not be influenced. These include, for example, older age and male gender. But you can certainly do something about other risk factors, such as overweight and a high-fat diet. In general, the more of the risk factors listed below a person has, the higher is his risk of heart attack.
Male gender: The sex hormones apparently have an impact on the heart attack risk. Because menopausal women have a lower heart attack risk than men; they are then better protected by the female sex hormones, such as estrogens.
Genetic predisposition: In some families, cardiovascular disease is more prevalent – the genes seem to play a role in the development of a heart attack. The risk of an infarction is thus hereditary to a degree.
Higher age: With age, the degree of arteriosclerosis increases. Thus, the risk of myocardial infarction increases.
Nutrition: High-fat and energy-dense foods lead to overweight and high cholesterol levels. Both promote arteriosclerosis and thus coronary heart disease – the most common cause of heart attack.
Overweight: It is generally unhealthy to weigh too many kilos. Even more so, when the excess weight is concentrated on the abdomen (rather than the hips or thighs), belly fat produces hormones and messengers that, among other things, increase the risk of cardiovascular diseases such as coronary heart disease and myocardial infarction.
Lack of exercise: Sufficient exercise has many positive effects on health. One of them: Regular physical activity prevents arteriosclerosis and coronary heart disease by lowering blood pressure and improving cholesterol levels. These protective effects are eliminated in the case of moans of movement.
Smoke: Substances from tobacco smoke promote the formation of unstable plaques that can break easily. In addition, when smoking any cigarette, the blood vessels, including the coronary arteries narrow. Most patients who have a heart attack before the age of 55 are smokers.
High blood pressure: Constantly elevated blood pressure values directly damage the inner walls of the vessel. This favors deposits on the walls (arteriosclerosis) and thus a coronary heart disease.
Elevated cholesterol level: High LDL levels and low HDL levels also promote plaque formation.
Diabetes mellitus: In diabetes, the blood sugar level is increased abnormally. In the long term, this damages the blood vessels – a risk factor for arteriosclerosis and coronary heart disease.
Controversial is whether an increased value of the protein building block (amino acid) homocysteine also represents a heart attack risk factor.
Heart attack: treatment
Heart attack: first aid
That way, you should have a heart attack First aid Afford:
- Call the emergency doctor at the slightest suspicion of a heart attack (Tel. 112)!
- For example, store the patient with a raised upper body by leaning against a wall, for example.
- Open tight clothing, for example collar and tie.
- Calm the patient and ask him to breathe calmly and deeply.
- Do not leave the patient alone!
If the patient becomes unconscious, no respiration is detectable or no pulse is palpable, there is a cardiac arrest. Then you have to act quickly and revive the patient: do that Heart pressure massage or – if practiced – alternate alternating cardiac pressure massage and mouth-to-mouth resuscitation (alternately pressing 30 times and breathing twice). Continue resuscitation until the ambulance arrives or the patient breathes again.
Myocardial Infarction: What Does the Emergency Doctor Do?
The emergency physician or paramedic will immediately control the patient’s most important parameters, such as state of consciousness, pulse and respiration. He also includes the patient ECG or a monitor to monitor heart rate, heart rhythm, oxygen saturation, and blood pressure. The ECG is very important for the accurate diagnosis of a heart attack. It can thus be determined whether it is a so-called heart attack with ST segment elevation (ST elevation myocardial infarction, STEMI) or a heart attack without ST segment elevation (non-ST elevation infarction, NSTEMI). This distinction is important for the choice of immediate therapy (see below).
About a nasogastric tube gets the patient oxygen supplied when the oxygen saturation is too low as well as shortness of breath or acute heart failure.
There is also an access placed over a vein to help the patient quickly drugs to be able to administer. This can be for example Diazepam against the strong fear and morphine against the pain. Also important are active ingredients (such as acetylsalicylic acid), which prevent the blood clot in the coronary vessel from becoming larger or clots forming.
In addition, the emergency doctor gives the patient nitrates, usually in the form of an oral spray. These dilate the blood vessels, reduce the oxygen demand of the heart and reduce the pain. However, the heart attack prognosis does not improve nitrates.
If there is a cardiac arrest during transport to the hospital, the emergency doctor or paramedic will immediately start the cardiac arrest Revival with one defibrillator.
Further heart attack therapy
Further treatment for myocardial infarction depends significantly on whether it is a heart attack with ST segment elevation (STEMI) or a heart attack without ST segment elevation (NSTEMI) (see below: “Myocardial infarction: examinations and diagnosis”):
- STEMI: The treatment of first choice is one in these patients Acute PTCA, This means that the constricted heart vessel is expanded by a balloon (balloon dilatation) and kept open by introducing a stent. If necessary, with STEMI also a thrombolysis (administration of medication that dissolves the blood clot in the heart vessel). Under certain circumstances, a bypass operation may be necessary in the further course.
- NSTEMI: The benefit of immediate balloon dilatation (acute PTCA) is not proven here. Even a lysis therapy is not indicated. Instead, those affected receive immediately after the diagnosis drugs, for example against (further) clot formation (such as acetylsalicylic acid). In addition, one can Cardiac catheterization be useful to determine the extent of damage to the heart muscle. It should be performed within two to 72 hours, depending on the risk profile of the patient. Further therapeutic measures depend on the result of the examination (for example, further drug treatment, balloon dilation and stent installation, bypass surgery).
In the following, the various treatment options for heart attack are described in more detail.
Heart attack therapy: Acute PTCA
At a Heart attack with ST segment elevation (STEMI) Therapy of first choice is a so-called acute PTCA (percutaneous transluminal coronary angioplasty). It instantly introduces a cardiac catheter to dilate the clogged vessel with a balloon. This is called balloon, After that often gets heart attack stent Implanted: This is a small metal stent designed to hold the vessel open. Often, stents coated with an anticoagulant drug are used. It prevents a blood clot from forming again at this point.
Acute PTCA can in most cases reopen the clogged blood vessel after a heart attack. It should be done within 60 to 90 minutes after the onset of pain.
However, such an intervention is not available promptly for all STEMI patients, because not every clinic has cardiac catheterization. Thus, if a heart attack patient can not be hospitalized within 120 minutes, where acute PTCA is possible, he should, within 30 minutes, have one thrombolysis (see below). Within the next three to 24 hours, he should then be transferred to a cardiological center for acute PTCA.
Heart attack therapy: lysis therapy
The lysis therapy (Thrombolysetherapie) comes in patients with a ST elevation myocardial infarction (STEMI) into consideration. In the process, the blood clot that triggered the myocardial infarction is dissolved by medication (lysis). The doctor injects the patient with drugs into a vein, which either directly break down the thrombus or activate the body’s own degradation enzymes (plasminogen), which in turn dissolve the blood clot.
The chance of the coronary vessel opening again is greatest shortly after the heart attack. Sometimes the emergency doctor starts the lysis therapy even before the patient arrives at the hospital.
Lysis can be performed up to a maximum of twelve hours after a heart attack. Thereafter, the blood clot is no longer properly resolved, and the side effects of the treatment outweigh.
Side effects: The lysis drugs given after a heart attack strongly inhibit the body’s own blood clotting – not only in the heart, but in the entire body. As a complication serious bleeding can occur. So far unrecognized bleeding sources such as stomach ulcers or vascular malformations (aneurysms) can be activated, so start to bleed. One of the most serious side effects is a brain hemorrhage.
Heart attack therapy: medication
In a heart attack, the doctor usually prescribes medication for the patient. These must be partially taken permanently. Which active ingredients are prescribed to the patient and how long they have to take depends on the individual risk profile. Common drugs in heart attack patients are:
- Acetylsalicylic acid (ASA): The active substance ASA is a so-called platelet aggregation inhibitor. That is, it prevents platelets from accumulating. In an acute myocardial infarction, this prevents the clot from enlarging in the affected coronary artery (or forming new clots). Already the emergency doctor injects the patient ASA, because an early treatment improves the prognosis.
- other platelet aggregation inhibitors: Some heart attack patients also receive clopidogrel, prasugrel, or other platelet aggregation inhibitors.
- beta blocker: They lower blood pressure, slow down the heartbeat and relieve the heart. If administered early, you can reduce the size of the heart attack and prevent life-threatening cardiac arrhythmias (ventricular fibrillation). Already the emergency physician can administer the patient beta blocker.
- ACE inhibitors: These drugs dilate the blood vessels, lower the blood pressure and relieve the heart. They lower the mortality risk in infarct patients.
- cholesterol-lowering drug: So-called statins reduce elevated levels of “bad” LDL cholesterol. This reduces the risk of another heart attack.
At a Heart attack without ST segment elevation (NSTEMI) It is generally started immediately after the diagnosis with the drug treatment. Patients receive platelet aggregation inhibitors (such as acetylsalicylic acid, prasugrel), anticoagulants (such as fondaparinux), and anti-circulatory drugs (beta-blockers). Sometimes with NSTEMI the drug therapy is sufficient. However, other therapeutic measures may be necessary (such as balloon dilatation or bypass surgery).
Heart attack therapy: bypass surgery
In some heart attack patients, the coronary arteries are so severely altered that a bypass operation is necessary: Under general anesthesia, the surgeon first removes a thoracic artery or a superficial leg vein from the patient. He then uses this to bridge the bottleneck of the coronary vessel.
Myocardial infarction: examinations and diagnosis
The urgent suspicion of a heart attack results from the patient’s complaints. But the signs are not always clear. Therefore, various investigations are needed. They help to hedge the diagnosis heart attack and to exclude other illnesses, which can cause similar symptoms (chest pain etc.). These include, for example, pericarditis (pericarditis), a tear of the large body artery (aortic dissection) or pulmonary embolism.
ECG
Electrocardiography (ECG) is the most important procedure for suspecting a heart attack. In doing so, electrodes are created on the chest of the patient. These record the electrical excitement in the heart muscle. Characteristic changes in cardiac electrical activity indicate the size and location of the infarction. Important for therapy planning is the distinction between a heart attack with and without ST segment elevation:
- Heart attack with ST segment elevation (STEMI): In this form of heart attack, a certain portion of the ECG waveform (the ST segment) is raised in an arc. The infarct affects the entire heart wall (transmural heart attack).
- Heart attack without ST segment elevation (NSTEMI or Non-STEMI): In this inner wall infarction (non-transmural infarction), the ST segment on the ECG is not raised. Sometimes the ECG is completely unremarkable despite typical symptoms of infarction. The diagnosis heart attack can be made here only if certain “heart enzymes” are detectable in the blood (see below: “blood test”).
In addition, ECG can also detect infarcts that cause no symptoms (silent or silent heart attack). Cardiac arrhythmias are also recognizable on the ECG. These are by far the most common complication of a fresh heart attack.
In addition, the ECG helps to differentiate an acute myocardial infarction from a recent myocardial infarction.
Some infarcts do not show up immediately after they have entered the ECG, but only become visible a few hours later. Therefore, in case of suspected myocardial infarction, several ECG examinations are performed several hours apart.
Heart ultrasound (echocardiography)
If the ECG does not show any typical changes, although the symptoms indicate a heart attack, cardiac ultrasound through the chest may help. The technical term for this study is “transthoracic echocardiography”. The doctor can detect disturbances of the wall movement of the heart muscle here. Because if the circulation is interrupted by the infarction, the affected heart section no longer moves normally.
blood test
The cardiomyocytes dying from a heart attack release certain enzymes. In an infarction, therefore, their concentration in the blood is increased. These include proteins called biomarkers Troponin T., Troponin I, myoglobin as well as the Creatine kinase (CK-MB), However, in the classical tests used for this purpose, the concentration of the enzymes in the blood rises measurably at the earliest approximately three hours after the heart attack. Newer, more sophisticated procedures can speed up the diagnosis.
cardiac catheterization
A cardiac catheterization reveals which coronary vessel is closed and whether other vessels are narrowed. The function of myocardium and heart valves can also be assessed using this examination.
As part of the cardiac catheterization, the doctor introduces a narrow, flexible plastic tube into the femoral artery (A. femoralis) and pushes it against the bloodstream to the heart. Mostly in the investigation one coronary angiographyThis means that a contrast agent is injected via the catheter so that the coronary vessels can be visualized in an x-ray.
During the cardiac catheterization, the closed coronary artery can also be reopened immediately: The doctor introduces a small balloon over the catheter. He is filled with liquid at the site of the vessel closure, whereby he expands the bottleneck (balloon or PTCA: see above). After that, the doctor usually places a small metal framework as a vascular support (stent) into the vessel to keep it open.

Myocardial infarction: disease course and prognosis
Decisive for the acute prognosis after an acute myocardial infarction are two possible ones complications – Cardiac arrhythmia (especially ventricular fibrillation) and a pumping failure of the heart muscle (cardiogenic shock). Patients can die from such complications.
The Long-term prognosis After an acute myocardial infarction depends, among other things, on the answers to the following questions:
- Does the patient develop heart failure (see below)?
- Can the risk factors for another heart attack (high blood pressure, high cholesterol etc.) be reduced or eliminated altogether?
- How consistently does the patient maintain a healthy lifestyle? These include, for example, regular exercise, a heart-healthy diet, avoiding smoking, reducing obesity and avoiding stress and tension.
- Is the disease of the coronary vessels (vascular calcification) progressing?
Statistically, five to ten percent of heart attack patients die from sudden cardiac death within two years after discharge from hospital. Particularly at risk are patients over 75 years.
Myocardial Infarction: Aftercare
Very important for the prognosis of a heart attack is the follow-up treatment. Already in the first days after the myocardial infarction the patients start with Physiotherapy and breathing exercises, Physical activity revives the circulation and prevents further vascular occlusions.
Some weeks after a heart attack, patients may be having one Cardiovascular training kick off. But this is far from competitive sports! Recommended sports include hiking, light jogging, cycling and swimming. Patients should discuss with their doctor an individual training program. You can also join one Heart Sports Group connecting: The joint training with other heart patients can make a lot of fun and motivate.
Most heart attack patients spend some time in one after discharge from hospital Rehab Facility, There they learn to change their lives so that the risk of another heart attack decreases.
As mentioned above, risk factors for a (re) cardiac infarction such as high blood pressure, high cholesterol, obesity or diabetes mellitus should be reduced as much as possible. This includes the fact that the patients comply with the prescribed therapy by the doctor, for example, conscientiously taking the antihypertensive medication. In addition, regular check-ups at the doctor are important. So you can recognize any problems early and take countermeasures in time.
Myocardial Infarction: Follow
For many sufferers, a heart attack has consequences that can change your life. These include on the one hand short-term consequences such as Arrhythmia, They can occur in the form of atrial fibrillation or as life-threatening ventricular fibrillation.
Even long-term consequences are possible after a heart attack. For example, some patients get one depression, Also one chronic heart failure(Cardiac insufficiency) may develop: Heart muscle tissue, which has died of infarction, is replaced by scar tissue, which impairs cardiac function.
A rehab treatment and a healthy lifestyle help to prevent such complications and consequences of a heart attack. Read more about it in the article Heart Attack – Follow.
Myocardial Infarction: Prevention
You can prevent a heart attack by reducing the risk factors for atherosclerosis as much as possible. That means:
- Do not smoke: If you do without cigarettes & Co., you can significantly reduce your risk of heart attack. At the same time, the risk of other sequelae such as stroke is reduced.
- Healthy eating: As a heart-healthy diet is about the Mediterranean diet. It consists of lots of fresh fruit and vegetables and low in fat. Here, instead of animal fats (butter, cream, etc.) preferably vegetable fats and oils are used (olive, rapeseed, linseed oil, etc.).
- Reduce obesity: Just a few pounds less have a positive effect on your health. With a healthy body weight can prevent heart attack and other diseases (stroke, etc.).
- Lots of exercise: Be physically active regularly. It is not about high-performance sports: Already a daily half-hour walk is better than no sport and lowers the heart attack risk. Also movement in everyday life (such as climbing stairs, shopping with the bike, etc.) contributes to.
- Treat risk diseases: Basic diseases such as diabetes, high blood pressure or elevated cholesterol levels should be optimally treated. This not only includes the regular use of prescribed medications. With a healthy lifestyle (exercise, healthy nutrition, etc.), each patient can contribute a lot to the success of the therapy itself.
- Avoid stress: Try to avoid prolonged job and personal stress as much as possible. This has been proven to reduce the risk of a heart attack.
Additional information:
Book recommendations:
- Restart: A heart attack may be the end – or the beginning (Oliver Gaw, 2016, adeo)
- Trauma Myocardial Infarction: The Psychological Coping of a Cardiovascular Disease (Mag Alexander Urtz, Dr. Sebastian Globits, 2017)
guidelines:
- Pocket guideline “Treatment of acute heart attacks in patients with ST segment elevation (STEMI)” (Version 2017) of the German Cardiac Society – Cardiovascular Research e.V.
- Pocket guideline “Acute Coronary Syndrome without ST-Elevation (NSTE-ACS)” (Version 2015) of the German Cardiac Society – Cardiovascular Research e.V.
Support Groups:
German Heart Foundation e.V.
www.herzstiftung.de