Vascular dementia develops as a result of circulatory disorders in the brain. It is the second most common form of dementia after Alzheimer’s disease. The two forms of dementia are often confused with each other. There are also mixed forms of both dementias. Find out more about vascular dementia here: Causes, Symptoms, Diagnosis, Therapy and Prognosis!
Vascular dementia: description
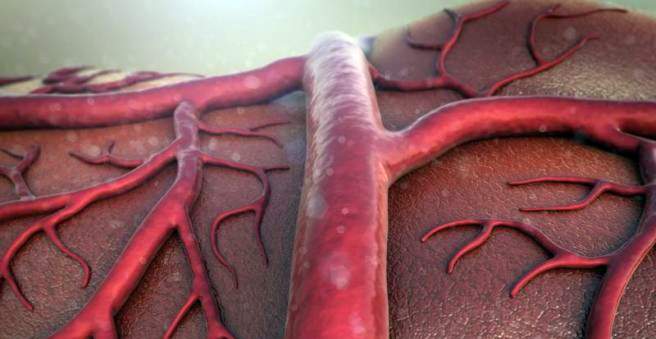
A “vascular dementia” is caused by a disturbed blood supply to the brain tissue. Depending on the mechanism of this circulatory disorder, physicians distinguish different forms of vascular dementia. Thus, for example, there is the multi-infarct dementia, which is caused by several small brain infarcts (strokes). Other forms include subcortical vascular dementia and mixed (cortical and subcortical) vascular dementia.
Vascular dementia accounts for about 10 to 15 percent of all dementias. Another approximately 20 percent is due to mixed forms of vascular and Alzheimer’s dementia.
Vascular dementia: symptoms
People with vascular dementia find it difficult to speak coherently, listen attentively, and get their bearings. They often seem confused. There are also drive and concentration disorders as well as mood swings. The latter can express themselves, for example, by the fact that those affected change very quickly between laughter and crying (often without corresponding emotion).
Vascular dementia is also associated with focal neurological deficits (due to cerebral infarction): hemiplexy, gait disorder and increased muscle reflexes, for example, can occur. Disorders of bladder emptying (micturition disorders) in the form of compulsive (imperative) urinary urgency or incontinence are also possible.
Personality and social behavior are not affected by the vascular dementia. Memory is often only marginally affected by the disease.
Vascular dementia: causes and risk factors
A vascular dementia is caused by a reduced blood flow in the brain (cerebral ischemia), which causes nerve cells to die off. Various mechanisms can trigger such ischemia:
The classic form of vascular dementia is the Multi-infarct dementia: It occurs when multiple concurrent or delayed cerebral infarctions (ischemic strokes) kill a critical mass of nerve tissue.
In other cases, vascular dementia is caused by a single, sometimes even small, infarct at a strategically important site (such as the thalamus) leading to a disruption of pathways. Doctors speak of this “strategic infarct dementia”.
The circulatory disorder can also be caused by a Thickening of the walls of small blood vessels be conditional, provide the deeper brain areas with blood. It comes to small infarcts (lacunae) and damage to nerve fibers (Mark bearing damage). Doctors speak of the subcortical vascular encephalopathy (SVE).
In some patients, vascular dementia is the result of smaller or larger ones Cerebral hemorrhage, Then one speaks of “hemorrhagic dementia“.
There are also other, rarer forms of vascular dementia.
Vascular dementia: risk factors
Various factors favor vascular dementia. These include, for example, high blood pressure, heart disease, diabetes mellitus (diabetes), elevated cholesterol, obesity, lack of exercise and smoking.
Vascular dementia: diagnosis
If vascular dementia (or other type of dementia) is suspected, the doctor will first discuss it with the patient and often with relatives To raise medical history (Anamnese):
He describes the symptoms and asks about current or past illnesses such as cardiovascular diseases, diseases of the cerebral vessels, hypertension, elevated blood lipid levels and diabetes. He also asks about the patient’s nicotine and alcohol consumption. In addition, the doctor asks to what extent the patient is physically active and whether he is taking any medications.
Physical examination
This is followed by the physical examination. If vascular dementia is suspected, the doctor will carefully check the cardiovascular status (blood pressure, heart rate, heart rate, heart size, etc.) and neurological status (tactile and balance, coordination, motor skills, strength, and reflexes).
Neuropsychological examination
Especially important for the diagnosis of vascular dementia is the neuropsychological examination. Various tests are carried out in order to be able to record the brain power disturbance (“dementia tests”). However, these deficits are very mixed in vascular dementia.
imaging
Imaging studies such as computed tomography (CT) and magnetic resonance imaging (MRI) are important to rule out other causes of the symptoms. These can be, for example, brain tumors, cerebral hemorrhages or a “hydrocephalus”. Characteristic tissue changes also indicate which vascular dementia variant is present, for example multi-infarct dementia or dementia as a result of infarction in important brain interfaces (strategic infarction).
An ultrasound examination of the brain supplying blood vessels can show possible constrictions (stenoses) and closures.
laboratory tests
When suspected vascular dementia is also routinely diagnosed blood sample examined by the patient. Parameters such as blood salts (electrolytes), blood sugar and liver enzymes are important in identifying risk factors for vascular damage that can be medically treated. In addition, other dementia causes (such as hypothyroidism or hepatic dysfunction) can be identified by blood tests.
If the findings remain ambiguous, they will also become one Sample of cerebrospinal fluid (CSF) and examined in the laboratory. In this way, for example, inflammatory or immunological diseases of the brain can be ruled out as a reason for the symptoms.
Genetic Testing
Vascular dementia may be associated with a variety of genetic vascular diseases. Some of these can be detected by molecular genetic methods. Such genetic tests should only be carried out on justified suspicion.
Vascular dementia: therapy
The vascular dementia can not be treated causally. With various therapeutic measures but you can try to relieve the symptoms.
drugs
Against the vascular dementia itself, there are no drugs that are approved and their effectiveness is scientifically proven. In individual cases, drugs are given for the psychiatric symptoms. Such preparations have no specific approval for vascular dementia, so they are used here in “off-label use”.
Sometimes in vascular dementia so-called acetylcholinesterase inhibitors and memantine are helpful. These drugs are used as anti-dementia drugs, especially in Alzheimer’s. There is also evidence that a particular extract of ginkgo leaves (Ginkgo biloba EGb761) is effective in vascular dementia.
Appropriate medicines should also treat relevant risk factors for vascular damage and underlying vascular diseases (such as increased blood lipid levels, high blood pressure, etc.). This should be avoided further vascular damage and infarction.
Non-drug treatment
Vascular dementia, like other types of dementia, should be treated non-medically. For example, cognitive training, ergo, music and dance therapy in dementia may be useful. In case of walking insecurity, sufferers should receive walking aids and regular walking training. For continence problems, a consistent toilet training is recommended.
Non-pharmacological measures are also important for vascular risk factors and underlying diseases. For example, the doctor will recommend that the patient refrain from smoking in the future and change the diet (less animal, more vegetable fats, etc.).
Vascular dementia: course and prognosis
The vascular dementia does not take a consistent course – the underlying disease mechanisms can be very different. Most of the symptoms are sudden (vascular dementia after stroke) and often worsen in batches. Some vascular types of dementia are also progressing slowly.
The course of the disease (as well as the symptoms) is also influenced by the fact that there is not always a purely vascular dementia. Patients often suffer from a mixed form, such as Alzheimer’s dementia plus vascular dementia. Life expectancy and course can then hardly be predicted.
In general, the life expectancy of patients is shortened in many cases. Vascular dementiaPatients often die from diseases such as pneumonia, stroke or acute circulatory disorder of the heart (acute coronary syndrome).