In a scoliosis, the spine curves to the side. Mostly, the vertebral bodies are twisted. Symptoms usually develop only with a stronger spinal curvature. Light forms can often be treated with physiotherapy and a special corset, heavy cases need surgery. Read all about causes, diagnosis and therapy for scoliosis here.

Scoliosis: short overview
- Definition: permanent lateral curvature of the spine
- Common symptoms: shoulders of different heights, oblique pelvis, head tilted to the side, lateral “rib hump”, back pain, tension
- Consequences: Stiffening of the respective vertebral section, early wear
- Important investigations: physical examination, Adams test, mobility / strength tests, X-ray, determination of skeletal maturity
- Treatment options: Physiotherapy, corset, plaster, brace technique, surgery
Scoliosis: description
To understand what scoliosis is, you first need to know how a healthy spine is built.
Structure of the spine
A healthy spine consists of about 33 vertebral bones: seven cervical vertebrae, twelve thoracic vertebrae, five lumbar vertebrae, five sacral vertebrae fused together, and about four – likewise fused coccyx vertebrae. Bone processes connect the vertebral bodies with the adjacent vertebrae and ribs.
Seen from the side, the spine has the shape of a double “S”. The cervical and lumbar spine bulge forward (lordosis), the thoracic and sacral vertebral column (sacral) to the rear (kyphosis). Looking at the spinal column from behind, it forms with its spinous processes a nearly straight line from the head to the anal fold. The vertebral bodies lie evenly on each other and between each two of them is an intervertebral disc as a shock absorber.
The spine is an important part of the supporting skeleton and also protects the spinal cord, a bundle of nerve tracts that transmits signals between the body and the brain.

What is scoliosis?
In case of scoliosis the spinal column structure is disturbed. The name of the disease is derived from the Greek word skolios, which means “crooked”: In this case, the spine curves not only forward and backward, but also to the side.
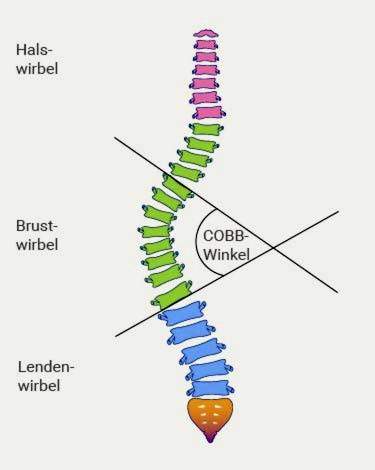
According to the guideline-compliant scoliosis definition, this disease is “a permanent (fixed) lateral spinal curvature of at least ten degrees Cobb angle, This angle indicates how strong the lateral curvature of the spine is and can be determined by means of an X-ray image. Depending on which side of the spine bends, doctors speak of a right or left convex scoliosis.
In addition, the individual vertebrae are twisted in itself and the entire spine in its longitudinal axis (rotation and torsion). This shows the bony vertebral body processes (spinous process, spinous process). The side of the appendages that points to the abdomen or chest thus turns in the direction of the spinal curvature. The rotation is strongest at the apex of the scoliosis and decreases again at the foothills of the curved spine segment.
As the scoliosis progresses, the corresponding vertebral portion may stiffen.
Due to the different degrees of torsion stress and compressive forces arise between the individual vertebrae. As a result, the vertebral bone also has a warped bone structure (torqued): on the convex side, the vertebral body is higher than on the inward facing side. The same applies to the intervertebral discs between the vertebral bones. This results in a permanently existing Schiefwuchs. The twisted and crooked spine also refer to experts as Torsionsskoliose.
Most torsion scoliosis occurs only at the main curvature. In order to compensate for a strong scoliosis, muscular force causes secondary curvatures of the spine in the immediate vicinity of the main curvature (static compensation). However, the minor curvatures have no rotation or torsion. If you do, you call that one Multiple Scoliosis.
Which scoliosis forms are there?
Scoliosis can be divided into different forms, depending on the point of view. So one differentiates generally about the idiopathic scoliosis from one secondary.
- Idiopathic means that no specific trigger for the disease can be found.
- Secondary scoliosis, on the other hand, is always the result of a known cause.
These “genuine” (structural) scolioses are to be distinguished from a scoliotic malposition (also functional scoliosis).
A scoliotic maladjustment is temporary and normalizes again through passive or active movements. It arises, for example, to compensate for a pelvic obliquity.
Since one does not know the cause of scoliosis in many cases, one can not effectively prevent it.
True scolioses can be further differentiated according to age and curvature pattern:
Scoliosis of different age groups
Among other things, scolioses can be differentiated according to the time of their first appearance. The early form becomes infant scoliosis and in most cases forms without therapy. From one infantile scoliosis Doctors talk when the spine curvature occurs by the age of three. Scoliosis in children aged four to ten years is considered juvenile form designated.
The most common, however, is the Adolescents Scoliosis from the age of eleven. The spine is usually bent to the right in the thoracic region (right convex scoliosis). Girls are more often affected than boys.
Scoliosis curve pattern
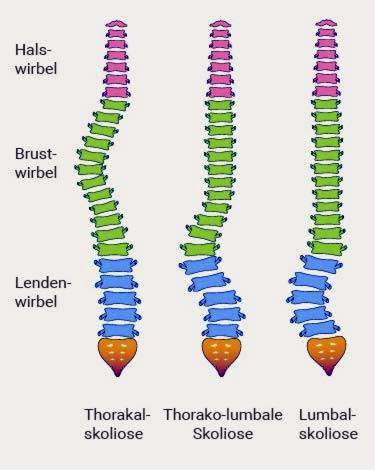
In addition, scoliosis may be assigned to the center (or apex) of its major curvature in the spine. At a Thorakalskoliose the curvature lies in the region of the thoracic spine (thoracic spine). Thoraco-lumbar scolioses have their strongest lateral deflection where the thoracic lumbar spine (LWS) passes. A spinal curvature in the lumbar region is called lumbar scoliosis.
- In some cases sufferers suffer from BWS and at the same time a lumbar scoliosis. It forms a curvature pattern, which – when viewed from behind on the back of the patient – the letter “S” reminds (double-curved).
- If the spine is completely bent to one side, doctors speak of a C-shaped scoliosis.
- Curves of the spine in all sections (thoracic, lumbar and their transition) alternately to the right and left, creates a double-S spine, also called triple scoliosis.
Scoliosis degree of curvature
Also, depending on how strongly the spine is curved, a scoliosis can be divided:
- slight scoliosis: angle up to 40 degrees (1st degree scoliosis)
- moderate scoliosis: angle between 40 and 60 degrees (2nd degree scoliosis)
- severe scoliosis: angle from 61 to 80 degrees (3rd degree scoliosis)
- very severe scoliosis: angle over 80 degrees (scoliosis grade 4)
Scoliosis frequency: The number of times the disease occurs
About two to five percent of the population suffer from idiopathic scoliosis. According to a study by the Maimonides Medical Center (USA), the incidence in old age (60 to 90 years) can increase up to 68 percent.
The greater the spine curvature and the higher the age, the more frequently women or girls are affected. In boys, especially mild scolioses can be found. More pronounced scoliosis, with a Cobb angle greater than twenty degrees, is found about seven times more frequently in women than in men.
Scoliosis: symptoms
Scoliosis is in many cases a purely cosmetic problem. However, the longer it remains untreated, the more likely it is to experience pain during the course of the disease. Because how pronounced the symptoms are always depends on how advanced the curve is.
Among the cosmetic scoliosis symptoms that can be seen with the naked eye include, among others
- different height shoulders
- oblique or on one side excellent basin
- head held awry
In pronounced scoliosis often occurs the so-called rib hump, it can form muscle bulges in the lumbar and neck area.
Due to increasing signs of wear, sufferers have more problems with muscle tension and pain, especially from the middle of the third decade of life. The lung capacity may also decrease and respiratory distress, a feeling of pressure on the chest or palpitations occur.
Read all about the scoliosis symptoms here.
Scoliosis: causes and risk factors
About 90 percent of all scolioses are idiopathic, so you do not know why they arise. The remaining ten percent – the secondary scolioses – have various causes that lead to spinal curvature.
Malformation scoliosis
This form of scoliosis is due to congenital malformations of individual parts of the spine, for example
- wedge-shaped vertebral bodies (different edge heights)
- split or semi-formed vertebral bones
- congenital malformations of the ribs (synostoses)
- Defects in the spinal canal (eg diastomatomyelia)
Experts therefore call them congenital scoliosis.
Myopathic scoliosis
These spinal curvatures are based on muscle diseases (including inheritable muscle weakness diseases). The most common is Duchenne muscular dystrophy, which does not produce any particular muscle protein. As a result, children already suffer from increasing muscle weakness and atrophy at an early age. More than half of those affected develop scoliosis during Duchenne muscular dystrophy, usually in early adolescence and after loss of walking ability.
Arthrogryposis may also lead to severe scoliosis in severe cases. It is a congenital stiffness caused by changes in the tendons, muscles and connective tissue.
Neuropathic scolioses
In this form, damage in the nervous system leads to a crooked spine. Muscles that stabilize the spine (abdominal and back muscles) then no longer work as usual. This creates an imbalance, the spine curving in the direction of the flaccid muscles.
Among other things, these diseases of the nervous system lead to scoliosis:
- Myasthenia gravis (muscle paralysis)
- viral spinal cord inflammation (myelitis)
- Early childhood brain damage (eg, infantile cerebral palsy)
- Neurodegenerative diseases with damage and loss of nerve cells (eg spinal muscular atrophy with decrease of the second nerve tract to the musculature)
- Caving in the Spinal Cord by Cerebral Water Jam (Syringomyelia)
- malignant or benign growths (eg spinal tumors)
Other scoliosis causes
In addition to the aforementioned muscle and nerve diseases, numerous other syndromes can be associated with different degrees of scoliosis. In this case, surrounding connective tissue, but usually also the bone and cartilage structures are directly affected. The table gives some examples.
|
group of diseases |
Scoliosis Causes (Examples) |
|
connective tissue disorders |
|
|
Rheumatic diseases |
|
|
Abnormalities of bone-cartilage structures (osteochondrodysplasias) |
|
|
Bone infections (acute, chronic) |
|
|
Metabolic disorders (metabolic disorders) |
|
|
Lumbosacral changes in the lumbar-sacral area |
|
In addition, accidents can lead to scoliosis. These posttraumatic scolioses occur, for example, after a vertebral fracture, burns or spinal cord injuries. Furthermore, some medical procedures cause a spinal curvature such as radiations or laminectomies, In the latter part of the vertebral bone (vertebral arch possibly with spinous process) is removed.
As with many diseases, experts suspect that scoliosis can also be inherited. 97 percent show a family-frequent occurrence. In identical twins, up to 70% of both cases develop scoliosis. As scoliosis increases with age, researchers assume that ultimately wear and tear have a decisive influence (degenerative changes).
Scoliosis: diagnosis and examination
The specialist for diseases of the musculoskeletal system is the orthopedist. There are also scoliosis pediatricians and pediatric orthopedists. First, the doctor raises the medical history (anamnesis) and asks the patient or his caregiver, among others, the following questions:
- When did the crooked spine first strike you?
- Do you suffer from ailments such as back pain?
- Has it already come to the first menstruation (menarche) or the voice break?
- How fast have you grown in recent years?
- Are other known diseases such as deformities of the feet, a crooked pelvis, muscle or nervous diseases?
- Are there already known cases of scoliosis in your family?
The US Scoliosis Research Society regularly publishes questionnaires for patients suffering from scoliosis (current version SRS-30). In German translation, the questionnaire is also used by doctors in Germany.
Tip: sufferers should complete the questionnaire at regular intervals. By doing so, they can indicate how they feel about the disease and assess the success of treatments.
Physical examination
After questioning, your doctor will physically examine you. First, he determines the standing and sitting size, then he examines the back and especially the shape of the spine. If the line of spinous processes deviates, it detects a so-called overhang. The thorax is laterally displaced. As a result, a straight line from the last cervical vertebra downwards no longer ends in the anal fold during scoliosis, but next to it.
He also checks the lateral alignment of the shoulder blades (symmetrical shoulder stand) and the waist and the outline of the trunk. In a scoliosis, the shoulders are different levels. The two so-called waist triangles are of different sizes, so the distances from the left or right drooping arm to the trunk.
In the course of the physical examination, the doctor also looks at the statue from the side. As a result, he or she can detect excessive humping (hyperkyphosis) or spinal column (hyperlordosis, eg hollow back), which is strongly curved towards the abdomen.
In rare, severe cases, a pronounced thoracic vertebra is formed. The thoracic spine is then not only to the side, but also strongly curved backwards (kyphoscoliosis).
Such kyphoscoliosis usually occurs with other diseases, such as rickets, bone marrow inflammation or tuberculosis of the vertebral bodies.
In addition, in the context of scoliosis, a crooked pelvis or legs of different lengths can be noticed (leg length difference).
The back skin will also be examined by the doctor, as already here diseases of the spinal cord can show. On the other hand, light brown and even spots on the skin, so-called café au lait spots, are typical of the hereditary disease neurofibromatosis type 1 (Recklinghausen’s disease), which mainly affects the skin and the nervous system. Again, sufferers may suffer from scoliosis, especially kyphoscoliosis.
Physical examination in the infant
Scolioses in infants become visible through various retention tests. For example, if the child lies with his stomach on the examiner’s hand, he can easily recognize a crooked spine because the curvature is usually clearly visible on the back. In the Since Vojta-tilt reaction you can find differences in arm and leg development. For this, the doctor holds the child sideways and pays attention to the body tension of the infant. Held on the side facing away from the curvature of the body usually falls much flaccid from, as on the side, after which the curvature is directed.
A scoliosis is also at the vertical hanging action according to Peiper and Isbert clearly visible. Held upside down by the feet, the entire infant body shows a C-shaped curve to one side.
Adams test
In this examination, the doctor asks you to bend forward with your knees straight. If he now looks at her back, he may recognize typical signs of scoliosis, for example, a rib hump on the back with bent posture or Muskelwülste neck and lumbar area.
In general, the doctor measures the severity of the rib hump or the Muskelwulste by means of a so-called Skoliometers or inclinometer, He compares the heights of the left and the right side with each other. Deviations of more than five degrees are considered pathological according to the guidelines. In these cases further examinations follow, in particular X-rays of the spine.
Examination of mobility, strength, elasticity and reflexes
As part of the physical examination, the doctor will ask you to lean back and forth as well as to the side. By doing so, he checks the mobility of the spine. He also measures the finger-to-floor distance in maximum forward bent position with outstretched legs. Ideally, you can touch the ground (0 cm), but this is rarely possible with pronounced scoliosis. In addition, the doctor will check whether the spinal curvature can be actively compensated by your own movements or by the manual assistance of the physician (passive, manual redressibility). “Real”, structural scoliosis can hardly be changed at all.
It is also important to detect any abnormalities in the nervous system, which can cause scoliosis or can be caused by a spinal curvature or hereditary connective tissue disorders (Marfan syndrome).
roentgen
In many cases, the doctor can diagnose scoliosis based solely on physical examination. However, if suspected spinal curvature, he will always initiate an X-ray. The whole spine is shown standing, once viewed from the front (or back), once from the side.
With the help of the X-ray images, the physician can measure the Cobb angle (in the case of infant scoliosis rather the RVAD rib exit angle), determine major and minor curvatures, make the vertex and end vertebrae and determine the curvature pattern. This procedure is important for later scoliosis therapy. In addition, malformations or deformations of the bones can be detected.

Determination of skeletal maturity
In order to assess the course of scoliosis in adolescents, it is important to determine the state of spinal cord growth. Skeletal maturity is assessed on the basis of the ossification of the iliac crests (apophyses). These processes ossify more and more as they grow older, when they are completely ossified and the apophyses are closed, skeletal growth is complete. The bone age can also be determined by means of an X-ray of the wrist and classified according to Greulich and Pyle.
Although the age usually depends on the skeletal maturity, but it may also differ. For the prognosis of scoliosis the bone age is more reliable than the age.
X Alternatives
In addition to a conventional X-ray diagnosis, there are also a number of imaging procedures without radiation exposure for the investigation of scoliosis. Alternatives include, for example, the Optimetric method, moiré photogrammetry, the video-raster-steriometry-formetric system or the 3D-spine analysis “ZEBRIS”. However, scoliosis can only be assessed to a limited extent using these methods, especially in comparison with X-rays.
Further investigations
In exceptional cases, the doctor can make cross-sectional images using a magnetic resonance imaging (MRI), especially if malformations of the spinal cord or changes in the spinal canal (eg tumors) are suspected.
In severe scoliosis, heart and lung function can be disturbed by the curvature and twisting of the entire chest. In these cases, further tests are initiated. These include, for example, ultrasound examinations of the heart and a lung function test (spirometry).
Depending on the extent of scoliosis, the physician will periodically repeat various tests to monitor the disease process of spinal curvature. In the control X-ray examinations, doctors are usually limited to a frontal image.
Scoliosis: treatment
Scoliosis is conservatively treated with physiotherapy or corset and in severe cases surgically. Scoliosis therapy should begin as soon as possible after diagnosis. The choice of treatment depends on the extent, cause and location of the spinal curvature, as well as the age and physical condition of the patient. Physiotherapy is often sufficient for mild scoliosis; doctors with a scoliosis corset are treated more severely. If there is a very high curvature, surgery can help.
Objectives of scoliosis therapy
With the treatment of spinal curvature, doctors, along with other professionals such as physiotherapists, are trying to reverse or at least not worsen scoliosis. If scoliosis therapy has reduced the curvature, further treatment steps will ensure that this success is achieved. For children and adolescents, the guidelines set a clear goal: the Cobb angle should be below 40 degrees when the growth is completed. If this succeeds, according to the experts, surgical scoliosis therapy is no longer necessary.
Scoliosis corset
A scoliosis corset is used for stronger spinal curvatures of the child (Cobb angle 20-50 degrees). Often one achieves thereby very good results with scoliosis, which are not based on severe basic illnesses (malformations, muscle or nervous illnesses among other things).
The corset (orthosis) is made of plastic and has both incorporated pressure pads (pads) and open spaces (expansion zones).
It is custom-made, attached to the body with straps and Velcro straps and is designed to return the spine to its natural state. The orthosis should be worn 22-23 hours daily. Depending on the height of the main curves, different scoliosis corsets are available.
Depending on the course, girls can gradually reduce the daily wear duration approximately two to three years after the first menstrual period. In boys, it should first be reached a certain skeletal maturity (Risser stage four or five), so that a large growth of the spine is no longer expected.
Adults benefit little from this scoliosis therapy because their bone growth is already complete. Nevertheless, the orthoses are also used in later life, for example, to stabilize and thus mitigate the disease.
Regular exercises also support successful scoliosis therapy with orthoses.
gypsum treatment
In some cases of early spinal curvature (less than five years old, early onset scoliosis) scoliosis therapy using plaster corset may be considered. Here, the spine can continue to grow normally. Gypsum treatment is usually followed by therapy with a scoliosis corset.
Operative scoliosis therapy
In some cases conservative scoliosis therapy (physiotherapy, corset) is not sufficient. If scoliosis deteriorates rapidly and if the curvature is pronounced, doctors generally recommend operative scoliosis therapy. They take into account several factors:
- the curvature severity (from a Cobb angle of about 40 lumbar and 50 degrees thoracic)
- a rapid progression and imminent wear
- the age (if possible, not before the tenth to twelfth year of life)
- general physical condition (mental stress, chronic pain)
With the surgical scoliosis therapy, inter alia, a stiffening spondylosis be prevented. In a spondylosis, the body builds bone substance to the vertebral edges so as to be able to compensate for increased stress. These bony paws of adjacent vertebrae can grow together but the resulting bone bridge stiffens the spine. Possible effects on the cardiovascular system and lung function are also tried with surgery.
During the actual surgical procedure, the surgeon exposes the affected spinal column section. The operation is performed either from the front, via the thoracic or abdominal cavity, or from behind. All surgical scoliosis therapies have in common that the crooked spine should be stretched and its rotation eliminated. In addition, the doctor stabilizes the spine, for example by means of screws and rods.
Scoliosis surgery: stiffening therapy
With the so-called Spinal fusion (Spinal fusion) intentionally causes the merging of vertebrae at the affected site. So you want to stiffen the spine in its previously corrected form.
Newer operative scoliosis therapies for children and adolescents
A stiffening of the spine prevents their natural growth. Therefore it is not an option for children and adolescents. Instead, doctors use special titanium rods in these cases, for example.
The so-called VEPTRs (vertically expandable prosthetic titanium rib) are used in this way – for example, from the rib to the vertebra – so that they do not prevent the spine from growing.
In this scoliosis therapy, doctors need to periodically adjust the bars to growth through further minor procedures, approximately every four to six months.
Modern variants of such bars, the “growing rods“(= Growing bars), include a small remote controlled motor. In this way, they can be adjusted from the outside and without renewed intervention to the respective spinal column growth.
A complex system of screws, rods and a special plate called Shilla method also promises scoliosis therapy without impeding growth. The rods used “grow along with” as they can slide in their mounting screws. Once bone growth is complete, the system can be removed.
correction system
Another method is the correction system ApiFix. It is attached vertically in the arc of curvature of the scoliosis. Physiotherapeutic treatments follow in the months following implantation.
The correction system can react to this by means of a ratchet mechanism: If the spine extends through an exercise, the system is dragged along and locks in place. As a result, the spine can not fall back into its crooked starting position. This scoliosis therapy takes place gradually, so that the surrounding tissue can adapt better.
clip art
This form of operative scoliosis therapy is suitable for bending angles below 35 degrees. Doctors attach special, claw-shaped brackets (Shape-Memory-Alloy, SMA) to the curvature side of the spine. After the procedure, they are cooled, and after the procedure, they visibly push through the body heat of the patient to their original shape, correcting scoliosis.
rehabilitation
Depending on the surgical scoliosis therapy, further treatments follow, for example:
- Scoliosis corset, which can be discarded as soon as the operated parts of the spine are ossified
- controlled physiotherapeutic applications and physiotherapy exercises
The rehabilitation can be done on an outpatient or inpatient basis. Those affected should in any case learn new movements as early as possible. With such rehabilitation measures, one can meaningfully support operative scoliosis therapy and prevent later damage.
Scoliosis: treatment of underlying diseases
If scoliosis is the result of another illness, it will always be treated. This is especially true for diseases or malformations that would promote the progression of spinal curvature. For example, if a patient has different lengths of legs, they try to balance that difference with special shoes.
pain Management
Scoliosis pain in the back, neck, or shoulders, as well as headaches, are usually treated with analgesics in tablet form. Sometimes plaster helps to give off heat. Locally anesthetizing syringes in the back are used only in severe pain. They arise in the context of a scoliosis, for example, by wear damage to the spine and constricted spinal nerves.
Sometimes the so-called “pain” helps with scoliosis Transcutaneous Electrical Nerve Stimulation (TENS), In doing so, electrodes are applied to the skin over the painful area. Diese Elektroden setzten elektrische Impulse frei, die auf tiefer liegende Nerven wirken. Sie hemmen somit die Schmerzübertragung dieser Nerven an das Gehirn. Das Deutsche Skoliose Netzwerk führt zudem die Akupunktur als Teil einer umfassenden Skoliosetherapie an – auch sie soll bei manchen Patienten die Schmerzen lindern.
Skoliose: Übungen
Bei leichten Wirbelsäulenverkrümmungen eignen sich krankengymnastische Übungen als Skoliosetherapie. Sie sollen die Körperhaltung korrigieren. Neben physiotherapeutischen Anwendungen gibt es auch Übungen bei Skoliose, die der Patient zuhause durchführen kann. Übungen als Teil der Skoliosetherapie sollen
- die Körperhaltung verbessern
- die Muskulatur kräftigen
- Krümmungen nach vorn und hinten beseitigen
- die Lungen- und Herzfunktion steigern
Mittlerweile gibt es sehr viele Methoden, um Skoliose mittels Übungen zu therapieren.
Lesen Sie hier alles Wichtige über Skoliose-Übungen.
Skoliose: Krankheitsverlauf und Prognose
Der Verlauf einer Skoliose ist sehr unterschiedlich. Prinzipiell gilt: Je früher eine Wirbelsäulenverkrümmung festgestellt wird, desto wahrscheinlicher schreitet sie voran.
Eine Ausnahme stellt die Säuglingsskoliose dar. Innerhalb der ersten beiden Lebensjahre bildet sich eine schiefe Wirbelsäule in bis zu 96 Prozent der Fälle selbstständig zurück. Außerdem kann sie durch geeignete Lagerungsmaßnahmen und Physiotherapie positiv beeinflusst werden.
Verbleibt eine Restskoliose von über 20 Grad, müssen die Eltern des betroffenen Babys mit einem Fortschreiten der Skoliose rechnen.
Risiko einer Verschlechterung der Skoliose
Tritt eine Skoliose erst in den folgenden Lebensjahren auf, ist die Prognose von verschiedenen Kriterien abhängig. Beispielweise können Grunderkrankungen am Muskel- oder Nervensystem den Krankheitsverlauf verschlechtern. Bei idiopathischen Skoliosen sind neben dem Alter (mögliches Restwachstum) weitere Faktoren von Bedeutung:
- Ausgangs-Cobb-Winkel
- Risser-Stadium (Skelettreife)
- Zeitpunkt der ersten Regelblutung (Menarche, nachgewiesener Zusammenhang mit schubhaftem Knochenwachstum in den darauffolgenden Jahren)
Der Cobb-Winkel hat zu Beginn der Diagnose den größten Stellenwert. Die Leitlinien geben die Wahrscheinlichkeit, dass eine idiopathische Skoliose zunimmt, abhängig vom Krümmungsgrad und dem Alter, wie folgt an:
|
Cobb-Winkel in Grad |
10-12 Jahre |
13-15 Jahre |
16 Jahre |
|
kleiner 20 |
25 Prozent |
10 Prozent |
0 Prozent |
|
20-29 |
60 Prozent |
40 Prozent |
10 Prozent |
|
30-59 |
90 Prozent |
70 Prozent |
30 Prozent |
|
größer 60 |
100 Prozent |
90 Prozent |
70 Prozent |
Krankheitsverlauf im höheren Alter
Skoliosen können sich auch noch im Erwachsenenalter verschlechtern. Dies gilt insbesondere dann, wenn der Cobb-Winkel bei Wachstumsabschluss über 50 Grad liegt. Dabei haben Berechnungen zu thorakalen und lumbalen Skoliosen gezeigt, dass die Krümmung um etwa 0,5 bis ein Grad jährlich zunimmt.
Bei starken Skoliosen, vor allem im unteren Rücken, steigt das Risiko schmerzhafter Beschwerden. Besonders ausgeprägte Verkrümmungen können auch Rückenmarksnerven (Spinalnerven) reizen und Missempfindungen oder Schmerzen hervorrufen.
Achtung: Erreicht die Skoliose einen Wert von etwa 80 Grad, kann sie die Lebenserwartung verringern.
Bei sehr ausgeprägten Verläufen fällt das Atmen durch die zunehmende Verformung immer schwerer. Der Brustkorb ist kaum noch beweglich (Thoraxstarre) und das Lungenvolumen sinkt. Auf der Seite der Krümmung wird die Lunge überbläht (Lungenemphysem). Die andere Lungenhälfte wiederum wird kaum noch belüftet und das Lungengewebe fällt stellenweise zusammen (Atelektase).
Es drohen schwere Komplikationen wie eine Lungenentzündung, eine chronische Bronchitis oder eine Lungenfellentzündung (Pleuritis). Darüber hinaus wird auch das Herz immer stärker belastet (Cor pulmonale).
Komplikationen nach Skoliose-Operationen
Wie jeder chirurgische Eingriff birgt auch eine Operation an der Wirbelsäule gewissen Risiken wie Blutungen, Infektionen (insbesondere bei Akne-Patienten) oder Wundheilungsstörungen. Empfindungsstörungen oder Lähmungen treten bei idiopathischen Skoliosen in der Regel nicht auf. Durch eine operative Skoliosetherapie kann es aber zu Nerven- oder Rückenmarksverletzungen kommen.
Die Wahrscheinlichkeit einer derartigen Komplikation ist allerdings sehr gering. Studien zufolge liegt sie bei 0,3 bis 2,5 Prozent. Das Risiko steigt, wenn ein großer Eingriff durchgeführt wird und weitere Erkrankungen (v. a. des Rückenmarks) bestehen. In manchen Fällen – beispielweise bei Rückenmarkserkrankungen – lassen die Ärzte den Betroffenen während der OP aufwachen und überprüfen dessen Bewegungen und Empfindungen an der Haut.
Ergüsse und Pneu
Wurde durch die Brusthöhle operiert kann es außerdem zu Flüssigkeitsansammlungen im Brustkorb kommen. Diese werden durch einen Schlauch (Drainage) aus dem Körper geleitet. Unter Umständen fällt ein Lungenflügel zusammen, medizinisch Pneumothorax (kurz: Pneu). Auch hier wird ein spezielles Drainage-System verwendet, damit sich die Lunge wieder entfalten kann.
Korrekturverlust
Nach manchen Versteifungsoperationen kann sich zudem die Gegenkrümmung einer Skoliose verstärken. Darüber hinaus geht die erreichte Korrektur in den ersten Jahren nach dem Eingriff manchmal teilweise verloren. In der Regel stabilisiert sich eine Skoliose aber nach der Operation.
Bei jungen Patienten, die schon im frühesten Knochenalter (Risser 0) versteift werden, kann sich ein Korrekturverlust problematisch gestalten. Da die Wirbelkörper weiterwachsen, verstärkt sich in vielen Fällen die Wirbelsäulenverdrehung. Mediziner sprechen vom sogenannten Kurbelwellenphänomen, Um das zu verhindern, erfolgt die versteifende Skoliosetherapie für gewöhnlich sowohl von vorne als auch von hinten.
Zu weiteren speziellen Komplikationen zählen Metallbrüche der bei einer OP eingesetzten Stäbe und Schrauben. In diesen Fällen kommt es fast immer zu einem Korrekturverlust. Bei manchen Versteifungsoperationen verwachsen die Wirbelkörper nicht wie geplant. Es bilden sich „falsche“ Gelenke, sogenannte Pseudarthrosen. Sie können anhaltende Schmerzen verursachen (insbesondere bei Lumbalskoliosen).
Bei manchen Patienten entwickelt sich durch eine aufrichtende Operation mittels Stäben (Harrington-Stäbe) ein Flachrücken. Dabei ist die natürlich bestehende Vorwärtskrümmung der Lendenwirbelsäule aufgehoben. Infolgedessen verschleißen die angrenzenden Wirbel und Bandscheiben schneller und verursachen schmerzhafte Beschwerden.
Skoliose und Schwangerschaft
Entgegen vieler Befürchtungen wirkt sich eine Skoliose nicht negativ auf eine Schwangerschaft aus. Dabei spielt es keine Rolle, ob die Patientinnen konservativ (Krankengymnastik, Korsett) oder operativ behandelt wurden. Wie bei allen Schwangeren kann es auch bei Skoliose-Betroffenen zu tieferliegenden Rückenschmerzen kommen, eine Zunahme des Cobb-Winkels konnte man bislang aber nicht nachweisen.
Kontrolluntersuchungen
Je nach Ausmaß der Skoliose kontrolliert der Arzt den Krümmungsverlauf regelmäßig. Kindliche Rückgratverkrümmungen unter 20 Grad werden ungefähr alle drei bis sechs Monate durch körperliche Untersuchungen überprüft. Hat der Arzt den Verdacht einer Krümmungszunahme, wird er ein Röntgenbild veranlassen. Skoliosen über 20 Grad werden mindestens einmal jährlich mittels Röntgenuntersuchung kontrolliert. Auch im Rahmen einer Skoliosetherapie erfolgen mindestens halbjährlich klinische Untersuchungen.
Ist das Wachstum abgeschlossen und der Cobb-Winkel kleiner als 20 Grad, bedarf es keiner weiteren Kontrolle. Bei einer Skoliose von 20 bis 40 Grad, die nicht operiert wurde, führt der Arzt etwa zwei bis vier Jahre nach Wachstumsabschluss eine Kontrolluntersuchung durch. Hat die Krümmung um fünf Grad zugenommen, folgen weitere Kontrollen. Leiden Erwachsene unter einer über 40-gradigen Skoliose empfehlen die Leitlinien eine jährliche Überprüfung.
Wurde der Betroffene operiert, sind zwei Jahre nach dem Eingriff bei stabiler Versteifung und einem Cobb-Winkel unter 40 Grad keine weiteren Routineuntersuchungen notwendig.
Leben mit Skoliose
In den meisten Fällen können Patienten gut mit ihrer Skoliose leben. Wichtig ist, aktiv gegen die Wirbelsäulendeformität zu arbeiten. Integrieren Sie Skoliose-Übungen in Ihren Alltag. Treiben Sie (Schul)Sport. Haben Sie bei manchen Aktivitäten Bedenken, sollten Sie auf jeden Fall Ihren Arzt befragen.
Belastet Sie Ihre Skoliose im alltäglichen Leben, beispielweise im Beruf oder in Ihrer Freizeit, zögern Sie nicht um Hilfe zu bitten. Wenden Sie sich an Ihren Arbeitgeber, Ihren Physiotherapeuten oder an Freunde. Manche Betroffene engagieren sich auch in Selbsthilfegruppen. Lastet die Skoliose auf Ihrer Psyche oder der Ihres Kindes, kann auch eine psychotherapeutische Behandlung sinnvoll sein. Durch ein offenes und aktives Verhalten können Sie so wertvolle Tipps sammeln und dem Fortschreiten Ihrer Skoliose prevent.
Additional information:
guidelines:
- Leitlinien zum speziellen Rehabilitationskonzept bei Wirbelsäulendeformitäten der Sektion Rehabilitation und Physikalische Medizin der DGOOC von Orthopäden für Orthopäden (Stand: 2012)
- Leitlinien zur idiopathischen Skoliose im Wachstumsalter (Stand: 2009, in Überarbeitung)