The term nephritis (nephritis) includes a number of inflammatory diseases of the kidneys. Depending on the inflamed tissue, there are various forms of nephritis (such as glomerulonephritis). After the course of acute and chronic nephritis can be distinguished. Read more about the individual forms of illness as well as the causes, symptoms, diagnosis, treatment and prognosis of a kidney inflammation!

Quick Overview
- What is a kidney infection? An acute or chronic inflammatory disease of the kidneys that can occur in various forms.
- To shape: Inflammation of the renal corpuscles (glomerulonephritis), inflammation of the urinary canals and the surrounding connective tissue (interstitial nephritis), inflammation of the renal pelvis (pyelonephritis)
- Causes: The onset of glomerulonitis usually involves the immune system. Interstitial nephritis is usually caused by medication or drug abuse. Both forms can also be triggered by other underlying diseases. Kidney pelvic inflammation is usually the result of a bacterial infection.
- symptoms: often symptomless for a long time, nonspecific symptoms in interstitial nephritis (fever, joint pain, etc.)
- Diagnosis: Doctor-patient interview (anamnesis), physical examination, blood and urine examinations, possibly imaging procedures and taking a tissue sample
- Treatment: Elimination or treatment of the cause, e.g. Discontinuation of triggering medications, therapy of underlying diseases, immune system suppressive drugs (immunosuppressive agents such as cortisone) in immune-mediated nephritis. In addition, often general measures such as physical protection and low-protein diet. Diuretic medicines (in the case of water retention in the tissue) and / or hypotensives (in the case of high blood pressure). In case of kidney failure possibly blood washing (dialysis) or kidney transplantation.
- Forecast: If the kidney infection is detected and treated early, the prognosis is usually good. Otherwise, severe events with permanent kidney damage or even kidney failure (renal insufficiency) may occur.
Renal inflammation: description
Renal inflammation (nephritis) can affect the function of the kidneys more or less strongly: The paired organs are involved in numerous vital body functions. They purify the blood of metabolism by-products, regulate water and electrolyte balance, help regulate blood pressure and produce various hormones such as erythropoietin (important for red blood cell formation). Correspondingly serious consequences can occur if the kidneys are limited or not working due to inflammation (or any other illness or damage). In some cases even mortal danger exists.
Renal inflammation: forms
Physicians differentiate depending on the type of inflamed tissue Renal cell inflammation (glomerulonephritis) and the Interstitial nephritis, In addition, there are still the Pyelonephritis.
glomerulonephritis
In glomerulonephritis, the so-called renal corpuscles (Malpighi bodies) are inflamed. These consist of a capsule and a vessel ball, the so-called glomerulus. From the latter derives the name of this form of nephritis.
The job of the kidney bodies is to filter waste products from the blood. In a glomerulonephritis – the typically both kidneys affects – this filter function is impaired.
Glomerulonephritis is immune mediated, That is, the immune system is involved in their formation. This can happen in different ways: Often, antibodies that have formed in the course of an infection or complexes of antibodies and antigens (such as bacterial components) are deposited on the renal bodies. This triggers an inflammatory reaction. Rarely does the immune system produce specific antibodies against kidney structures (autoantibodies). The attack of these autoantibodies against the kidney tissue causes the inflammation.
Depending on the cause, doctors distinguish two forms of glomerulonephritis:
Primary glomerulonephritis
A primary glomerulonephritis is when the inflammation of the kidneys or the kidney corpuscles is not due to an existing underlying disease. An example of this is the so-called IgA nephropathy, also called Berger’s disease.
Secondary glomerulonephritis
The renal corpuscles are ignited due to a disease outside the kidney, is of one secondary glomerulonephritis the speech. Causes are for example:
- certain connective tissue diseases (autoimmune diseases) such as systemic lupus erythematosus (SLE)
- HIV
- an inflammation of the heart’s lining caused by certain bacteria (streptococci) (endocarditis lenta)
- Liver inflammation (hepatitis)
- cancers
- drugs
- genetic defects
Interstitial nephritis
In the interstitial nephritis the so-called interstitium is inflamed. This refers to the intermediate tissue (especially connective and supporting tissue) of the kidneys, which encloses the renal corpuscles and the connected system of the finest urinary tubules (tubule system). If the urinary canals (renal tubules, tubules) are also affected, there is one tubulointerstitial nephritis in front.
Interstitial nephritis: causes
An acute interstitial nephritis usually arises as allergic reaction to medication, Sometimes poisonous effects of certain chemical substances behind it. In both cases one speaks of an abacterial interstitial nephritis (abacterial = not caused by bacteria). Less common are infections with Bacteria or viruses or genetic causes (eg, Balkan nephritis) is the trigger of this form of nephritis.
For example, chronic interstitial nephritis can last for years Prescription drug abuse arise.
Tubulointerstitial nephritis: causes
Depending on the cause, tubulointerstitial nephritis can be divided into a primary and a secondary form. The primary tubulointerstitial nephritis arises as a direct result of infections or Reactions to medication, Secondary tubulointerstitial nephritis develops as a result of other diseases such as renal cell inflammation (glomerulonephritis), which spread to the interstitial tissue of the kidney.
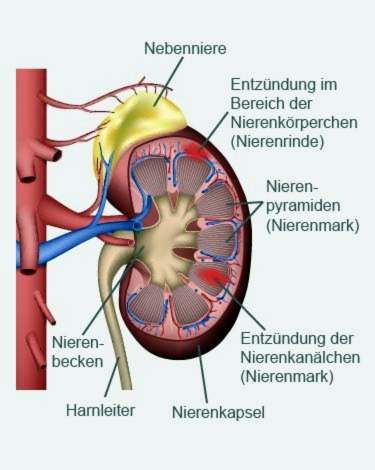
Pyelonephritis
The renal pelvis is the funnel-shaped cavity inside the kidney, where the urine coming from the renal tubules collects before entering the ureter. Inflammation of the renal pelvis (pyelonephritis) can occur when bacterial pathogens ascend via the ureters into the renal pelvis. This form of kidney inflammation is one of the upper urinary tract infections and is one of the most common diseases of the kidney.
Since women have a shorter urethra than men, they are two to three times more likely to be affected by a pyelonephritis. An acute pyelonephritis usually occurs suddenly. It is accompanied by severe flank pain, chills, fever and general malaise.
The chronic form often runs in bursts or creeping. Those affected are tired and ineffective and often have no appetite. Left untreated, chronic pyelonephritis can damage the kidneys to failure.
Read more about risk factors, symptoms, treatment and prevention of pyelonephritis in the article Kidney pancreas.
Renal inflammation: symptoms
Whether symptoms of kidney inflammation appear and how exactly they look depends on the type of disease, its causes and the course of the disease. In some cases sufferers show no symptoms for a long time. The kidney inflammation and resulting kidney damage then remain untreated for too long.
The often long asymptomatic phase is due to the fact that in many patients, the remaining healthy kidney tissue can compensate for the damage over a long period of time.
Glomerulonephritis: symptoms
In contrast to pyelitis, inflammation of the renal corpuscles (glomerulonephritis) usually without pain, Doctors often discover the disease only by chance during routine examinations. In rare cases, the disease only occurs when the kidneys are already severely damaged and a blood wash (dialysis) or transplantation is inevitable. The doctor can recognize this form of nephritis by the following factors:
- It can be Blood and proteins in the urine evidence (hematuria, proteinuria). Both come from the damaged kidney bodies. A very high-protein urine is often cloudy and frothy. Bloody urine has a reddish or brownish color (gross hematuria). Sometimes, however, the amounts of blood in the urine are so small that they are invisible to the naked eye (microhematuria).
- By the disturbed urine production remain more salts (electrolytes) and more fluid in the body, Thus, the inflammation of the kidney can cause symptoms such as water retention in the tissue (edema) (especially in the face and eyelids). High blood pressure (hypertension) is one of the possible signs. Renal inflammation and blood pressure changes are often related through multiple mechanisms, as the kidney can also regulate blood pressure via hormones.
- If more proteins are excreted in the urine, the protein concentration in the blood decreases with time. Parallel the blood lipid levels rise (Hyperlipoproteinemia). Together with the water retention doctors speak of the nephrotic syndrome, For a doctor, a combination of these symptoms is a clear indication of nephritis.
Renal inflammation can lead to acute deterioration of kidney function (acute renal failure). In some of the affected patients, however, the kidney loses its function slowly and over several years to a function of dialysis-dependent chronic renal failure.
Interstitial nephritis: symptoms
The symptoms of this form of nephritis can be different. Sometimes there are no symptoms (asymptomatic course). In other cases it happens:
- fever
- joint pain
- skin rash
- nodular changes under the skin (nodular, erythema nodosum)
- bloody or protein-rich urine
Sometimes, interstitial nephritis causes acute renal failure immediately after taking certain medications.
Chronic courses are also possible, for example when people are taking high-dose painkillers for a long time (Analgesic).
In the long term, people with interstitial nephritis will experience symptoms like one yellow-brownish skin color, a headache and a total dried out appearance on. One chronic kidney failure can be the result.
Renal inflammation: diagnosis
Although it is often difficult to identify and classify the symptoms of inflammation of the kidneys, a doctor can use some examinations to quickly determine if the kidneys are okay or not.
First of all, the doctor talks to the patient To raise medical history (Anamnesis): He asks about the symptoms, possible pre- or underlying diseases and after the application of medication. This information helps the doctor to narrow down the possible causes of the symptoms and to assess the course of the disease.
This is followed by a thorough physical examination, Among other things, the doctor palpates and taps the kidneys. He also checks whether the lateral abdominal regions (flanks) and the area between the last rib and the spine hurt. The skin is also examined, as a kidney infection is often accompanied by rash. In addition, the doctor measures the blood pressure and looks to see if the patient fluid accumulation in the tissue (edema).
To further diagnosis of nephritis are Blood and urine tests important. In the blood test, especially the creatinine value of importance: If it is increased, this indicates a limited kidney function. The urine is mainly tested for protein and – in glomerulonephritis – for blood (proteinuria, hematuria).
Also Imaging procedures like ultrasound can be used to clarify a nephritis. They help to estimate the condition of the kidneys. Sometimes the doctor also takes one tissue sample (Biopsy) from the kidney, to find out the cause of the disease.
Renal inflammation: treatment
The therapy of a kidney inflammation depends on the cause and severity of the illness as well as the course form (acute or chronic).
It belongs to an effective treatment that Cause of nephritis as possible to eliminate or treat, For example, if the immune system is involved in the development of nephritis, it may be useful to prescribe anti-immune drugs. Such immunosuppressants are, for example, glucocorticoids (cortisone). If a drug or drug abuse is the trigger of nephritis (especially in interstitial nephritis), the drug should be discontinued or replaced by a better tolerated. In patients with streptococcal glomerulonephritis, the patient is given antibiotics. If existing underlying diseases such as systemic lupus erythematosus or HIV are the cause of (secondary) nephritis, their treatment should be intensified.
In addition, doctors often recommend kidney inflammation general therapy measures, These include, for example, physical protection and low-protein diet. When water retention in the tissue (edema) help a low-salt diet and possibly dehydrating drugs. If the kidney inflammation causes hypertension, the patient gets hypotensive.
When glomerulonephritis causes no discomfort, little or no protein and blood are excreted through the urine, and kidney function and blood pressure are normal, it is usually sufficient for the patient to be examined regularly by the doctor (including blood and urine tests).
In case of advanced kidney inflammation the kidneys can fail (kidney insufficiency). Then often one hemodialysis (Dialysis) or – as a last therapy option – one kidney transplant necessary.
Renal inflammation: course and prognosis
The prognosis of nephritis is very variable depending on the type, severity and course (acute / chronic).
An acute nephritis heals in many cases with timely diagnosis and treatment out. If left untreated, however, it can lead to complete kidney failure in severe cases. Of particular importance is early diagnosis and treatment in the so-called “rapid progressive” glomerulonephritis (RPGN). This can take a heavy course and quite quickly lead to kidney failure. Indeed, in four out of ten RPGN patients, blood dialysis will become inevitable over time.
Is a nephritis no longer curable, the right treatment is nevertheless important: this can often prevent or at least slow down further deterioration of kidney function. This may delay the time it takes the sufferer to undergo a blood or kidney transplant.