Hives (medical urticaria) is one of the common skin diseases. Typical symptoms are reddened skin and strong itchy wheals. Sometimes skin and mucous membranes swell. Hives can be acute or chronic and have a variety of triggers. Read more about the causes, symptoms, diagnosis, treatment and prognosis of hives!

Hives: Short overview
- symptoms: Redness of the skin, severe itching wheals and / or skin / mucosal swelling (angioedema)
- Causes: very diverse. Sometimes an allergy is behind it, but hives are often not allergic. Possible triggers are, for example, incompatibilities with food or medication, physical stimuli (cold, light, pressure, etc.), autoimmune reactions or chronic infections.
- Forms of urticaria: spontaneous acute hives, spontaneous chronic hives, physical forms of hives, aquagens hives, exercise-induced hives, etc.
- Treatment options: Avoid the trigger or treat the cause. Medicines (antihistamines, cortisone etc.). In certain cases further therapy such as UV treatment.
Hives: causes and risk factors
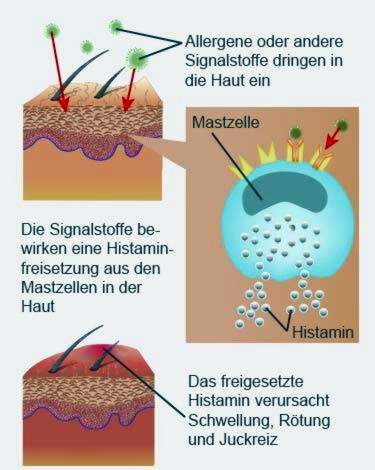
The emergence of hives is very complex. It is known that the typical itchy rash is formed by certain immune cells (mast cells) responding to irritation inflammatory messengers pour out. Above all, tissue hormone is one of these messengers histamine: It is mainly responsible for the symptoms of hives (wheals, itching, redness, swelling).
That the mast cells release more inflammatory messengers, may be an allergic reaction (on food, pollen, etc.). However, the mast cells can also be activated by other means. This means: Not every hives are allergic.
At the sight of conspicuous skin symptoms, many people fear that hives are contagious. However, the concern is unfounded: there is no danger of infection from the patients!
Various forms of hives
There are several forms of hives. They do not always occur individually: some patients have two or more of these subtypes at the same time.
The different forms of illness can be divided into three major groups:
- Spontaneous hives: Wheals and / or angioedema suddenly form here, without the doctor and patient being able to recognize an external trigger. This urticaria thus appears “as if out of nothing”. Depending on how long the symptoms persist, a distinction is made between spontaneous acute and spontaneous chronic hives (see below). About 80 percent of all patients have spontaneous urticaria, of which two thirds are acute.
- Physical hives: This includes all forms of hives that are triggered by physical stimuli (such as pressure, wind, cold contact, etc.). They account for only about 10 percent of all cases of hives.
- Other forms of hives: Causes are here for example physical exertion, contact with water or sweating. Such special forms of hives are found in less than 10 percent of all patients.
The different types of urticaria are described in more detail below.
Spontaneous acute hives
The hives symptoms occur here completely suddenly without apparent external stimuli up, but hold less than six weeks at.
A specific hives trigger can rarely be found. Significantly many sufferers suffer from acute respiratory or digestive tract infections; a connection seems likely therefore. Also, an intolerance or allergy to certain foods or food additives (dyes, preservatives, etc.) come as a cause in question.
The same applies, for example, to certain medications. These include so-called non-steroidal painkillers such as acetylsalicylic acid (ASA) and the ACE inhibitors (for high blood pressure and heart failure). They often cause pseudoallergic reactions of the skin.
Acute urticaria becomes threatening if the mucous membrane of the respiratory tract (pharynx, larynx, etc.) becomes very swollen (angioedema). Then the breathing air is difficult or impossible to get through. Those affected get breathless and can even suffocate!
In the event of a sudden shortness of breath, you should always call the rescue service immediately (# 112)!
Spontaneous chronic hives
Keeps a spontaneous hives longer than six weeks It is referred to as “spontaneous chronic urticaria” (or simply “chronic urticaria”). The symptoms of hives may either persist (continuously) or be repeated (with more or less long symptom-free phases in between).
Many triggers of spontaneous acute hives may also be responsible for spontaneous chronic hives. In some patients, several different factors trigger chronic urticaria.
The main causes of spontaneous chronic hives are:
- Chronic infections: Chronic or frequently recurring infections such as sinusitis, tonsillitis or jaw abscesses can trigger chronic urticaria. Many patients are also with the stomach germ Helicobacter pylori infected. Chronic infections, apart from urticaria, do not necessarily trigger further symptoms.
- Autoimmune reactions: In some patients defense cells are against the body’s own cells (autoantibodies), e.g. against the mast cells. This can also trigger a spontaneous chronic hives. It is also called “autoreactive hives.”
- Hypersensitivity (pseudoallergy): Here, the immune system is hypersensitive to certain additives in foods (dyes, preservatives, etc.), to natural flavorings in fruits or vegetables, or to cosmetics or medicines.
Sometimes, chronic urticaria also arises for other reasons, such as allergy.
Physical hives
An itchy hives can also be triggered by a variety of physical stimuli (pressure, cold fluid, etc.): In direct skin contact, an itchy rash forms at the site of the stimulus. It can also occur in another area of the body and additionally provoke low blood pressure or a fast heartbeat.
Depending on the physical stimulus one distinguishes different types of hives:
- Urticaria factitia (Urticarial dermographism): It is triggered by shear forces that act on the skin. Such shear forces occur, for example, when scratching, rubbing and rubbing the skin.
- Delayed pressure urticaria: Prolonged pressure triggers a staggered hives rash – the wheals do not form until three to twelve hours later. The affected persons therefore often do not recognize the direct connection with the pressure effect.
- Kältekontakturtikaria: The trigger is contact with cold objects, cold air, cold wind or cold liquids. For example, in the winter on uncovered body parts itchy rashes or redness may form.
- Wärmekontakturtikaria: The trigger here is the localized contact with heat (blow-drying, hot foot bath, etc.).
- urticaria: Both UV light (eg in the solarium) and visible light can be the cause.
- Vibratory urticaria: Vibrations such as those that occur when working with the jackhammer are also possible causes of hives.
Familial cold urticaria is a rare, genetically-related disease that is not classic hives (despite the similar name)!
Special forms of hives
The cholinergic urticaria arises from an increase in body core temperature. This can happen, for example, if you eat spicy food or take a hot bath. Also physical exertion as well as emotional stress can raise the temperature inside the body. As a result, pinhole-sized wheals form, but disappear within an hour. General symptoms are also possible (dizziness, nausea, headache etc.). Young people and young adults are particularly affected by this form of hives.
Physical exertion can also be a so-called Exercise-induced urticaria trigger. In comparison to cholinergic urticaria, the wheals are larger than a pinhead and the general symptoms (up to shock) are more common. Sometimes the symptoms are after eating, within four to six hours. These symptoms are then both stressful and food-induced.
In the contact urticaria Nettle rash develops through contact with so-called urticariogenic substances. Sometimes these are substances that the person is allergic to, such as certain foods or latex.
The contact urticaria can also occur independently of an allergy in contact with irritants. These may be, for example, the perfume Peru balsam (in cosmetics, medicines, cleaning agents, etc.), the preservative benzoic acid (food, etc.) or certain plants. Well-known examples are the itchy wheals, which causes skin contact with stinging nettles (this plant is also the namesake of hives).
Urticaria is very rarely caused by contact with water – no matter what the temperature. This so-called Aquagenic urticaria can put a heavy strain on those affected: On showers, swimming or a heavy downpour, the skin can react with itchy wheals. But this is not an allergy to the water!
Hives: treatment
The hives therapy is composed of different building blocks. The attending physician will customize them to each patient. The type of urticaria and the severity of the symptoms play a role here.
Avoid triggers
The most important building block of hives therapy is the Avoid the trigger as much as possible, Of course, this is only possible if it could be clearly identified.
When it comes to certain foods, sufferers should refrain from doing so. If certain medications are the trigger, they should be discontinued if possible. If this is not possible, they can often be replaced by a more compatible active ingredient.
Pressure urticaria can be prevented by, for example, shouldering only backpacks and bags with wide straps. If chronic infections (stomach germ, infections of the upper respiratory tract, etc.) turn out to be the cause of chronic hives, they must be treated properly.
It can be more difficult if, for example, physical stimuli such as heat or friction cause hives. The threshold is often very low here. Thus, people with a urticaria factitia sometimes even when wearing clothes that is not completely loose, get a hives. In addition, some physical stimuli (cold wind, UV rays, etc.) can hardly be completely avoided.
Medicines for hives
For the treatment of hives different drug groups are available:
antihistamines
Antihistamines are among the most important drugs in the treatment of hives. They can effectively relieve allergic and allergy-like symptoms in many patients. Antihistamines inhibit the effect of histamine. This messenger substance is mainly responsible for the hives symptoms.
As a rule, so-called H1 antihistamines of newer generations are used, which do not have a depressant (sedative) effect on the brain, so do not make you tired and drowsy. Examples of such agents are loratadine or desloratadine and cetirizine.
Antihistamines are usually taken as a tablet. In severe acute hives symptoms, it may be necessary to administer the drug as an infusion.
Even so-called H2-antihistamines can inhibit the histamine effect (other than H1-antihistamines). They are used in the treatment of hives but only in special cases, such as a difficult to treat chronic urticaria.
glucocorticoids(“Cortisone”)
In severe cases, urticaria often needs to be treated with cortisone (such as prednisolone). This may be the case if antihistamines do not adequately help with the hives symptoms.
The active ingredient is administered either in tablet form or as an infusion (in acute cases). Sometimes the doctor also prescribes a cortisone-containing ointment, such as in pressure urticaria.
As a general rule, cortisone should only be used for a short time and at low doses. This reduces the risk of side effects.
Leukotriene antagonists
These drugs have anti-inflammatory and antiallergic properties. Especially the active ingredient montelukast is sometimes used in difficult to treat hives. For example, if you can not get a grip on chronic urticaria with antihistamines, the doctor may also prescribe montelukast. Also in some other forms of urticaria (such as cold urticaria), this drug is an option if other treatments are not effective.
immunosuppressants
These are drugs that suppress the immune system. They are very effective, but are also not considered a standard treatment for hives. In some patients with chronic urticaria, however, the symptoms can only be alleviated with an antihistamine plus an immunosuppressant (such as cyclosporin A). The doctor will closely monitor the treatment to detect any side effects at an early stage.
Other medicines
The treatment of hives may be difficult, especially for chronic or chronic recurrent symptoms. In severe cases, it may then be necessary to administer other drugs to a patient – in addition to or as an alternative to the above-mentioned drugs. Some examples:
In spontaneous chronic urticaria doctors sometimes prescribe the drug hydroxychloroquineif other treatments do not help. This anti-inflammatory and anti-parasitic drug is otherwise used mainly in other diseases such as malaria and lupus erythematosus.
Some patients with difficult to treat chronic hives also benefit from treatment with omalizumab, This is a special antibody that blocks the secretion of proinflammatory messengers from mast cells.
For persistent cold urticaria, some patients are being tested antibiotics (like penicillin).
Hives: other treatments
In addition to drugs, other treatments may be considered for severe hives, depending on the type of disease.
This includes, for example, the habituation therapy (“Hardening”): It is useful if, for example, antihistamines do not help with light urticaria. Then the skin can be repeatedly and specifically exposed to the sun’s rays. This is meant to cause the body to slowly develop a tolerance to the light. In a similar way sometimes a stubborn cold contact urticaria can be treated (eg by regular cold showers). A habituation therapy must be carefully considered and accompanied by a doctor. It can significantly burden the patient.
In a difficult to treat Urticaria factitia can be a targeted irradiation with UV-B light (UV-B therapy) make sense.
Hives & home remedies
Home remedies can help with acute urticaria and support the effects of medication:
- Cold for itching: The itching can be relieved with cool compresses or a cold shower – but only if it is not a cold urticaria!
- Baking powder: It quenches the annoying itching when you stir it with a little water and apply it as a paste on the skin. You can also use it as an additive in bath water.
- Medicinal plants: Witch hazel (witch hazel) has an anti-inflammatory effect, soothes the itching and narrows the vessels. Therefore, ointments or creams with witch hazel are best suited to alleviate all symptoms of hives. The marigold has similar effects.
- Vinegar Wrap: A well-tried remedy for itching is the vinegar wrap. Moisten a kitchen towel with a vinegar-water mixture and place it on the skin.
Hives & Homeopathy
Some swear by the long-term treatment of chronic urticaria on the effect of homeopathy. However, to find the right remedy, the cause must be known. An experienced homeopath can choose the right homeopathic remedy for each patient. For example, they are used Urtica urens (Stinging nettle), Acidum formicicum (Formic acid) and Sulfur (Purified sulfur). In most cases, homeopathy supplements conventional medical treatment of hives.
Hives: symptoms
Although the triggers are very diverse – hives cause symptoms with a typical appearance:
- reddened skin
- very itchy skin blisters (wheals)
- sometimes extensive skin / mucosal swelling (angioedema)
One of the neurotransmitters responsible for these symptoms is more likely to be released in hives: the histamine, It dilates the small blood vessels in the skin, causing them to settle reddens, At the same time, the vessels become more permeable. As a result, more fluid enters the tissue: it forms wheals, These are superficial elevations of the skin of variable size, which are almost always surrounded by redness. They are fleeting: they disappear on their own within 24 hours. At the same time, however, new wheals may form elsewhere.
Sometimes the wheals are limited to a limited area, in other cases they cover practically the whole body. They go with you strong itching associated. It can be relieved by rubbing and rubbing the affected areas of skin, but less by scratching. Therefore, the skin is rarely scratched even with the strong itching.
In some patients with hives, sudden, pronounced swelling of the skin / mucous membranes occurs, for example on the face. These so-called angioedema may be accompanied by an unpleasant feeling of tension and itching. They form back more slowly than wheals (within 72 hours). With mucosal swelling of the respiratory tract (pharynx, larynx, etc.) it can be dangerous (breathlessness!).
Some patients have only the wheals, others (rarely) only the angioedema. Still others have develop both hives symptoms.
Hives: examinations and diagnosis
The reddish, itchy wheals are a typical disease that quickly suggests the diagnosis of hives. It is often more difficult for the doctor to find out the exact cause of the urticaria. The simplest but most important means for this purpose is the thorough patient survey: In conversation, the doctor raises the medical history of the patient (anamnesis). For this he can describe the symptoms exactly, asking for any pre-existing or underlying diseases and possible triggers of hives. Frequently asked questions of the doctor are:
- What symptoms do you have and since when do they exist?
- Is there a relationship between the symptoms and your job, your hobbies, any travel or leisure activities, the menstrual cycle?
- Are there any cases of hives or atopic diseases (atopic dermatitis, hay fever, allergic asthma etc.) in the family?
- Did you have or have an allergy or intolerance (to foods, medicines, etc.)?
- Are you aware of any infections, psychosomatic or psychiatric disorders?
- Do you have a suspicion of what might trigger the symptoms (certain foods, alcohol, smoking, cosmetics, cold, exercise, stress, etc.)?
- Which medicines do you use (occasionally or more often)?
Tip: Patients who have persistent or recurring hives should keep a diary of their symptoms. At the same time they should write down what they each ate and drank and what drugs they used. Other possible factors influencing the disease should also be noted. This can help the patient and doctor to find the cause of hives.
In spontaneous acute hives often no further diagnostic steps are necessary. However, if there is a suspicion that the urticaria is an allergic reaction, the doctor may allergy tests (like prick test) to find the trigger.
Further investigations in certain cases
Spontaneous chronic hives and other forms of urticaria require further investigation:
Help with chronic hives laboratory teststo detect any infections or other diseases as a trigger. So, for example, by means of a blood sample Differential blood picture and inflammatory parameters (like CRP). The patient may be suffering from a chronic infection or inflammation of the upper respiratory tract or the teeth Visit the ENT doctor or dentist make sense.
The blood of the patient can also be up Antibodies against infectious agents be investigated, for example against the bacterium Helicobacter pylori, If you actually find antibodies against this stomach germ, a stool sample and a mucosal sample from the stomach can confirm the infection.
Also revealing is the evidence of so-called Autoantibodies in the blood – Antibodies that act against the body’s own tissue. They could be the cause of chronic hives. Such autoreactive hives can be clearly demonstrated with a simple test (ASST = Autologous serum skin test).
Sometimes, chronic hives develop because the patient can not tolerate certain food ingredients (no allergy!): The hives rash is then a pseudo-allergic reaction to this irritant. For clarification, the doctor can special diet for three weeks recommend: During this time, the patient should abstain from all foods containing flavorings, preservatives, dyes or antioxidants. The prohibition concerns primarily industrially processed foods. If this pseudoallergenergic diet improves the symptoms, such additives are likely to be the cause of hives.
For confirmation, a more targeted provocation test For a while, suspicious foods are eaten in larger quantities. Such provocation tests can also be used to identify physical stimuli as causes of hives. Here, a body site is exposed to a certain stimulus. This can be cold or hot water, light or pressure.
The doctor can also rub the skin with a blunt tip. When it reddens, wheals and begins to itch, there is urticarial dermatography (urticaria factitia). The suspicion of an aquagent urticaria can also clarify with a provocation: For 20 minutes, a wet, body-warm compress on the skin.
Allergies are rarely the cause of chronic hives. But if there is a suspicion, bring allergy tests Clarity.
If the doctor suspects that the chronic rash is caused by a so-called mastocytosis, he removes a small amount in the area of the wheals skin sample and has her examined in the laboratory. The term mastocytosis refers to diseases that are caused by excessively many mast cells in the body. If this excess is limited to the skin, there is a so-called cutaneous mastocytosis. It is also called urticaria pigmentosa. Previously it was considered a sub-form of “conventional” hives, but not anymore.
For hives in children, experts recommend the same diagnostic procedures as adults. The possible causes of urticaria are the same in both age groups. There are only differences in the frequency of the different hives.
Hives: history and prognosis
About every fifth German (20 percent of the total population) gets a urticaria in the course of his life. This is usually one acute hives, It usually disappears within a short time.
In a small part of those affected, the wheals and itching last longer than six weeks. Then one is chronic hives emerged. Often their trigger can be identified. Then you can usually treat him (infections or other diseases) or largely avoid (medicines, food additives, etc.).
If the cause of chronic urticaria can not be determined, you can at least alleviate the symptoms (with medication, etc.). There is a small consolation for the patients: At some point, every chronic cure hives from alone. This can take years or even decades.
Additional information:
Books:
- Urticaria (hives): 100 questions – 100 answers: A patient guide (Marcus Maurer, akademos Wissenschaftsverlag, 2005)
Guideline:
- S3 Guideline “Urticaria” German Society for Allergology and Clinical Immunology and the German Dermatological Society (2011)
Support Groups:
- urticaria network e.V.