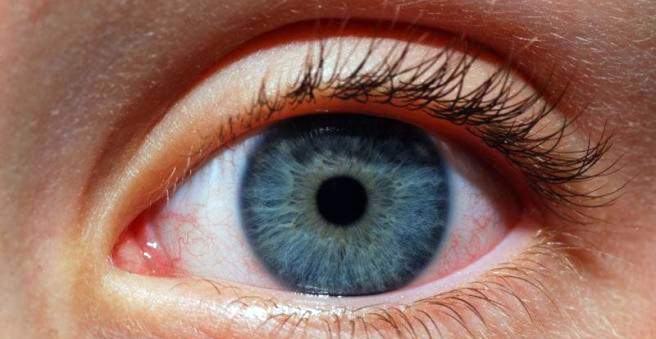
In uveitis or iris inflammation, the inner eye skin is inflamed. The eye appears red and hurts. The disease may be caused by viruses or bacteria or may be associated with another underlying disease. Affected are people of all ages. Read everything important about causes, symptoms and treatment of uveitis.
Uveitis: description
The eyeball is lined inside by three layers (eye skins). The middle eye skin is the uvea. In turn, it consists of the iris, the ray body and the choroid. If the uvea is inflamed, it is called uveitis. In this case, each section, ie iris, radiation body or choroid can be affected. Sometimes all sections of the uvea ignite. In Germany, about 100,000 people suffer from the inflammation each year.
Front uveitis
Inflammation in the anterior part of the uvea is most common. Either the iris, the ray body or both structures are inflamed. In most patients, the symptoms are sudden.
Middle uveitis
About one third of all inflammations inside the eye are moderate eye skin inflammations. Children are most likely to be between the ages of five and fifteen and young adults. Mostly both eyes are inflamed simultaneously.
Rear uveitis
The posterior uveitis affects only the choroid. It contains blood vessels and supplies the retina and surrounding layers with nutrients. In an inflammation of the choroid, therefore, the retina is often affected.
Uveitis: symptoms
Uveitis can affect one or both eyes. Often it comes very suddenly to the typical symptoms, sometimes develop the symptoms but also over a longer period. Depending on which section of the eye is affected, the symptoms also differ. Most of the time, they are the worse, the farther in the eye the inflammation is.
Front uveitis
Typical for a front iris inflammation are suddenly occurring, one-sided pain. The eye has a strong reddening and tears. Bright light is perceived as unpleasant. A few days before the first symptoms of uveitis occur, many patients have an uncomfortable feeling in the affected eye. Long-lasting inflammation can worsen vision. Some sufferers see flakes, shadows or lightning in front of the diseased eye.
In the case of an inflammation in the anterior segment of the eye, the iris and the lens may stick together, and the pupil then appears irregularly distorted (rounded). During the course of the disease, it is possible for the lens to cloud. This disease is also called “cataract”. Furthermore, the intraocular pressure can increase and cause a so-called “green star”.
Middle uveitis
The middle uveitis initially makes often no complaints. Occasionally, those affected see flakes or streaks in front of their eyes. Some complain of a diminishing visual acuity. If the disease persists for a long time, fluid may accumulate around the so-called “sharpest point of sight” (macula) on the retina. In this case, those affected see blurred and blurred. Sometimes, the retina then dissolves or breaks. Also a gray or a green star are possible complications of a central Uveitis.
Rear uveitis
Patients with a posterior uveitis often see everything “as if in the fog”. Sometimes shadows, spots or spots appear in front of the eye. If the vitreous also becomes inflamed, it can pull through the process of inflammation on the retina. The retina detaches and there is a risk of blindness.
Uveitis: causes and risk factors
Uveitis can be caused by pathogens such as viruses, bacteria, fungi or parasites. Also, rheumatic diseases are often triggers an iris. The causes are inflammatory processes resulting from the infection, which can also affect the eye skins. Sometimes uveitis is also caused by autoimmune processes or no apparent cause. More than half of the patients developed uveitis as part of comorbidities.
The following diseases are at increased risk for uveitis:
- Rheumatic diseases: ankylosing spondylitis, Reiter’s disease, sarcoidosis, Behcet’s disease, lupus erythematosus
- Joint inflammation (arthritis)
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis
- Inflammatory kidney disease
- multiple sclerosis
In the case of autoimmune uveitis, the body’s immune system reacts incorrectly for reasons that are still unexplained and produces antibodies against the middle eye skin.
Uveitis: examinations and diagnosis
In case of a sore or watery eye, fog or fog, or spots or clouds in front of the eye, the ophthalmologist should be consulted swiftly. Since uveitis can have many causes and is often part of another condition, the doctor will probably ask the following questions:
- Have you had a uveitis before?
- Do you have a chronic illness?
- Are there any autoimmune diseases or rheumatic diseases in your family?
- Have you ever had Lyme disease, tuberculosis or a herpes infection?
- Do you have problems with your joints?
- Do you often suffer from abdominal cramps or diarrhea?
- Do you often suffer from respiratory complaints?
The doctor then examines the eye with a special lamp that allows him to take a closer look at the fundus. In order to visualize the fundus, the pupil must be dilated with eye drops. In the case of iris inflammation, symptoms such as veiling vision occur, and the doctor can identify which section of the eye skin is flammable.
Inflammatory cells on the cornea
In inflammation, many cells and protein accumulate in the eye. They prefer to deposit on the cornea of the eye. This may cause the cornea to appear “dirty”. With a so-called slit lamp, the ophthalmologist can assess these soiling more accurately.
By means of an eye test the eyesight is checked. The intraocular pressure should also be determined in order to detect and treat a green cat early.
Fluorescence angiography shows whether the location of the sharpest vision on the retina (macula or yellow spot) is affected. For the examination, the patient gets a dye injected into a vein. This dye spreads through the bloodstream in the blood vessels of the eye. Subsequently, the fundus is considered.
If there is any suspicion that uveitis is a concomitant of another disease, further investigations are underway to expose the disease.
Uveitis: treatment
Uveitis is mainly treated with anti-inflammatory eye drops and ointments. In a bacterial iris inflammation eye drops are added with antibiotics. In order to prevent the iris from sticking to the lens, partially pupil-dilating eye drops must be given.
Sometimes cortisone-containing eye drops are also used. Occasionally, cortisone-containing medications are injected with a syringe around or into the eyeball under local anesthesia.
If uveitis is caused by a rheumatic or inflammatory disease, it must be treated at the same time.
Uveitis: Disease course and prognosis
Uveitis can start suddenly or slowly. If it lasts longer than three months, it is called chronic. Especially chronic uveitis can lead to complications such as gray or green cataracts or in the worst case to blindness.
Under therapy, anterior uveitis heals in most cases after five to six weeks. The middle uveitis is particularly often chronic, the posterior uveitis after healing, however, leave scars that reduce visual acuity.
If the disease occurs in the context of a chronic disease, the uveitis come back after a successful treatment. Therefore, the eyes of patients who are at increased risk for iris inflammation should be regularly monitored by the doctor.