Autoimmune hepatitis (AIH) is a liver infection that is triggered by a dysregulation of the immune system. Symptoms, like other forms of hepatitis, include fatigue, fever, joint pain and jaundice. The exact cause of autoimmune hepatitis is not yet known. The disease is treated with drugs that suppress the immune system (immunosuppressants). Here you will learn everything important about autoimmune hepatitis.
Autoimmune hepatitis: description
Autoimmune hepatitis (AIH) is a so-called autoimmune disease. These are diseases in which the immune system produces antibodies against the body’s own structures (autoantibodies). In the case of autoimmune hepatitis it concerns Autoantibodies to the liver tissue: They attack the liver cells and ultimately destroy them as if they were foreign tissue or a dangerous intruder.
The autoimmune hepatitis runs mostly chronic, An acute course is also possible.
About 80 percent of all patients with autoimmune hepatitis are women, The disease can occur at any age but is most common in middle-aged adults (especially between 40 and 70 years). In Europe, about one to two out of every 100,000 people suffer from autoimmune hepatitis every year.
Combination with other diseases
Often, autoimmune hepatitis occurs along with other immune-mediated diseases. These include, for example:
- autoimmune thyroiditis (autoimmune thyroiditis)
- Autoimmune inflammation of the biliary tract within the liver (primary biliary cholangitis)
- autoimmune inflammation of the bile ducts inside and outside the liver (primary sclerosing cholangitis)
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Sjogren’s syndrome
- Diabetes mellitus type 1
- celiac Disease
- Ulcerative colitis
- multiple sclerosis
- Vitiligo (white spot disease)
- Psoriasis (psoriasis)
Autoimmune hepatitis: symptoms
A acute autoimmune hepatitis causes symptoms of acute hepatitis such as fever, nausea and vomiting, upper abdominal pain and jaundice. Rarely, the disease is fast and difficult (brilliant) with acute liver failure. This becomes apparent, for example, from jaundice, blood clotting and consciousness disorders.
But most patients develop one chronic autoimmune hepatitis with a gradual course. For the most part, there are no or only unspecific complaints over a long period, such as:
- Fatigue and poor performance
- loss of appetite
- Aversion to fatty foods and alcohol
- Stomach and headache
- fever
- dizziness
- light stool and dark urine
- Yellowing of the skin, mucous membranes and the white dermis in the eye (jaundice)
In many patients, autoimmune hepatitis occurs together with other autoimmune diseases (such as type 1 diabetes mellitus, autoimmune thyroiditis, etc.). Then additional symptoms are added accordingly.
Most of the time, chronic autoimmune hepatitis ultimately leads to cirrhosis of the liver.
Autoimmune hepatitis: causes and risk factors
In autoimmune hepatitis, autoantibodies attack the liver tissue. This triggers inflammation, which ultimately destroy the liver cells.
Why the affected person’s immune system is directed against the body’s own tissue, you do not know. Experts suggest that patients have a genetic predisposition to autoimmune hepatitis. When external factors (triggers) are added, the disease breaks out. As such triggers are discussed, for example, infections, drugs, toxins or pregnancy.
Autoimmune hepatitis: classification
Autoimmune hepatitis (AIH) was originally divided into three variants:
- Type 1 autoimmune hepatitis (AIH1): It is by far the most common form of autoimmune hepatitis. Antinuclear antibodies (ANA) and / or antibodies against smooth muscle fibers (anti-SMA) are detected here. Often, certain antibodies also appear against neutrophilic granulocytes (a form of white blood cells), so-called p-ANCA (anti-neutrophil cytoplasmic antibodies).
- Type 2 autoimmune hepatitis (AIH2): Those affected have certain antibodies against so-called liver-kidney microsomes (anti-LKM1). Sometimes other autoantibodies also occur (Anti-LC1, Anti-LKM3). This type is commonly found in children and patients in the Mediterranean.
- Type 3 autoimmune hepatitis (AIH3): In the blood of those affected, only antibodies to soluble liver antigens / liver-pancreatic antigens (anti-SLA / LP) can be found.
Internationally common is a division into the Types 1 and 2, The type 3 autoimmune hepatitis is considered as Variant of type 1 considered: The autoantibodies typical of AIH3 (anti-SLA / LP) are sometimes associated with ANA and / or anti-SMA (typical autoantibodies in type 1 autoimmune hepatitis).
Autoimmune hepatitis: examinations and diagnosis
If autoimmune hepatitis is suspected, the doctor will tell you take a blood sample, In the laboratory, the liver values such as GPT, GOT, gamma GT and alkaline phosphatase (AP) are determined. Elevated readings indicate possible liver damage, such as autoimmune hepatitis. Also, the antibody type immunoglobulin G (IgG) is increased in this disease.
Additional blood levels such as albumin and Quickwert are measured to detect any diminished liver function.
The blood sample is also screened for autoantibodies against liver cells. Mostly, various autoantibodies can be detected. But that alone is not enough for a final diagnosis.
Caution: Autoimmune hepatitis, acute or very sudden and severe (fulminant), may lack autoantibodies and an increase in immunoglobulin G (IgG).
Using a Ultrasound examination of the liver can generally detect pathological changes in the tissue. This includes, for example, the conversion of liver tissue into connective / scar tissue (fibrosis of the liver). It ultimately leads to cirrhosis of the liver. This can be caused by a chronic autoimmune hepatitis, but also have other causes.
Note: About one third of all patients with autoimmune hepatitis already have cirrhosis of the liver at diagnosis.
Sometimes the doctor gives the patient tentative medicationthat suppress the immune system. Such immunosuppressants are standard in autoimmune hepatitis. If the patient’s symptoms improve due to the medication, this is an indication of autoimmune hepatitis, but not clear evidence.
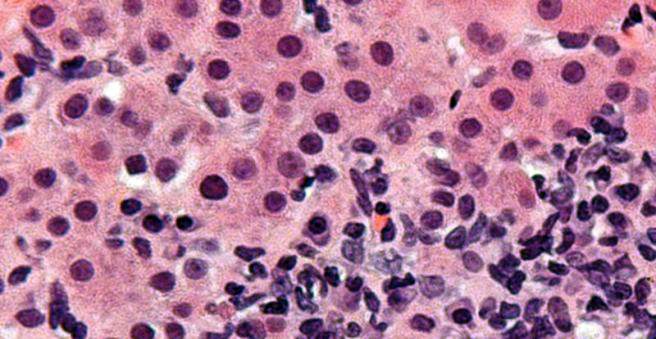
To help diagnose autoimmune hepatitis, the doctor takes one Tissue sample from the liver (Liver biopsy). It is examined more closely in the laboratory. If characteristic cell changes are found, it is very likely that autoimmune hepatitis is actually present.
Note: The TSH value should also be determined when evaluating autoimmune hepatitis. This hormone value provides evidence of thyroid function. Autoimmune hepatitis often involves autoimmune thyroiditis (autoimmune thyroiditis).
Autoimmune hepatitis: treatment
Autoimmune hepatitis can not be treated causally yet. This means that the dysregulation of the immune system can not be corrected. But you can administer drugs that suppress the immune system – so-called immunosuppressants, They inhibit the inflammatory processes in the liver. This helps against the symptoms and generally prevents further liver damage (including cirrhosis and liver failure).
In general, the two active ingredients for autoimmune hepatitis therapy azathioprine and Prednisolone (or its precursor prednisone) prescribed. By combining the two drugs, the cortisone preparation prednisolone can be dosed lower and usually at some point slowly settle (if possible within six to twelve months). Thus, side effects of prolonged high-dose cortisone therapy can be prevented.
Note: If autoimmune hepatitis is very mild with low inflammatory activity, treatment with immunosuppressants may be avoided in individual cases.
If the chronic autoimmune hepatitis has not yet led to cirrhosis of the liver, instead of prednisolone / prednisone, the active ingredient budesonide used in combination with azathioprine. This is also a cortisone preparation, but it should cause fewer side effects than prednisolone.
In certain cases, other medicines are used. For example, in difficult to treat autoimmune hepatitis immunosuppressants Ciclosporin or tacrolimus help.
Caution: Patients with severe autoimmune hepatitis (fulminant course) should be promptly admitted to a liver transplant center.
During the treatment are regular check-ups necessary at the doctor.
A longer cortisone treatment can bone loss (Osteoporosis). Adult patients therefore receive calcium and vitamin D as preventatives.
How long will the treatment take?
The immunosuppressive therapy in chronic autoimmune hepatitis usually causes the symptoms to subside (remission). The treatment should be continued for at least two more years. This maintenance therapy is possible only with azathioprine alone. If this is not enough to prevent relapse, patients must continue to take the cortisone preparation (prednisolone / prednisone or budesonide). This is dosed as low as possible.
After at the earliest two years one can try to sell the medicines in agreement with the attending physician. In some patients, the disease does not return then, at least not for the time being: it can still come after years to relapse, to prevent a recurrence of autoimmune hepatitis.
In most patients, however, the laboratory values deteriorate immediately after discontinuing the medication. You will need to continue taking immunosuppressants. In many cases, treatment must continue for many years.
Autoimmune hepatitis: history and prognosis
A mild autoimmune hepatitis can regress spontaneously. Otherwise, the disease can usually be treated well with immunosuppressants. Patients then generally have a normal life expectancy.
However, some patients do not respond well to the immunosuppressants. The Autoimmune hepatitis can then progress to liver cirrhosis despite consistent therapy – with the risk of liver failure and increased mortality. Then the last therapy option is a liver transplant.