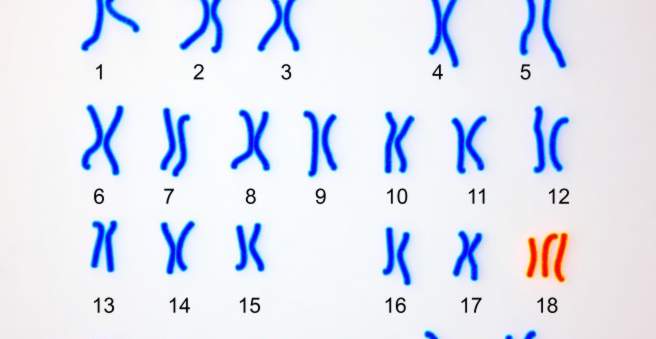
Trisomy 18 (Edwards syndrome) is a genetic disorder in which chromosome 18 (or parts thereof) is present in triplicate rather than in duplicate. This disturbs the development of a child already in the womb and causes various organ malformations. Most of the small patients die before or soon after birth. Read more about the symptoms and consequences, causes, diagnosis, treatment and prognosis of trisomy 18.
Quick Overview
- What is Trisomy 18? A serious hereditary disease, which is based on a faulty distribution of chromosome 18 in the development of a child. The disease was first diagnosed in 1960 by British dr. John Edwards described. It is therefore also called Edwards syndrome.
- Frequency: In Europe, one out of every 2,700 newborns with a trisomy 18 is born on average. Almost all of them are girls, because affected boys usually die in the womb. The reason for this is unknown so far.
- Symptoms and consequences: Depending on severity, for example, low birth weight, overlapping fingers, long and narrow skull, small mouth, receding chin, “faunal ears”, “cradle feet”, organ malformations (such as heart defects, cleft palate, malformations of the brain), thrives and growth disorders, respiratory problems
- Causes: Chromosome 18 (or part of it) is present in all or some of the child’s body cells in triplicate – two would be normal. Mostly the mistake happens by chance during the development of the baby. However, a higher age of the expectant mother is considered a risk factor.
- Treatment: Trisomy 18 is not curable. One can only try to alleviate the symptoms and consequences of the serious illness (e.g., gavage feeding problems or heart failure surgery).
- Forecast: Most children with trisomy 18 still die in the womb or soon after birth. Patients who survive slightly longer often show mental and physical disabilities and delayed development. In the rare mosaic trisomy 18, the prognosis can be significantly better.
Trisomy 18: symptoms and consequences
Children born with trisomy 18 (Edwards syndrome) often show characteristic features. These include:
- low birth weight
- Finger overlays (the little finger overlaps the ring finger, and the index finger the middle finger)
- long, narrow skull
- small facial skull, small mouth, small and back-receding chin
- Faunal ears (pointed ears, but low ears)
- “Cradle feet” (the shape of the sole reminds of the skids of a cradle)
In addition, there are usually a variety of internal organ malformations. Some of the most common are:
- cleft palate
- cardiac defect
- Kidney malformations
- Harnleiterfehlbildungen
- Malformation of the brain
- Lung malformation
The affected children often have nutritional problems, failure to thrive and respiratory problems. The growth is delayed. Many of the little patients can not walk free and speak only a few words.
This full image of Trisomy 18 is particularly evident in children with the disease variant Free Trisomy. in which all body cells undergo a free trisomy. In particular, in mosaic trisomy, the symptoms may be less pronounced, especially if only a few cell lines are affected by the chromosome disorder.
Trisomy 18: Causes and Risk Factors
A trisomy is a chromosomal mismatch in which the chromosome 18 (or part of it) does not occur twice (as usual), but three times in a cell. The risk increases, for example, with the age of the expectant mother.
Healthy body cells have 23 pairs of chromosomes (“double set of chromosomes”) – in each pair, one copy comes from the mother and the other from the father. In total there are 46 chromosomes. The germ cells (egg and sperm cells) have only one “simple set of chromosomes” (23 chromosomes), ie only one copy of each chromosome. In their formation, the double set of chromosomes was halved. Only then can a cell with a double set of chromosomes arise during fertilization by the fusion of an egg and a sperm cell. Out of this countless divisions of cells, the new organism emerges.
The mistake that leads to trisomy 18 sometimes happens during the formation of the germ cells. In other cases, it is only after fertilization in the development of the fetus or embryo to do so. Accordingly, doctors distinguish different variants of trisomy 18:
Free Trisomy 18
At free trisomy already before fertilization of an egg there is an incorrect distribution of a chromosome 18. In more than 90 percent of cases this erroneous assignment happens at formation of an ovum (in other cases at creation of a sperm cell). This error often occurs spontaneously and rarely follows certain inheritance patterns.
Because the defect is already present in a germ cell (egg or sperm cell), it can also be found in all body cells of the developing child: All cells have three (instead of two) copies of chromosome 18. The affected children show the full picture of the disease ,
With around 94 percent Free Trisomy 18 is the most common variant of the disease.

Mosaic trisomy 18
In the mosaic trisomy 18, the error occurs relatively late in the development of the fertilized egg. Therefore, only individual cell lines have three chromosomes 18. All other cell lines have the normal number of two chromosomes 18 and are thus healthy. The fewer cell lines are affected, the lower the trisomy-18 symptoms and the higher the life expectancy of the affected child.
Mosaic trisomy 18 only does about five percent of all illnesses.
Translocation trisomy 18
The starting point of this variant is a so-called “balanced translocation” in a parent, usually the mother: it has the normal number of chromosomes in their cells. However, as a result of a chromosomal break, one part of chromosome 18 was falsely attached to another chromosome (translocation). However, since all the genes of chromosome 18 are present in normal numbers (although not in a normal arrangement), this is called “balanced translocation”. The affected parent is perfectly healthy.
However, when a child is conceived, the transmission of the translocation chromosomes can lead to a child with “unbalanced translocation” and thus a translocation trisomy 18: A part of chromosome 18 is present in triplicate. Doctors speak here too partial trisomy due to translocation.
at about one percent all trisomy-18 patients have a translocation trisomy.
Second most common trisomy
In addition to Trisomy 18, there are other trisomies – ie chromosome disorders with a supernumerary chromosome (or surplus chromosome parts). The most common is trisomy 21 (Down syndrome). In second and third place follow trisomy 18 and trisomy 13 (Pätau syndrome). Children who have one of these three trisomies are potentially viable. In contrast, unborn children with other trisomies die very early in development. In these cases, pregnancy is often not noticed.
Trisomy 18: examinations and diagnosis
If a gynecologist at the regular Ultrasound examinations in pregnancy If abnormalities are discovered in the unborn child, he may suspect a chromosome disorder such as trisomy 18. These suspicious abnormalities include, for example, delayed growth as well as malformations on the child’s abdomen, head, or heart, which are in line with the picture of trisomy 18. In addition, trisomy 18 often involves only one artery (instead of two) in the umbilical cord. The amount of amniotic fluid can be an indication of a disease.
Triple Test
In addition, certain maternal blood values be elevated at a trisomy. This blood test is also known as a triple test or MoM test (Multiples of the Median). It helps to identify unborn children who are at an increased risk for trisomy. However, the triple test allows no sure diagnosis! He can only estimate the risk of certain chromosome disorders in the child. If the readings are conspicuous and the expectant parents want to be certain, invasive examinations are needed.
Despite its low significance, the Triple Test has a great advantage: in contrast to the more detailed invasive examinations (such as amniocentesis), it bears no risks for pregnancy and the unborn child.
Invasive investigations
In order to clarify a suspected trisomy 18, the doctor can perform an invasive examination method: He can take a tissue sample of the mother cake (chorionic villus sampling) or some amniotic fluid (amniocentesis = amniocentesis). Both samples contain childlike cells. Their genetic material is examined in the laboratory for chromosome disorders such as trisomy 18.
In both invasive examinations, the sampling may harm the child and possibly even cause a miscarriage.
Chromosome analysis using a blood sample
The blood of a pregnant woman also contains traces of the child’s genome (DNA). For some time, it has been possible to isolate this child’s DNA from the mother’s blood and to examine in the laboratory for chromosome disorders. These prenatal blood tests include, for example, Harmony Test, PraenaTest and Panorama Test.
In contrast to invasive methods of prenatal diagnosis (such as amniocentesis) these are blood tests safe for the unborn child, You can, however, with high reliability recognize an existing trisomy (such as the Edwards syndrome).
The DNA test is at a Risk pregnancy from the completed 9th week of pregnancy (Harmony test: from the completed 10th week of pregnancy) offered. Pregnant women, for example, are women whose ultrasound examination or first-trimester screening has revealed abnormalities in the unborn child. Even in older pregnant women or those with a family history the doctor may suggest a prenatal blood test.
The test usually has to be paid out of pocket (as IGeL = Individual health care) – the health insurances do not take over the costs in principle. Depending on the test and the scope of the analysis, these amount to several hundred euros. In addition, there are the costs for the medical services associated with the test, ie examination, education and human genetic counseling. The latter is intended to ensure that the expectant parents understand the meaning and possible consequences of the test and are then left with the test result alone.
In some cases, some health insurance companies take the cost of a prenatal blood test. Pregnant women should discuss the possibility of reimbursement with their health fund before they have the test done.
Trisomy 18: treatment
Trisomy 18 can not be healed. All therapeutic measures are merely aimed at relieving the symptoms of the child or maintaining the organ functions. For example, if the child has nutritional problems, special suckers or tube feeding may be helpful. In case of breathing problems, the breathing can be monitored by monitor.
The very common heart defects are sometimes operated on. Also in other organ malformations such as disorders of urinary outflow surgery can be performed. In general, surgical corrections of malformations are carefully considered because it is unclear whether they actually improve the prognosis and quality of life of the small patients.
A psychological counseling of the parents is useful in many cases, since usually the death of the child is to be expected. Especially in the first weeks of life, the life of the newborn is at risk.
Trisomy 18: Disease course and prognosis
More than 95 percent of children with trisomy 18 still die in the womb, often in the first trimester of pregnancy. The life expectancy of live born trisomy 18 children is not very high. If the organ malformations are already known before birth, delivery can take place at a maternity ward with subsequent maximum pediatric care. This can increase the chances of survival of the child.
The average life expectancy of trisomy 18 children is one to two weeks. Only five percent reach the first year of life, and only one percent is the age of ten. In individual cases, the prognosis depends on various factors. This includes, above all, the type of trisomy 18: small, partial trisomies and slight mosaic trisomies have a better prognosis than a free trisomy 18.
Even if the child survives his first birthday, one has to reckon with severe physical and mental disabilities and developmental delays. In addition to organ malformations, many children are prone to seizures, severe postural deformity, and feeding problems. In rare cases patients with trisomy 18 reach adolescence. There are also reports of individual Trisomy 18 patients who survived until the age of 27.
The unfavorable prognosis is especially true for the full picture of the disease – the free trisomy 18. It is by far the most common disease variant. The rarer mosaic trisomy 18 often has a better prognosis. In some cases, the development of the child may even be almost normal if only a few cell lines are affected by the chromosomal disorder.
Not to be underestimated is the psychological burden of the parents, who live every day with the certainty that their child can suddenly die. parents of Trisomy 18-Children should therefore take advantage of the various counseling and support services.
Additional information
Support group:
- LEONA e.V. – Association for parents of chromosomally damaged children