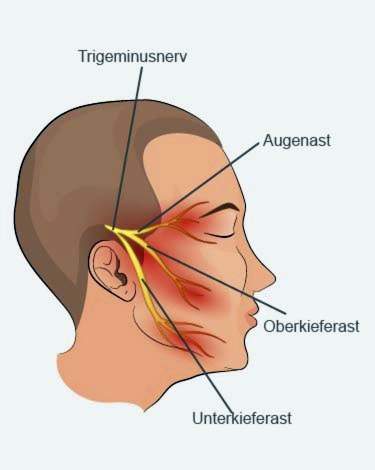
With a trigeminal neuralgia suddenly violent facial pains occur. They usually last only a few seconds, but can always return. The complaints start from the trigeminal nerve (Latin for trilling nerve). He provides over three branches face, forehead, eyes, chin, upper and lower jaw. When damaged, the nerve reports severe facial pain to the brain. Read all important information about causes, symptoms, diagnosis, therapy and prognosis of trigeminal neuralgia!

Quick Overview
- Definition: Violent, attack-like facial pain emanating from the trigeminal nerve.
- Frequency: Only about 4 out of every 100,000 people in Germany suffer from trigeminal neuralgia. The disease usually occurs after the age of 40 years. Because of the higher life expectancy, there are slightly more female than male patients.
- Causes: often unclear (classic trigeminal neuralgia). Sometimes there is a causative disease (symptomatic trigeminal neuralgia).
- symptoms: lightning-fast, very short and extremely severe attacks of pain on the face, often triggered by touch, speech, chewing, etc.
- Doctor treating: Neurologist or neurosurgeon
- Therapy: Medication or surgery, possibly supplemented by psychological care.
- Forecast: Through therapy, the pain can be controlled, but not permanently eliminated.
Trigeminal neuralgia: causes and risk factors
Depending on the cause, the International Headache Society (IHS) divides trigeminal neuralgia into two groups:
Symptomatic trigeminal neuralgia
Symptomatic trigeminal neuralgia is present when radiological imaging or surgery is used to detect another disease as the clear cause of pain attacks. These possible causes include:
- Diseases in which the protective sheaths of the nerve fibers (myelin sheaths) in the nervous system are destroyed (demyelinating diseases): e.g. Multiple sclerosis (MS)
- Brain tumors, especially so-called acoustic neuromas: These are rare, benign tumors of the auditory and equilibrium nerves. They press the trigeminal nerve or an adjacent blood vessel so that both are pressed against each other. This triggers the pain.
- stroke
- Vascular malformations (angioma, aneurysm) in the area of the brainstem
Patients with symptomatic trigeminal neuralgia are on average younger than people with the classic form of disease.
Classic trigeminal neuralgia
In classical trigeminal neuralgia, no other disease can be identified as the cause of the symptoms. This disease form is therefore also called “idiopathic trigeminal neuralgia” (idiopathic = no known cause).
Experts suspect that the pain in the affected by the fact that adjacent blood vessels press on the nerve and so the envelope of the nerve (myelin sheath). Such pathological contact between vessel and nerve is more likely when the walls of the arteries are thickened and rigid. This is the case with an arteriosclerosis (arteriosclerosis). This may therefore increase the risk of trigeminal neuralgia.
Trigeminal neuralgia: symptoms
Characteristic of a trigeminal neuralgia are attacks like facial pain, the
- suddenly and in a flash,
- are extremely strong and
- last a short time (fractions of seconds to two minutes).
Trigeminal neuralgia pain is one of the most severe pains ever. They can repeat themselves up to a hundred times a day (especially in the classic disease form).
Those affected often describe the pain as “shooting out of the blue” or “surge-like”. Sometimes the pain occurs without any trigger. But very often there are such triggerthat cause a pain attack. This can be something quite commonplace like:
- Touch of facial skin (by hand or wind)
- Speak
- Brush teeth
- Chewing and swallowing
For fear of a pain attack, some patients eat and drink as little as possible. You can thereby (dangerously much) lose weight and develop a fluid deficiency.
Differences between the forms of illness
At a classic trigeminal neuralgia usually the second or third major branch of the trigeminal nerve (trigeminal nerve) is affected. Patients therefore often have unilateral pain in the upper or lower jaw. There is no pain between the individual attacks. The violent, shooting pain can trigger a reflex twitching of the facial muscles. It is also called as Tic douloureux (French for “painful muscle twitching”).
If all three branches of the trigeminal nerve or both sides of the face are affected, that speaks rather for one symptomatic trigeminal neuralgia, In addition, the patients are usually not pain-free in this form of disease between attacks. Often also occur sensory disturbances (for example, tingling, numbness, etc.) in the supply area of the trigeminal nerve.
Trigeminal neuralgia can be very stressful psychologically. Therefore, many sufferers suffer from a depressive mood.
Trigeminal neuralgia: examinations and diagnosis
Not every pain in the facial area is trigeminal neuralgia. For example, TMJ problems, diseases of the teeth or cluster headache can cause facial pain.
It is important to distinguish trigeminal neuralgia from many other forms of headache and facial pain. Based on the typical course of pain, the family doctor can usually identify a trigeminal neuralgia. But the right contact person for the diagnosis and follow-up examinations for this disease is one Specialist in Neurology or a Specialist in neurosurgery.
The first step in suspecting a trigeminal neuralgia is the Survey of the medical history (Anamnesis): The doctor interviews the patient in detail about his complaints. Possible questions are:
- Where exactly are you in pain?
- How long does the pain last?
- How do you feel the pain, for example, as stinging, oppressive, jerky?
- Do you have any other complaints besides the pain, such as emotional disturbances on other parts of the body, blurred vision, nausea or vomiting?
- Are the pain attacks very troublesome for you?
Afterwards, the doctor leads one physical examination by. The doctor, for example, pays attention to whether the sensibility (sensibility) in the facial area is normal.
Further investigations must clarify whether a causative disease of the trigeminal neuralgia underlying or not. Symptomatic and classic trigeminal neuralgia are treated differently. Depending on the symptoms, the doctor may perform one or more of the following examinations:
Magnetic Resonance Imaging (MRI): Using magnetic resonance or magnetic resonance imaging, the doctor can check whether a disease such as multiple sclerosis, brain tumor, stroke or vascular malformation (aneurysm) triggers the trigeminal neuralgia.
Collection and analysis of nerve water: With a thin, fine hollow needle, the doctor can take a sample of the nerve water (cerebrospinal fluid) from the spinal canal (CSF). In the laboratory it is examined whether the patient suffers from multiple sclerosis.
Computed Tomography (CT):In particular, the bony structures of the skull can be examined. Possible pathological changes can be the cause of pain attacks.
Angiography or Magnetic Resonance Angiography (MRA): On the basis of an X-ray examination of the blood vessels (angiography) in the cranial area, possible vascular malformations can be detected. In nuclear spin angiography, X-ray imaging of the vessels is performed by magnetic resonance imaging. The imaging of the blood vessels is also useful before surgery, so that the neurosurgeon sees exactly where the blood vessels in the operating area.
Electrophysiological examinations: These include, for example, trigeminal SEP (examination of the functioning of sensory nerve tracts, eg sensation of touch and pressure), examination of the eyelid reflex, massaging reflex, etc.
Other investigations: If necessary, further examinations are necessary, for example with the dentist, orthodontist or ENT specialist.
Trigeminal neuralgia: treatment
Basically, the trigeminal neuralgia can be treated either with medication or surgery. There are differences between the two types of disease:
- A classic trigeminal neuralgia is first and foremost medicated. It is operated only if the drugs do not work or the side effects are too serious.
- Symptomatic trigeminal neuralgia often removes the cause (such as a brain tumor) surgically. The procedure can relieve the pain or even completely switch it off for a while.
The fact that the causes of facial pain have not been fully resolved makes trigeminal neuralgia therapy more difficult. If the right treatment is found, the pain can be well relieved, but never completely or permanently “off”.
Medicines for trigeminal neuralgia
The usual pain medications (such as ibuprofen, diclofenac, etc.) unfold their effect too late for the lightning, short pain attacks. Trigeminal neuralgia therefore requires preventive long-term therapy with special pain medications.
For example, the active ingredients are used carbamazepine and oxcarbazepine, They are also used to treat epilepsy. Often also helps the muscle-relaxing drug Baclofen, If possible, the doctor prescribes only one active ingredient in trigeminal neuralgia alone (monotherapy). For severe pain, two drugs may be useful (combination therapy).
Acute pain can be treated with the anticonvulsant phenytoin in hospital for inpatient treatment.
Surgical therapy for trigeminal neuralgia
Surgery can relieve the pain of trigeminal neuralgia or even eliminate it in the long term. However, they can occur again after a few years. In addition, every operation naturally involves risks. Patients should therefore discuss the chances and risks of the procedure with the attending physician prior to the operation.
In principle, trigeminal neuralgia has three surgical options:
Classic surgical procedure (microvascular decompression according to Jannetta)
This method is used in healthy people with low surgical risk. Through an opening in the back of the head, the doctor places a Goretex or Teflon sponge between the nerve and the vessel. This is to prevent the trigeminal nerve from coming under pressure again.
Immediately after the procedure, about 82 percent of the patients are painless. Ten years after the operation, it is still 67 percent. For follow-up surgeries, the success rate for pain relief is lower.
Possible side effects / risks of surgery include bleeding, cerebellar injuries, and on the affected side loss of hearing and facial numbness.
Percutaneous thermocoagulation (according to Sweet)
This procedure is suitable for people with a higher surgical risk. The doctor pushes a probe through the skin to the so-called ganglion Gasseri. This is an accumulation of nerve cell bodies of the trigeminal nerve. There, especially the pain fibers of the nerve are destroyed – either by local heat application, mechanically by pressure balloon or chemically by means of glycerine.
The success rate right after the operation is high: About 90 percent of the patients are initially pain-free. However, this success only last for about every second.
Possible side effect is a sometimes painful loss of feeling on the affected side of the face.
Radiosurgical procedure
This is a comparatively gentle method of radiotherapy. The doctor irradiates the trigeminal nerve near the brainstem once with a high radiation dose. For this he uses the so-called Gamma Knife or Cyber-Knife, Compared to the other two surgical methods, this procedure is less likely to cause complications. But also the chances of success are lower:
If this procedure is performed without any previous other surgery, 63 to 75 percent of trigeminal neuralgia patients will be pain free after the procedure. If another surgery has already taken place, chances of success are much worse. Overall, the effect of the therapy usually only after a few weeks, so much later than the other methods.
The doctor treats trigeminal neuralgia in patients with multiple sclerosis by medication (active substance misoprostol) or by means of percutaneous thermocoagulation and radiosurgical procedures.
Trigeminal neuralgia: course and prognosis
The course of the disease in trigeminal neuralgia is very variable. It is hardly predictable how much time will pass before the next pain attack. Sometimes there are days, weeks, months or even years between individual attacks.
In about 29 percent of those affected, it even remains with a single attack of trigeminal neuralgia. Often, however, the attacks only start occasionally, but accumulate over time.
The trigeminal neuralgia can massively affect the everyday life of those affected – not only by the violent pain attacks themselves, but also by the fear of the next attack. The emotional wellbeing can suffer as well. Therefore, some patients additionally develop a depressive mood. Therefore, a medical and / or surgical treatment of trigeminal neuralgia should, if necessary, be extended by one psychological or psychotherapeutic treatment be supplemented.
With the right treatment plan, you can reduce or eliminate the pain of a trigeminal neuralgia, at least for a while. However, the disease can not be completely cured at present. So far it is not known if and how one trigeminal neuralgia can prevent.
Additional information
Book recommendations:
- Trigeminal neuralgia: when life gets out of hand (Simone Brockes, Ennsthaler, 2017)
guidelines:
- S1 guideline “Trigeminal neuralgia” of the German Society of Neurology (2016)