A gastric ulcer (medical gastric ulcer) is a deep wound in the gastric mucosa. It is typically noticeable by upper abdominal pain. Gastric ulcers are mainly caused by an excess of stomach acid. Often a colonization of the gastric mucosa is responsible for the bacterium Helicobacter pylori. With medication, a gastric ulcer can usually be completely cured. Find out, among other things, which risk factors favor a stomach ulcer, which warning signs you should look out for and how the treatment and prognosis look like.

Quick Overview
- What is a stomach ulcer? deep wound in the gastric mucosa; Men and women are about equally affected.
- Causes: Infection with the gastric bacterium Helicobacter pylori, disturbed gastric emptying, disturbed gastric acid production, certain drugs, genetic stress, unfavorable living habits (stress, alcohol, etc.)
- symptoms: Upper abdominal pain, nausea, feeling of fullness, loss of appetite, possibly tarry stool, anemia
- complications: Bleeding from the ulcer, stomach opening with peritonitis
- Examination: Doctor-patient interview (anamnesis), physical examination, blood test, ultrasound, gastroscopy, breath test
- Therapy: medication; in case of complications surgery
- Forecast: good for early treatment and stomach-friendly lifestyle
Gastric ulcer: symptoms
Gastric ulcers are among the most common gastrointestinal diseases. Even more often occurs only Duodenal ulcer (medical ulcer duodeni).
Both gastric and duodenal ulcer typically cause oppressive or burning pain in the upper abdomen (Epigastrium = between costal arch and navel). The complaints often occur in connection with eating or drinking. However, people with a duodenal ulcer often have pain with an empty stomach (fasting pain) and at night. In contrast, an increase in pain shortly after eating is a typical ulcer.
Furthermore you can anorexia, bloating, Nausea and vomiting such as weight loss indicate a gastric ulcer. Some patients also develop signs of bleeding gastric ulcer anemia (Anemia).
Some gastric ulcers do not cause any discomfort. They are then often discovered by chance during an examination or become noticeable only in the case of complications.
Rarely, gastric cancer can trigger similar symptoms as gastric ulcer. Clarity brings then a gastroscopy, in the context of which one takes a tissue sample (biopsy) and histologically examined histologically.
Gastric ulcer: complications
Certain analgesics and anti-inflammatories such as acetylsalicylic acid (ASA), ibuprofen or diclofenac can cause stomach ulcers on the one hand. On the other hand, if taken regularly, they can suppress the pain stimulus so that sufferers do not notice the typical gastric ulcer symptoms. As a result, unnoticed (severe) complications may develop.
The most common complication of gastric ulcers (and duodenal ulcers) is one Bleeding from the ulcer, One possible sign of this is a pitch-black stained chair (tarry stool). The black color develops when the blood from the ulcer is decomposed by the acid gastric juice.
Sometimes the bleeding from the gastric ulcer is so small that the stool does not discolor. However, persistent blood loss is reflected in a decreased hemoglobin level in the blood.
If a gastric ulcer bleeds heavily, the person may even vomit the blood (vomiting blood or hematemesis). This is life threatening and must be treated immediately!
Rarely does a gastric ulcer break through the stomach wall into the abdominal cavity. Digested food and acid can enter the abdominal cavity through this hole Peritonitis (Peritonitis). Affected then feel massive pain throughout the abdomen (peritonitis) and get a fever.
The breakthrough of a gastric ulcer is an emergency that needs to be treated as quickly as possible!
Gastric ulcer: causes and risk factors
Mental factors: “With so much stress you’ll get a stomach ulcer sooner or later” – such warnings are heard more often. In fact, stress in a professional or private environment seems to increase the risk of gastric ulcer. This is probably due to the fact that the body produces excessive stomach acid while maintaining stress, while at the same time producing less protective mucus.
Even acute stress or shock situations and depression seem to favor the development of gastric ulcers. However, they are most likely not the only triggers. Rather, they only work in combination with other risk factors.
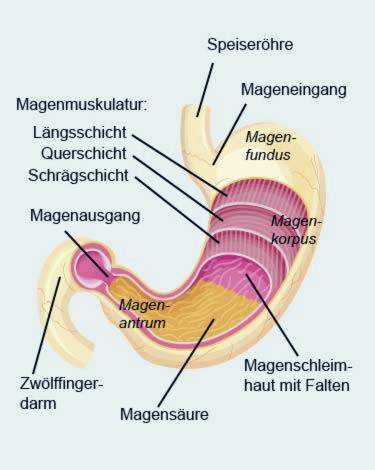
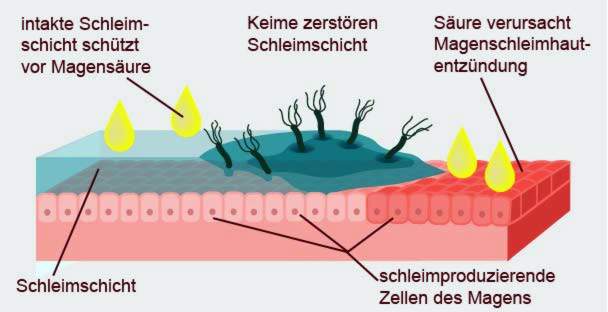
Too much stomach acid: A gastric ulcer occurs when the aggressive gastric acid and the protective factors of the gastric mucosa (for example mucus and acid-neutralizing salts) are in imbalance. If the acid is too strong or the protective factors are too weak, the mucous membrane is damaged and a gastric ulcer can develop. By such an imbalance inflames first the gastric mucosa (gastritis). If the inflammation persists for a long time or returns again and again, a gastric ulcer may develop over time.
Disturbed processes in the stomach: Disturbed stomach movements are also suspected of causing gastric ulcer. If the stomach defecates and at the same time more bile acid flows back into the stomach, this may favor the development of a gastric ulcer. An increased ulcer tendency is also seen in humans, who produce only reduced amounts of the protein that repairs the gastric mucosa.
Colonization with Helicobacter plyori: This bacterium, which does not mind aggressive stomach acid, is the main cause of gastric ulcer. In 75 percent of all patients with a gastric ulcer and in up to 99 percent of all patients with a duodenal ulcer, the bacterium can be detected. The stomach germ is not responsible for an ulcer alone. Only in combination with other risk factors can ulceration occur. These risk factors include the use of certain medications and unfavorable dietary habits (see the following).
Taking certain medications: Particularly susceptible to gastric ulcer are people who regularly take painkillers and anti-inflammatory drugs from the group of non-steroidal anti-inflammatory drugs (NSAIDs or NSAIDs). These include active ingredients such as acetylsalicylic acid (ASA), ibuprofen and diclofenac. Particularly problematic is the combination of cortisone (glucocorticoids) and non-steroidal anti-inflammatory drugs.
Unfavorable dietary and lifestyle habits: Smoking, alcohol and coffee increase gastric acid production and thus increase the risk of gastric ulcer. Certain foods (such as spicy foods) can also irritate the stomach lining. What is tolerated is individual but very different.
Genetic preload: In some families gastric ulcers occur frequently. This suggests involvement of genetic factors in ulcer formation.
Other causes: Gastric ulcers can very rarely also be caused by metabolic diseases such as hyperparathyroidism (hyperparathyroidism) or a tumor disease (gastrinoma, Zollinger-Ellison syndrome). Even after major operations, accidents or burns, stomach ulcers can develop. Since in these situations different “stress reactions” take place in the body, such a gastric ulcer is also called a stress ulcer. In addition, people over the age of 65 and those with blood type 0 are more susceptible to gastric ulcers. In addition, in people who have ever had such an ulcer, can easily form a new one.
Gastric ulcer: treatment and prevention
How doctors treat a gastric ulcer depends mainly on the cause. A particularly important factor is whether the gastric bacterium Helicobacter pylori was detected in the stomach in the patient. If this is the case, the doctor prescribes gastric ulcer therapy in the first place antibiotics one to eliminate the infection. To do this, the person takes two different antibiotics (clarithromycin and amoxicillin or metronidazole) daily for seven days. In addition, the doctor will use an acid-reducing drug (for example, a so-called “Proton pump inhibitors“). As a “stomach protection” they inhibit the production of stomach acid, so that the attacked mucous membrane can recover.
Helicobacter antibiotic treatment is referred to as “Helicobacter pylori eradication therapy”. It is successful in more than 90 percent of patients with gastric or duodenal ulcer. In rare cases, however, the pathogens of gastric ulcer are resistant to one of the antibiotics. Then effective gastric ulcer therapy is more difficult.
If the bacterium Helicobacter pylori can not be detected, no antibiotics are used, only acid-reducing drugs, especially “proton pump inhibitors”. The therapy is symptomatic. This means that it only alleviates the symptoms. Without the damaging effect of stomach acid, the gastric ulcer usually heals by itself. In addition, however, it must be ensured that the person concerned completely avoids stomach-irritating substances and foods (alcohol, coffee, nicotine) until the gastric ulcer has healed.
In addition to proton pump inhibitors, H2-antihistamines and antacids also have an acid-reducing effect. Read more about the effects and use of these drug classes in gastric ulcer treatment:
|
Proton pump inhibitor (“stomach protection”) H2 antihistamines antacids |
Gastric ulcer treatment: gastroscopy
After completion of the medical gastric ulcer treatment, gastroscopy is performed within about six to eight weeks (gastroscopy). It is checked if the ulcer is really completely healed.
In addition, a gastroscopy can be performed to treat complications: If the ulcer bleeds, the doctor can inject a special protein glue (fibrin glue) into the wound in the context of gastroscopy to so stop the bleeding.
Gastric ulcer treatment: surgery
Gastric ulcers are rarely operated on today. For example, with a very stubborn boil, it may be useful to remove part of the stomach. As a rule, the vagus nerve (vagus nerve) is also severed (vagotomy) in order to reduce gastric acid production.
Complications of a gastric ulcer may also require surgery. For example, a stomach opening must always be surgically treated.
Gastric ulcer: examinations and diagnosis
The right person to contact if you suspect a stomach or duodenal ulcer is a specialist in internal medicine and gastroenterology. Affected can go first but also to their family doctor. He may then initiate further investigations if necessary.
anamnese
First, the doctor will talk in detail with the patient to raise his medical history. Possible questions are:
- Where exactly do you have abdominal pain?
- Does the pain of eating and drinking become stronger or weaker?
- Do you drink alcohol? When Yes, how much?
- Do you smoke? When Yes, how much?
- Do you drink coffee? When Yes, how much?
- Do you have a lot of stress right now?
- Are you taking over-the-counter painkillers like acetylsalicylic acid (ASA), ibuprofen or diclofenac?
- Do you take any other medications?
- Have you or a family member ever had a stomach ulcer or duodenal ulcer?
- Have you ever had a gastroscopy done? If yes, when?
- Do you have any pre or basic diseases?
Physical examination
After the interview, the doctor will examine the patient briefly if necessary. He gently feels his stomach. So he gets an impression of how severe the pain is. In addition, the palpation may show a defense tension: This means that involuntarily tense the abdominal muscles due to the pain. For the doctor, this is a sign that he must immediately initiate further examinations and appropriate treatment.
Blutntersuchungen
If a gastric ulcer is suspected, the patient’s blood is also examined. If there is a bleeding gastric ulcer, continuous blood loss may be reflected in anemia (anemia). Typically, then the hemoglobin (Hb) is lowered.
Various blood levels can also indicate whether inflammation is taking place in the body (number of white blood cells, CRP etc.). This is possible with a gastric ulcer, which has broken through the stomach wall.
Ultrasonic
An ultrasound examination of the abdomen may help to rule out other possible causes of abdominal pain. Thus, the pain can also emanate from other abdominal organs such as the liver or gallbladder. However, to be able to assess the condition of the stomach and duodenum more accurately, a gastroscopy is necessary.
gastroscopy
The gastroscopy (gastroscopy) serves to ensure the diagnosis “gastric ulcer”. It helps a flexible hose, at the front end of a light source and a small optics are installed. This endoscope is gently advanced over the mouth and esophagus into the stomach and to the duodenum. This allows the doctor to directly assess any changes in the mucous membrane.
tissue Collection
During gastroscopy, the doctor can take tissue samples (biopsies) from suspicious mucosal sites via the endoscope. They are examined microscopically in the laboratory. In this way, it can be ascertained whether the mucosal lesions really are a stomach ulcer and not stomach cancer. In addition, a colonization with the gastric germ Helicobacter pylori can be detected on the basis of the tissue samples.
13C breath test
Another method for detecting Helicobacter pylori infection is a special breath test. The patient drinks a special solution with labeled 13C urea. If Helicobacter bacteria live in the stomach, they split up the urea. As a result, 13C-labeled carbon dioxide can be detected in the exhaled air.
Gastric ulcer: disease course and prognosis
If you treat a gastric ulcer consistently early with medication and maintain a stomach-friendly lifestyle, the ulcer usually heals easily and without complications. A stomach-friendly lifestyle includes abstaining as completely as possible from alcohol, nicotine and caffeine, from eating stomach-irritating (because it is very hot or spicy) food and largely avoiding stress.
If complications such as bleeding or a stomach wall breakthrough occur, healing usually takes much longer.
Gastric ulcer: prevention
You can do a lot yourself to prevent a stomach ulcer. This is especially important if you have ever had a stomach ulcer.
For example, pay attention to your diet: Avoid very hot and spicy foods because they irritate the stomach lining. For the same reason you should be careful with alcohol and coffee – in some people, the stomach reacts to small amounts of stimulants irritated, in which case a complete renunciation is advisable. Other people can tolerate at least an occasional glass of wine or a cup of coffee quite well.
To prevent gastric ulcers, you should also avoid stress as much as possible. Make sure you have regular relaxation periods in everyday life, such as walks, gardening, meditation or yoga. Try out what makes you relax.
Some people need to take regular medications that damage and stomach the stomach stomach ulcer can cause. Then you should talk to the attending physician, if possible, a reduction in the dose or a switch to a better tolerated drug is possible.
Additional information
guidelines:
- Guideline “Helicobacter pylori and gastroduodenal ulcer disease” of the German Society for Gastroenterology, Digestive and Metabolic Diseases (2016)