In heart failure (heart failure, heart failure, myocardial insufficiency), the heart is no longer able to provide the body with sufficient blood and oxygen. The disease is one of the leading causes of death in Germany. Read all about this topic: What is heart failure? What causes can she have? Which symptoms occur? How is the heart failure diagnosed and treated?

Heart failure: short overview
- Causes: Heart muscle diseases, heart valve defects, high blood pressure, constriction of the coronary arteries (coronary heart disease), chronic lung diseases, heart valve defects, liver cirrhosis, drug side effect
- symptoms: respiratory distress (dyspnea) during exercise or at rest, pale or blue discoloration of the lips and nail beds, edema v.a. on ankles and lower legs, rapid weight gain, nocturnal urination, palpitations, cardiac arrhythmia, low blood pressure
- diagnosis: körperl. Examination, blood pressure measurement, interception of heart and lungs, cardiac ultrasound, chest X-ray, ECG / long-term ECG, cardiac catheter
- Treatment: Antihypertensives, diuretics, slowing down of the heartbeat (e.g., beta-blockers), and fortifying the heart (e.g., digitalis). Depending on the cause surgery (for example, the heart valves, bypass, cardiac pacemaker), sometimes heart transplantation
Heart failure: causes and risk factors
In heart failure (heart failure), the heart is no longer as powerful as a healthy heart. It can no longer sufficiently supply the tissue of the body with blood (and therefore oxygen). That can be life threatening. Heart failure can be due to several causes:
The most common cause of heart failure is calcification of the coronary arteries (Coronary heart disease, CHD). This calcification causes the vessels that supply the heart muscle to contract. As a result, the heart muscle is undersupplied and is not as powerful.
The second main cause applies High blood pressure (hypertension), In hypertension, the heart has to pump more permanently. For a long time, however, it does not endure this load – the pumping power decreases.
Other heart failure causes are Arrhythmia and Myocarditis, Also Defects of the heart septum and Valvular heart disease (congenital or acquired) can lead to heart failure. The same applies to fluid accumulation in the pericardium (pericardium effusion or pericardial effusion).
Cause of heart failure can also Cardiomyopathies (Cardiomyopathy). These in turn can be caused by infection or excessive alcohol, drug or drug abuse. A special case is the so-called stress cardiomyopathy. It comes after a serious traumatic event suddenly to a life-threatening heart failure. After some time, the heart function normalizes but usually again. So there is no lasting heart failure. Life expectancy and quality of life are therefore not impaired after a surviving stress cardiomyopathy.
Metabolic diseases may also play a role in the development of heart failure. Examples are diabetes mellitus (diabetes) as well as disorders of thyroid function (such as thyrotoxicosis = excess of thyroid hormones).
Diseases of the lung such as pulmonary emphysema or COPD are other potential heart failure causes. In particular, the rare right ventricular failure (dysfunction of the right half of the heart) may be due to a lung disease.
In some people, heart failure develops as a result of anemia (Anemia), one cirrhosis or one AV fistula (AV-shunt). The latter is an abnormal shorting connection between an artery and a vein.
Sometimes cause too drugs a heart failure. This risk exists, for example, in certain remedies for cardiac arrhythmias, certain anticancer drugs (antineoplastic agents), appetite suppressants and migraine medications (such as ergotamine).
Systolic and diastolic heart failure
Heart failure is generally composed of two parameters: systolic and diastolic heart failure.
The term systolic heart failure (also known as congestive heart failure) refers to the reduced pumping capacity of the heart: the pumping function and the output of the left ventricle (ventricle) are reduced. As a result, the organs are no longer adequately supplied with blood.
However, heart failure is described inadequately. In addition to systolic heart failure, diastolic heart failure usually occurs. This means that the heart chambers are no longer adequately filled with blood. Mostly the left ventricle is enlarged morbidly and can not be sufficiently filled. As a result, less blood is then transferred to the systemic circulation. This leads to an undersupply of the body with oxygen. Diastolic heart failure occurs especially in old age. Women are affected more often than men.
Diastolic and systolic heart failure each have different causes and differ in heart failure therapy and prognosis.
Heart failure: classification
Heart failure can be classified according to various criteria:
- Depending on the affected heart area, a distinction is made between Left Heart Failure, Right Heart Failure and Global Heart Failure (both halves of the heart affected).
- Depending on the course of the disease, a distinction is made between acute heart failure and chronic heart failure.
- A rough classification according to the severity of the disease is in Compensated Heart Failure and Decompensated Heart Failure.
- A more accurate severity classification provides the NYHA classification of heart failure.
Heart failure: Left, right, global
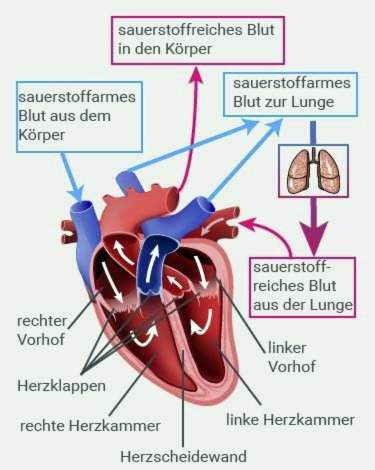
In the right heart failure Above all, the right atrium and the right ventricle of the heart muscle are affected by heart failure. The right side of the heart is the side into which the oxygen-depleted blood is first passed out of the body before being transported further into the lungs to “fill up” with new oxygen there. The enriched blood then flows into the left half of the heart and from there into the systemic circulation.
A disease-induced increased pressure in the lungs leads to a backflow in the blood flow: The right ventricle then has to pump the blood into the lungs with more force. Over time, the heart becomes overloaded and damaged (lung heart / cor pulmonale). Excessive stress causes the muscle layer in the wall of the right ventricle to thicken.
If the right half of the heart can no longer muster the additional power, the blood in the supplying vessels (veins) will back up. The increased pressure in the veins leads to water retention (edema) in the body, especially in the legs and in the abdomen.
Right heart failure usually develops as a result of chronic left ventricular failure.
In the left ventricular failure the pumping power of the left half of the heart is no longer sufficient. As a result, the blood builds up in the pulmonary vessels (congestion lung). This is especially dangerous as it can lead to fluid retention in the lungs (pulmonary edema). Cough and shortness of breath are typical symptoms.
When a global heart failure is present, the pumping power of both parts of the heart is reduced. So there are symptoms of right and left heart failure.
Acute heart failure and chronic heart failure
In acute heart failure first symptoms appear very quickly within a few hours to a few days. Causes are usually other diseases. Chronic heart failure develops slowly over several months to years.
Compensated and decompensated heart failure
The terms compensated heart failure and decompensated heart failure describe in which cases symptoms occur. The compensated heart failure triggers symptoms only under stress. At rest, the heart can provide the required performance, so there are no complaints.
In contrast, congestive heart failure causes symptoms such as fluid retention (edema) or shortness of breath (dyspnea) already at rest or at low stress such as climbing stairs.
Heart failure: NYHA classification
The NYHA (New York Heart Association) has created a common classification of heart failure for the observable symptoms:
- NYHA I: No physical symptoms at rest or during everyday stress.
- NYHA II: Slight restrictions on exercise capacity, but no symptoms at rest.
- NYHA III: Even with everyday physical stress high restrictions. Complaints such as fatigue, cardiac arrhythmia, shortness of breath and “chest tightness” (angina pectoris) occur even at low load quickly.
- NYHA IV: Symptoms manifest with every physical exercise and at rest. Those affected are usually immobile (bedridden) and depend on permanent help in their daily lives.
Heart failure: symptoms
Heart failure: symptoms of left heart failure
The left part of the heart is the part into which the blood that has been oxygenated in the lungs is transmitted. When this half of the heart stops functioning properly, the blood builds up in the lungs. this leads to to cough up to difficulty in breathing (Dyspnea). In most cases, respiratory distress initially occurs only during exercise (stressful dyspnea) and only later at rest (resting dyspnoea). In many cases, it makes itself noticeable at night.
Heart failure symptoms with “asthma cardiale”
As left heart failure progresses, fluid from the pulmonary capillaries passes into the alveoli. This so-called transudate leads not only to respiratory distress but also to increased coughing. At the same time, the bronchi can cramp. One also calls this symptom complex “Asthma cardiale“(” cardiac asthma “).
If fluid continues to pass into the alveoli, a so-called pulmonary edema, His hallmarks are severe shortness of breath and “blasige” secondary breath sounds. Due to the lack of oxygen, skin and mucous membranes turn bluish (cyanosis). In some patients, frothy, partly flesh-colored nasal secretions are also potential heart failure symptoms.
Heart failure patients usually become instinctive due to respiratory problems upright and elevated upper body out. This relieves the symptoms. In addition, the breathing aid muscles can be used more effectively in this attitude.
Heart failure: Symptoms of right heart failure
The oxygenated blood from the body flows into the right part of the heart. It is pumped from the right ventricle into the lungs, where it is re-oxygenated. When the right half of the heart is affected by heart failure, the butt plumps back into the body veins. Typical heart failure symptoms in this case are water retention in the body (edema). They usually show up first in the legs (leg edema) – especially on the ankles or on the back of the foot, then over the shins. In bedridden patients, the edema usually first forms above the sacrum.
In the advanced stage of right heart failure, water retention also occurs in the organs. As a result, the abdominal organs swell, and the waist circumference can increase. Other typical symptoms of cardiac insufficiency include impaired organ functions. In addition, fluid can accumulate in the abdominal cavity (Ascites, Ascites).
Water retention often causes one rapid weight gain, often more than two kilos a week.
These swellings can dry out the skin because the pressure in the tissue becomes too great. Possible consequences are Inflammations (eczema)that are too open, badly healing wounds can develop.
Global Heart Failure: Symptoms
If both halves of the heart are affected by organ weakness, it is called global heart failure. Symptoms of both forms of disease (right and left heart failure) then occur together.
Other heart failure symptoms
Heart failure usually causes water retention (edema) throughout the body, regardless of the affected heart area. These are resolved (mobilized) especially at night when the person is lying. The body wants to excrete the released, excess fluid through the kidneys. Therefore, people have to go to the bathroom very often at night. This heaped nocturnal urinals is called nocturia.
Especially in advanced stages of heart failure it comes to a disturbed breathing, The most common form is the so-called Cheyne-Stokes respiration. This can be recognized by the fact that the breathing depth and thus also the breathing noise periodically increase and decrease.
When loaded, the heart beats very fast (palpitations = Tachycardia). In addition, you can Arrhythmia occur, especially in the advanced stage of heart failure. The arrhythmias can be life-threatening and must be treated immediately.
Another classic late stage cardiac insufficiency is low blood pressure.
Common and very common heart failure symptoms are as well reduced efficiency, fatigue and exhaustion.
Heart failure: examinations and diagnosis
The heart failure diagnosis is based on the registration of the medical history (anamnesis) and the physical examination (including physical examinations).
in the anamneseAmong other things, the doctor asks the patient about his symptoms and whether heart diseases have already occurred in the family (genetic predisposition).
In the physical examination There are various options that are different consuming and meaningful. In addition, the physical examination is used to rule out other diseases that also cause heart failure symptoms such as shortness of breath and chest pain (differential diagnosis).
The monitor Cardiac activity with the stethoscope provides the physician with first indications of heart valve failure or myocardial insufficiency. Listening to the lungs, a rattling sound is a sign of heart failure. It indicates water retention in the lungs.
When edema in the legs can be visible in the ankle region dents push into the skin.
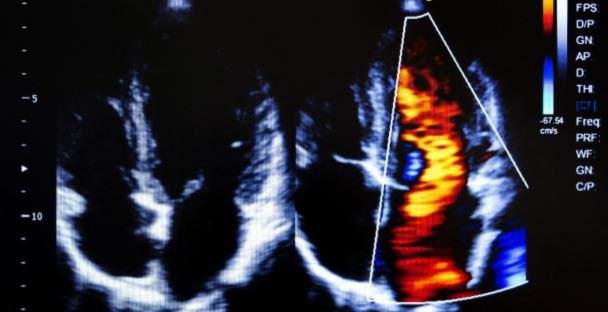
The function of the heart can be combined with a Cardiovascular Ultrasound (Echocardiography). The doctor can see if there are any defects on the valves, on the structure of the heart walls or in the heart interiors. Also, a thickened wall structure and the ejection performance of the heart are made visible.
The bloodstream that flows through the heart can be controlled using the Color Doppler sonography to make visible. This is a special form of ultrasound examination.
Cardiac arrhythmias are combined with a Holter best proved. In doing so, the person concerned gets a portable small device. It is connected to the electrodes that the doctor attaches to the patient’s left chest and continuously records heart activity. Such a long-term ECG usually runs over 24 hours. The examination is painless and does not affect the patient.
With a Cardiac catheterization can be determined whether the coronary arteries are narrowed. The examination usually takes place under local anesthesia. If narrow spots are discovered, they can be stretched immediately. Under certain circumstances, stents (stents) are used to keep a constricted coronary vessel permanently open.
Also one Blood pressure measurement is performed in case of suspected heart failure. Besides, the doctor arranges different Urine and blood tests in the laboratory: The urine status and a blood picture are made. The content of the electrolytes sodium and potassium in the blood is determined. Also measured are creatinine, fasting blood sugar, liver enzymes and the value of the B-natu- ruretic peptide (BNP). Heart failure leads to an increase in BNP levels. This is directly related to the classification of heart failure into a stage of the NYHA Association (see below).
These examinations can be used to detect disorders of the liver, kidney or thyroid gland. Increased blood lipid levels and diabetes mellitus can also be diagnosed.
In addition, you can radiographs of the ribcage and one magnetic Resonance Imaging (MRT) support heart failure diagnosis.
Heart failure: treatment
Heart failure therapy consists of several components and depends mainly on the severity of heart failure. Basically, in addition to a drug therapy and the personal lifestyle is crucial. In severe cases, a pacemaker or a heart transplant may be necessary.
In general, heart failure is a progressive disease that often leads to death. The therapy guidelines of international specialist societies therefore recommend palliative care for all patients. This includes, on the one hand, the alleviation of symptoms (such as medication or surgery). On the other hand, there is an intensive communication between doctor and patient: Everything important about diagnosis, therapy, course and prognosis of the disease should be discussed together. Also, precautionary powers and living wills should be taken care of. This makes it easier for the patient and his relatives to deal with the disease.
Heart failure: medication
With the medicamentous heart failure therapy one wants to prevent complications of the illness and to improve the quality of life of the patients. Depending on the cause of heart failure, different medicines are used. Some medications have been shown to improve prognosis, while others alleviate existing symptoms.
Very often in the heart failure therapy agents from the group of ACE inhibitors and beta-blockers are used. They are life-prolonging, according to recent studies. However, for these and other drugs to really work, they must be taken permanently and regularly as prescribed by the doctor.
Overall, various drugs are available for heart failure therapy. The most important ones are:
- ACE inhibitors: They block a protein that is responsible in the body for the constriction of the blood vessels. As a result, the blood vessels remain permanently enlarged, and the blood pressure drops. This relieves the heart, and the heart muscle remodeling as a result of continuous overload is slowed down.
- AT1 antagonists: They block the effect of a blood pressure-increasing hormone. They are only used if the patient does not tolerate ACE inhibitors.
- Beta blocker (beta receptor blocker):They prevent life-threatening cardiac arrhythmias and thus improve the prognosis for heart failure.
- Mineralocorticoid Receptor Antagonists (MRA): They increase the excretion of water from the body, which ultimately relieves the heart.
- Sacubitril / valsartan: This drug combination is prescribed only in certain cases of chronic heart failure. Sacubtril inhibits the breakdown of hormones in the body, which dilate the vessels. Valsartan abolishes the effect of the hypertensive hormone angiotensin.
- ivabradine: This drug lowers the heart rate.
- Digitalis: Preparations with digitalis improve the pumping power of the heart. It does not prolong life, but increases the quality of life and resilience of those affected. It also serves to control the frequency of atrial fibrillation, a common form of cardiac arrhythmia.
- diuretics: Diuretics are diuretic drugs. They exude stored fluid, so that the heart and vessels are less stressed.
Every drug can also have side effects. A common side effect of ACE inhibitors, for example, is irritating cough. This is usually harmless. AT1 antagonists and diuretics can mess up the blood salt balance, and beta blockers can slow down the heartbeat. If heart failure suffers from medication side effects, they should inform their doctor about it. This can adjust the dosage or possibly even prescribe another preparation.
Hawthorn in heart failure
The herbal medicine recommends for heart failure hawthorn-Preparations. They are intended to improve the contraction force and oxygen supply of the heart muscle. In addition, they counteract cardiac arrhythmia (antiarrhythmic effect). From a scientific point of view, no relevant and proven efficacy of hawthorn in cardiac insufficiency has yet been demonstrated. If patients still want to try such medicinal plant preparations, then in consultation with the doctor or pharmacist and in addition to conventional medical heart failure treatment.

Pacemaker against heart failure
In people with advanced heart failure, a so-called biventricular pacemaker(CRT = Cardiac Resynchronization Therapy) combined with drug therapy. Both together can balance the heart failure.
Patients who have survived a cardiac arrest or suffer from dangerous cardiac arrhythmias benefit from one implantable defibrillator (implantable cardioverter / defibrillator, ICD), The device is used like a pacemaker. It gives off an electric shock when it detects a dangerous arrhythmia.
Sometimes doctors also use a combination device from both systems, the so-called CRT-ICD System.
Surgical measures
If heart failure deteriorates despite existing therapy, it may be necessary to replace the old one with a new one (heart transplant). Patients can receive a donor heart or an artificial heart. This can lead to various complications such as rejection reactions.
Narrowed coronary arteries (coronary heart disease, CHD) are among the most common causes of heart failure. The impaired blood flow can be surgically improved by widening the vessels (balloon, possibly with installation of a stent = vascular support). You can also do one bypass lay.
If defective heart valves are the cause of heart failure, surgery may also be necessary. Sometimes a “repair” (Reconstruction) of the heart valve possible. In other cases, the defective heart valve is replaced (biological or mechanical Prosthetic valve).
Heart failure: what you can do yourself
If the doctor has found you heart failure, you should definitely pay attention to a healthy lifestyle. Risk factors are thus minimized and the quality of life increased. You should therefore heed the following:
- Nutrition: Look for a diet with enough fruits and vegetables. If possible, avoid animal fats and eat low in salt. Salt ensures that water is stored in the body. The heart then has to work harder.
- Hydration: The amount of daily fluid intake should be discussed with your doctor. As a general rule, you should not drink three or more liters a day if you have heart failure. Ideally, in most cases, a fluid intake of 1.5 to two liters per day.
- Move: In any case, effective heart failure therapy requires exercise and moderate physical activity. In everyday life, for example, you can walk to work and take the stairs instead of the elevator. Even walks, light strength and coordination exercises, swimming, cycling and walking are recommended. You can also join a sports group for cardiac patients (rehab sport). Discuss with your doctor which physical activities and sports are appropriate in your case and to what extent you are allowed to exercise.
- Body weight: Obesity has a negative effect on cardiac insufficiency. From a body mass index (BMI) over 40, the weight should be reduced. The weight loss should be controlled and slow and definitely under the supervision of a doctor. Also normal-weight heart failure patients should regularly control their weight, preferably daily. A very fast and big weight gain can be an indication of water retention in the body. Rule of thumb: If you gain more than one kilo per night, over two kilos in three nights, or more than two pounds in a week, you must go to the doctor.
- Alcohol: Minimize your alcohol intake, because alcohol can damage the heart muscle cells. Women are advised to consume no more than twelve grams of pure alcohol per day (a standard drink). Men should not consume more than 24 grams of pure alcohol (equivalent to two standard drinks) per day. Patients whose heart failure was caused by excessive consumption of alcohol (alcoholic cardiomyopathy) should abstain completely from alcohol.
- Smoke: It is best to stop smoking completely!
- Vaccination: Get regular vaccinations every year against the flu and every six years against pneumococci.
- Diary: Keep a journal of any complaints you notice. So you can not forget anything at your next visit to the doctor.
Heart failure: disease course and prognosis
Heart failure is not curable. Only in the rarest of cases can the symptoms be reduced to such an extent that completely undisturbed life is possible. However, each patient can influence themselves whether and how far the disease progresses. By a change of lifestyle and one conscious dealing with the disease sufferers can do a lot to improve their prognosis.
In addition to the lifestyle, it is above all the Compliancethat patients need to pay attention to. With compliance or compliance, the doctor describes the extent to which patients comply with the prescribed and discussed therapy. This includes, for example, that the prescribed medications are taken regularly, even if at present may be no symptoms. Complications and deterioration of the general condition can thus be prevented in advance.
Compliance also means that the check-ups at the family doctor are regularly performed. In particular, the blood concentrations of sodium and potassium as well as the kidney values are tested. If these values are outside the normal range, more frequent controls are needed.
Also important in heart failure: Immediately check with the doctor for any suspicion that your condition has worsened!
Heart failure: life expectancy
Statistically, half of all patients die within five years of the diagnosis of “heart failure.” Life expectancy and quality of life of patients have risen in recent years, however, due to the ever better medical care. Thus, sufferers often have a good prognosis and, despite illness, a relatively high life expectancy. In individual cases, this depends on the type (genesis) of the disease, the age of the person concerned, possible comorbidities and the personal lifestyle.
Death certificates often indicate “heart failure” as the cause of death. This is the acute one heart failure meant, which in many cases leads to death.
Additional information
Book recommendations:
- Special volume on the heart failure of the German Heart Foundation
guidelines:
- Pocket Guidlines “Heart Failure” of the German Society of Cardiology (as of 2016)
- National Care Guideline “Chronic Heart Failure” of the Association of Scientific Medical Societies (AWMF) et al. (As of 2017)