Pancreatitis can be acute or chronic. Acute inflammation is triggered by gallstones in most patients. It causes the gland to “digest itself” to a certain extent. The typical symptom of acute pancreatitis is belt-shaped upper abdominal pain radiating to the back. Read more about symptoms, causes, diagnosis and treatment of pancreatitis!

Quick Overview
- Definition: acute or chronic inflammation of the pancreas (abdominal gland, which produces digestive enzymes and important hormones)
- symptoms: Acute pancreatitis: severe upper abdominal pain that can radiate into the back; in addition, rubber belly, nausea and vomiting, fever, jaundice, bluish skin discoloration. Chronic pancreatitis: weight loss, digestive problems, fatigue, gait disturbances, night blindness, bleeding tendency etc.
- Causes: In acute pancreatitis mostly gallstones or alcohol consumption, more rarely drugs, infections etc .. The trigger of chronic pancreatitis is usually regular alcohol consumption. Rarer causes include metabolic diseases or genetic defects.
- investigations: Patient interview (anamnesis), physical examination, blood test (pancreatic enzymes, calcium, gamma-GT, alkaline phosphatase, liver values, etc.), stool examination, imaging techniques (ultrasound, X-ray, possibly magnetic resonance imaging, computed tomography), bile resection (ERCP)
- Treatment: Acute pancreatitis: hydration, medication, short-term food abstinence, followed by light diet, possibly artificial diet, removal of existing gallstones; rarely an operation is necessary. Chronic pancreatitis: Lifelong alcohol abstinence, intake of digestive enzymes and vitamins, possibly Insulinabe, rarely surgery.
- Forecast: Depends on course (acute / chronic) and severity of inflammation.
Acute pancreatitis: symptoms
Sudden, severe pain in the upper abdomen are common signs of acute pancreatitis. Symptoms such as bloated stomach and nausea and vomiting are often added. However, the nature and extent of the symptoms depend on the severity of the inflammation and any consequences. In summary, in acute pancreatitis symptoms and complications of the following kind may occur:
- acute, severe upper abdominal pain: Sudden upper abdominal pain that radiates belt-shaped to the back or sometimes in another direction and can last for several days. Gallstones are the trigger of acute pancreatitis, the pain can be colicky (ie wave-like increase and decrease).
- Nausea and vomiting: The upper abdominal pain in acute pancreatitis is usually accompanied by nausea and vomiting.
- Flatulence and bloated abdomen: In acute pancreatitis, the belly is often inflated gummy (“rubber belly”) and sensitive to pressure.
- facial flushing
- Fever and weakness: Temperatures above 38 ° C are a defense mechanism of the body, which occurs in the context of inflammatory reactions. Often the blood pressure is very low. Both result in the patient feeling tired and tired.
- Circulatory problems: Released inflammatory substances cause the vessel walls to become more permeable. This allows fluid to escape more easily into the surrounding tissue. This lowers the blood pressure, which can cause circulatory problems. Maybe even a circulatory shock occurs!
- Water accumulation in the stomach and lungs: As a result of acute pancreatitis, fluid may accumulate in the abdominal cavity (ascites, ascites) or between the lungs and chest wall (pleural effusion).
- Bluish skin discoloration: In severe acute pancreatitis, sometimes bluish greenish spots (bruises) around the navel (Cullen sign) or on the side flanks (Gray Turner sign). They are caused by small bleeding in the superficial fatty tissue. This symptom is considered an unfavorable sign for the further course of acute pancreatitis.
- Jaundice (jaundice): Most of the acute pancreatitis is due to a gall disease. If this organ stops functioning properly, bilirubin, a breakdown product of red blood pigment (hemoglobin), remains in the body and deposits in various places. The first thing that counts is the sclera, that is, the whites in the eye, that subsequently discolouredly bleaches. Later, the bilirubin settles in the skin and mucous membranes, which also assume a yellowing.
Acute pancreatitis: causes and risk factors
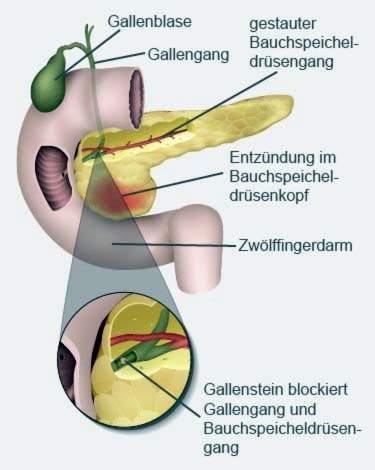
Acute pancreatitis is prevalent in about 45 percent of cases gallstones caused (biliary pancreatitis): The bile (produced in the liver and stored in the gallbladder) and the digestive secretions from the pancreas (pancreatic juice) usually flow through a common passage in the small intestine. If this gait is blocked by gallstones, the pancreatic juice backs up into the pancreas (and the bile in the direction of the liver). The digestive enzymes, which are contained in the jammed pancreatic juice, are then active in the pancreas instead of as planned only in the intestine. They attack the glandular tissue, causing the pancreas to self-digest (proteolytic autodigestion). The damaged tissue invokes the immune system and causes an inflammatory reaction.
alcohol is the second leading cause of acute pancreatitis. He is responsible for around 35 percent of all illnesses. Alcohol attacks the pancreatic tissue directly, causing an inflammatory reaction.
In order to get an acute pancreatitis, an alcohol excess is not necessarily necessary. Some people already respond to a relatively moderate amount of alcohol with a pancreatitis.
Rarer causes of acute pancreatitis (about 15 percent of all cases) are:
- Viral infections such as mumps, HIV, viral hepatitis
- certain medications such as dehydrators, antihypertensives, hormones
- greatly increased calcium levels, e.g. in hyperfunction of the parathyroid gland
- high blood lipid levels (> 1000 mg / dl)
- Mirroring of the biliary system (ERCP), abdominal injury or surgery
- Inheritance (hereditary pancratitis)
- anatomical features
In about 15 percent of those affected, no cause for the pancreatitis can be found. Doctors call this one idiopathic pancreatitis.
Chronic pancreatitis
In contrast to acute pancreatitis, chronic pancreatitis is one recurrent inflammation of the pancreas, In 70 to 80 percent of cases, the trigger is regular alcohol consumption. At the same time, people react differently sensitively to the pleasure poison: sometimes even small amounts of alcohol suffice for a chronic inflammation of the pancreas.
The disease often begins creeping with mild to moderate discomfort. Belt-shaped upper abdominal pain is – as in acute pancreatitis – a typical symptom. Often they wake up after eating. Other common signs of chronic pancreatitis include weight loss, indigestion, nausea, vomiting and a greasy, foul-smelling stool (fat stool).
For more information on the causes, symptoms, treatment and consequences of a chronic inflamed pancreas, see Chronic pancreatitis.
Acute pancreatitis: examinations and diagnosis
If you develop any signs of (acute) pancreatitis, you should go to the family doctor or directly to a specialist in internal medicine and gastroenterology. If the symptoms occur outside office hours, it is advisable to visit a hospital. Especially with strong complaints you should not hesitate to get medical help! Above all, an acute pancreatitis can be not only very painful, but under certain circumstances also life-threatening.
Survey of the medical history
First the doctor will ask you about your complaints. He will also inquire about possible triggers of pancreatitis. Typical questions in this anamnesis interview are:
- Do you have a fever or are you sick?
- Did the symptoms occur suddenly? Or do you appear on specific occasions?
- Are you familiar with gallstones?
- Have you taken any medications and, if so, which ones?
- Did you drink a lot of alcohol before the symptoms started or do you drink alcohol regularly?
- Did a blood test give you elevated blood lipid or calcium levels?
- Does her chair shine greasy?
Physical examination
After the interview follows a physical examination. The doctor will ask you to clear the stomach. So the doctor can check if you have an elastic and tightly stretched “rubber belly” – a common sign of acute pancreatitis. In addition, the stomach is often very sensitive to pain. Patients often angle their legs to relieve pain.
During the physical examination, the doctor also looks for bruising in the lateral flanks and around the navel and checks whether the whites of the eyes and the skin have turned yellow.
blood tests
Certain blood levels help to rule out or confirm an (acute) pancreatitis: Pancreatic pancreatic enzymes, for example, have elevated levels of pancreatic enzymes Lipase and alpha-amylase detectable. However, increased enzyme levels may have other causes, so they are not proof of pancreatitis.
Other blood counts that are detected in suspected pancreatitis are blood sugar, Kidney and liver values, Also the Calcium level is measured: Increased calcium levels may be the cause of acute pancreatitis.
Increased values for Gamma-GT and alkaline phosphatase (AP) may indicate bile dew.
Furthermore, the doctor can inflammatory markers measure like the C-reactive protein (CRP). If it is elevated, it generally speaks of inflammation in the body. In addition, the CRP value is suitable for the follow-up of acute pancreatitis.
Imaging procedures
To safely diagnose pancreatitis, the doctor must examine the abdomen with an imaging technique. The simplest and fastest method is one Ultrasound (Sonography). This is often used to detect gallstones, which are the most common cause of acute pancreatitis. In addition, the doctor can ultrasonically assess the extent of inflammation and discover disease-related changes. This can be a swelling of the pancreas, dead tissue and accumulation of water in the stomach and lungs.
If the ultrasound findings are not clear, one can MRI (Magnetic resonance imaging, MRI) or a Computed tomography (CT) bring clarity. Both methods provide very detailed images of the examined tissue. They are also used in severe pancreatitis.
By means of a X-ray The doctor can check the function of the lungs and intestines. Water retention between the lungs and the chest wall as well as in the abdomen can be easily recognized on the x-ray. Also visible are possible air bubbles in a paralyzed intestine.
Endoscopic examination
If bile ducts are suspected to be blocked by gallstones or a tumor in the region of the bile ducts, the doctor can perform a bile reflex: more precisely, it is a reflection of the pancreas, bile duct and gallbladder. The medical term for this endoscopic examination is endoscopic retrograde cholangiopancreatography (ERCP).
By means of ERCP, discovered gallstones can usually be removed as well.
stool examination
If a suspected chronic pancreatitis is suspected, the physician may send a patient’s stool sample to the laboratory for analysis. There is the content of the pancreatic enzyme elastase measured, which is normally excreted unchanged with the stool. In tissue damage (due to chronic pancreatitis, for example) less elastase gets into the small intestine and into the stool. Then the elastase concentration in the feces is unusually low.
Since some illnesses can cause symptoms similar to a pancreatitis, the doctor must exclude these in the diagnosis. These diseases include, for example, myocardial infarction, appendicitis, biliary and renal colic, ectopic pregnancy and pulmonary embolism.
Acute pancreatitis: treatment
Acute pancreatitis is potentially life-threatening. Patients must therefore be treated in the hospital, in severe cases even in intensive care. Sufficient hydration and appropriate pain therapy are important building blocks of treatment. In addition, the diet must be adjusted for pancreatitis. In certain circumstances
Pancreatitis – fluid administration
In patients with pancreatitis, much fluid from the blood vessels enters the tissues. As a result, there is a lack of fluid in the blood vessels. The blood pressure drops, possibly to the cycle failure by a shock. The patients therefore receive sufficient liquid by infusion. If they are also lacking in blood salts (electrolytes), these are also supplied with the infusion.
Pancreatitis – medicines
Painkillers and anti-spasmodic drugs help against the strong, often spasmodic pain. In severe acute pancreatitis patients often get antibiotics: This is to prevent a bacterial infection of the inflamed pancreas or fight early. In acute pancreatitis, blood clots (thrombosis) may develop in some cases, which is why doctors use the anticoagulant heparin as a precautionary measure.
Pancreatitis – nutrition
Patients should not eat for several days to relieve the pancreas. This is especially true when nausea and vomiting occur. Especially in cases of severe acute pancreatitis and complications, those affected are supplied with necessary nutrients via infusions (parenteral nutrition). Sometimes a small bowel probe is placed later: The doctor carefully guides a thin tube over the patient’s nose or mouth through the esophagus and stomach to the small intestine. Through this probe, nutrients can be routed directly into the intestine.
As soon as the patient is allowed to take food again, start with a light diet (rusk, rice pudding, tea, etc.). Fatty food is allowed again only after two to three weeks and then only in small quantities for the time being. Alcohol is taboo. More detailed tips on nutrition in pancreatitis gives the treating physician. He may also recommend to the patient to temporarily take enzyme preparations that aid digestion.
Removal of gallstones
Gallstones are the cause of acute pancreatitis (bilateral pancreatitis), these are usually removed endoscopically using ERCP. Larger stones are first crushed with shock waves (shock wave therapy).
surgery
Severe acute pancreatitis sometimes requires surgery. Especially if inflammation caused a lot of pancreatic tissue is dead (necrotizing pancreatitis), you have to cut this out.
Acute pancreatitis: course and prognosis
If no complications occur, the prognosis for acute pancreatitis is usually good. Properly treated, approximately 80 percent of patients will recover after approximately one to two weeks. In about 20 percent of the cases, serious consequences develop. The healing process can then take weeks or months. In severe acute pancreatitis, approximately 15 percent of those affected die.
Gauge Ranson score
In order to better estimate the prognosis for acute pancreatitis in individual cases, physicians use the so-called Ranson score. Various clinical parameters and laboratory values are assessed within the first 48 hours after the patient has been admitted to the clinic:
|
When admitted to the hospital |
||
|
Age |
> 55 years |
1 point |
|
White blood cells (leukocytes) |
> 16000 per mm3 |
1 point |
|
Lactate dehydrogenase (LDH) |
> 350 U / liter |
1 point |
|
Aspartate aminotransferase (ASAT) |
> 250 U / liter |
1 point |
|
glucose |
> 11.1 millimoles per liter or> 200 milligrams per deciliter |
1 point |
|
48 hours after admission to the hospital |
||
|
Hematocrit drop |
> ten percent |
1 point |
|
Urea increase |
> 1.8 millimoles per liter |
1 point |
|
Calcium value in the serum |
<2 millimoles per liter |
1 point |
|
Arterial oxygen partial pressure |
<60 mm Hg |
1 point |
|
Base deficit in the blood |
> 4 mEql |
1 point |
|
Fluid loss from the vasculature into the tissue |
> 6 liters in 48 hours |
1 point |
For each applicable criterion, one point is awarded in the Ranson score. The higher the score, the greater the risk that acute pancreatitis will be fatal (mortality forecast).
Possible complications
If the acute pancreatitis is not treated, it can cause complications anywhere in the body:
Volume-loss shock (hypovolemic shock): The blood vessels become more permeable as a result of inflammation. If too much fluid escapes into the surrounding tissue as a result, there is a dangerous lack of volume in the vascular system – the blood pressure can drop so much that the organs can no longer be adequately supplied with oxygen. The result is a hypovolemic shock.
Intestinal paralysis: Any inflammation in the service room can disrupt normal bowel movements. These can even come to a standstill, so that the porridge can no longer be transported. Then there is a life-threatening intestinal paralysis (paralytic intestinal obstruction)! Possible signs are severe pain and flatulence. In extreme cases, the patient vomits stool. An intestinal obstruction must always be treated as quickly as possible!
Pancreatic pseudocysts: After the onset of acute pancreatitis, fluid-filled cavities surrounded by collagen fibers and wound healing tissue may form in the pancreas. They are called pancreatic pseudocysts. Often, they remain small, do not trigger symptoms, and recover within a few weeks. Sometimes, however, they also cause symptoms such as stomach upset or feeling bloated. In addition, larger pseudocysts are at risk of tearing and bleeding or infecting and forming an abscess. To prevent this from happening, the fluid in larger pseudocysts will be sucked from the outside via a hollow needle (drainage). Sometimes an operation is necessary.
Necrotizing infectious pancreatitis: Rarely, acute pancreatitis develops into necrotizing infectious pancreatitis. That is, inflammation causes glandular tissue to die off (necrosis), and the dead tissue becomes infected with bacteria. This dangerous complication can become a so-called SIRS (systematic inflammatory response syndrome) It is characterized by a spread of inflammation to the whole body. Possible symptoms include high fever (sometimes a low temperature), fast heart rate and fast breathing. There is a danger that organs will fail!
Acute pancreatitis: prevention
It is usually the case that the acute pancreatitis came from nowhere. In fact, such a disease often leads to a long-term lifestyle. To prevent acute pancreatitis, you should therefore:
- eat low in fat
- drink little or no alcohol
- Treat diseases such as increased blood lipid levels or hyperparathyroidism
Especially people who have ever had an acute pancreatitis should heed these tips!
Additional information
guidelines:
- Guideline “Chronic Pancreatitis: Definition, Etiology, Diagnosis and Conservative, Interventional Endoscopic and Operative Therapy of Chronic Pancreatitis” of the German Society for Digestive and Metabolic Diseases (2012)
Self-help:
- Working group of pancreatectomized e.V.