Tuberculosis (TB) is a serious infectious disease caused by bacteria. The pathogens are usually transmitted through droplets in the breath, which are inhaled. Therefore, tuberculosis in most cases affects the lungs first. But it can also affect other organs such as the intestine or the bones. Read here what tuberculosis is, how to be infected, how to recognize it and what treatment options are available.

Tuberculosis Short overview
- Description: Reportable bacterial infectious disease. Affects mainly the lungs, but also bones, intestines and other organs
- Infection: Mostly by droplet infection via the lungs, but also via the digestive tract or skin injuries. Only one in ten people develops symptoms
- symptoms: Fever, coughing, night sweats, weight loss, fatigue, in the later stage bloody sputum
- Particularly at risk: People with a weak immune system, e.g. HIV patients, people taking immunosuppressants, homeless, malnourished, children, addiction patients
- Diagnosis: Antibody test on the skin, blood tests, x-rays, direct bacterial detection
- treatment: Special antibiotics, difficult treatment for resistant bacterial strains
- Forecast: In otherwise healthy patients, there are good chances of recovery if the disease is detected early.
Tuberculosis: description
Tuberculosis (TB, TB) is caused by rod-shaped bacteria called mycobacteria. It mainly affects the lungs, but can also affect other organs.
In most cases, the body succeeds in successfully controlling the pathogens or rendering them harmless by encapsulation. Only in about ten percent of cases does tuberculosis actually break out. Symptoms include fever, fatigue, night sweats and weight loss. Later also bloody cough and shortness of breath.
In the past, the disease was also referred to as consumption, because those without effective treatment lose their body very quickly.
Tuberculosis – that’s how you get involved
Tuberculosis was long considered nearly extinct in western industrialized countries. In recent years, the disease has become more common due to the inflow of sick people, for example from Eastern European countries.
How do the bacteria get into the body?
The tuberculosis transmission takes place via different routes:
Infection via the breath: By far the largest proportion of patients get infected when infectious microdroplets enter the lungs with the air they breathe. The bacteria are sneezed out or coughed up by patients with so-called open tuberculosis. Open tuberculosis means that the foci of infection in the lungs are not encapsulated, but open to the bronchi.
Infection via the digestive tract: The bacteria can also enter the body via the digestive tract. The causative agent of bovine tuberculosis, Mycobacterium bovis, for example, can be transmitted to humans through raw milk of diseased cows.
Infection via the skin: Another transmission pathway is skin injury, through which the tuberculosis pathogen enters the body.
How contagious is tuberculosis?
TBC is less contagious than other infectious diseases such as flu. Only one out of every ten infected people actually die of the disease. Whether one falls ill after the contact with an infected person depends above all on two factors:
- how many pathogens the patient has secreted
- how powerful your own immune system is
The tuberculosis incubation period can be weeks to months.
Tuberculosis: symptoms
The symptoms of tuberculosis and the symptoms that a tuberculosis patient suffers depend on the stage of the disease and the affected organs.
Latent tuberculosis
After a tuberculosis infection, patients often have no complaints. In fact, in most cases, the body manages to keep the bacteria in check. Then there are no symptoms of tuberculosis. This condition is called latent tuberculosis.
Closed tuberculosis
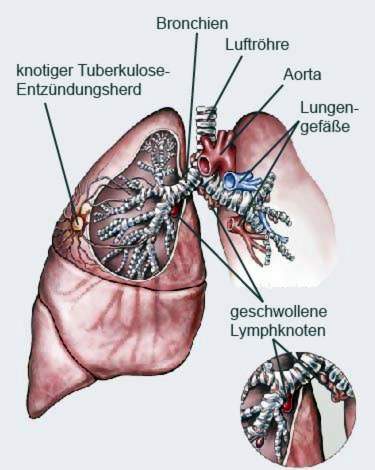
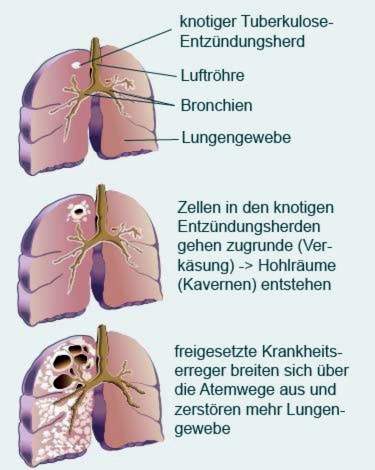
In people with good body defense form the defense cells around the inflammatory foci a kind of capsule. There are nodular structures called granulomas or tubercles. The pathogens may still be active in these tubercles, but do no harm to the body. Later, the tubercles increasingly scarred and calcified. You can often see them on x-ray pictures years later. This form of medicine is referred to as closed tuberculosis.
primary tuberculosis
In about five to ten percent of patients, the body’s immune system fails to successfully encapsulate the pathogen. Then inflammatory foci form in the lungs and the nearby lymph nodes. These enlarge. This condition is called primary tuberculosis. However, the process is slow: most of the time this stage begins within two years of infection.
The patients often do not notice this form of tuberculosis either. But it can also occur various complaints such as:
- fever
- to cough
- nocturnal sweats
- anorexia
- weight loss
- fatigue
- exhaustion
Open tuberculosis
If the infection spreads in the body, cavities, so-called caverns, form in the lung tissue. They are filled with dead cells and active tuberculosis bacteria (necrosis, caseation). When these cavities break through to the bronchi, it is called open tuberculosis.
Then typical tuberculosis symptoms occur: the patient coughs up phlegm, which can also be bloody. The pathogens then often reach the breathing air in large numbers. Patients with open tuberculosis are highly contagious.
Post-primary tuberculosis
Tuberculosis can persist in the body for a long time without causing symptoms. However, the disease can also start or re-emerge many years after the initial infection. Then one speaks of a postprimary tuberculosis.
In about 80 percent of cases, this affects the lungs. Sometimes, however, the pathogens also spread through the bloodstream. There are the smallest inflammations in other organs, so-called “minimal lesions”.
Most of these are pectoralis, lymph nodes, bones and joints. But also digestive tract, skin and genitals can be affected.
Tuberculosis outside the lung tissue
Even though they usually sit in the lungs, tuberculosis pathogens can infect organs and tissues throughout the body. There are quite different symptoms.
Lung root: There, where the bronchi enter the lungs (lung root, Lungenhilus), sit particularly many lymph nodes. When they are attacked by tuberculosis bacteria, they swell and compress the adjacent airways.
The underlying lung tissue is cut off from the air supply and collapses. If the ventilated lung area is large, the patient is noticeably suffering from shortness of breath.
Pleura: In cases of tuberculosis of the pleura (pleurisy tuberculosa), those affected usually have pain when breathing. In a “wet” pleurisy, liquid accumulates around the lungs, which can squeeze the lungs so much that respiratory distress arises.
miliary tuberculosis: Miliary tuberculosis is a TB infection that affects not only the lungs but also the meninges, liver, spleen, kidneys and eyes. This small, distributed throughout the organ, granules large inflammatory foci form. They are reminiscent of millet grains, Latin Milium. In Germany, this form is rare, but more often affects children or people with a weakened immune system.

The tuberculosis symptoms are then nonspecific. This means they can also be found in many other diseases and are not typical for tuberculosis. These include fever, headaches, a stiff neck and blurred vision.
Intestinal tuberculosis: With the intestinal tuberculosis, the patients are mainly infected by the consumption of infected raw cow’s milk.
In addition to flu-like symptoms, there are symptoms that are reminiscent of a chronic inflammatory bowel disease: diarrhea, abdominal pain and weight loss. Often there is also blood in the stool. In the further course of peritonitis or dangerous intestinal obstruction may occur.
Tuberculosis of the skin: An infection of the skin with tuberculosis pathogens may be expressed differently. The most common are flat, red-brown skin lesions. These are often hardened and clearly palpable. However, the patient has no pain. Doctors also speak of the disease in this disease picture Lupus vulgaris.
Tuberculosis of the urinary tract: If the urinary tract is affected by tuberculosis, inflamed nodules develop in the kidneys, ureters and bladder, which can scar and calcify.
Affected suffer from pain when urinating and in the flanks. You may find blood or pus in the urine. Through the nodules, the urinary tract can also close, so that the urine backlogs. The urinary organs can suffer permanent damage.
Tuberculosis of the sexual organs: In women, a tuberculosis infection of the genitalia usually migrates from the fallopian tubes to the uterus. Subsequently, the menstrual bleeding often stops and the woman can become infertile.
In men, the epididymis can be infested with tuberculosis bacteria. These swell painfully and are red. The disease can lead to infertility.
Bone and joint tuberculosis (tuberculosis spondylitis): A bone and joint tuberculosis manifests itself in swelling and pain in the joints, but especially in the thoracic and lumbar spine. The patients feel very ill.
If the inflammatory process of this tuberculosis continues untreated, abscesses develop. There are nerve failures with signs of paralysis in the affected areas. Often a round back is formed. In extreme cases, the spine bends backwards. These serious TB symptoms have become very rare thanks to good treatment options.
Tuberculosis: causes and risk factors
With more than 95 percent, Mycobacterium tuberculosis is the most common cause of tuberculosis in humans. The disease breaks out especially in people with weakened immune systems. This includes:
- HIV-infected, AIDS patients
- chronically ill (e.g., diabetics)
- Patients in whom the immune system is drug-suppressed (for example, after a transplant)
- Drug addicts, smokers and alcoholics
- older people
- Diabetics and patients with kidney failure
- homeless people
- Malnourished
- Infants and children under four years
Migrants from poorly-endowed countries are more likely to suffer from tuberculosis. In the cramped refugee camps, the risk of infection is particularly high. Even among prisoners Tbc is more widespread than in the rest of the population.
For both groups medical attention therefore focuses on a possible spread of TB.
Tuberculosis: diagnosis and examination
The signs of Tbc are only slightly characteristic (nonspecific). In about 15 percent of cases, no symptoms occur. The infection is therefore usually discovered by accident, for example, during a check-up at the family doctor or specialist in internal medicine.
Medical history (anamnesis)
If there is a suspicion of TB, the doctor will ask the patient about the symptoms that occur, for example:
- Do you have a slight fever?
- Do you sweat very much at night?
- Have you lost a lot of weight lately?
Other circumstances that make tuberculosis more likely:
- previous tuberculosis infection. In that case, dormant Tbc bacteria may have been reactivated in the body.
- Known TB cases in the vicinity, ie in the circle of relatives and friends or at work (especially in the medical field)
- Travel to countries with higher tuberculosis spread
- Pre-existing conditions or drugs that weaken the immune system and thereby promote a tuberculosis infection
Physical examination
Since tuberculosis usually occurs in the lungs, the doctor examines them by listening and tapping. In other parts of the body, you can also find signs of consumption, such as skin changes or headache over the lateral ribs or kidneys.
If a doctor suspects a tuberculosis infection, he has a number of other research options available that can confirm this suspicion.
Tuberculosis: test procedure
There are special tests that help to diagnose tuberculosis.
Tuberculin skin test (THT): In the tuberculin test according to Mendel-Mantoux, the doctor injects the patient a small amount of protein of the pathogen (tuberculin) under the skin. The immune system infected usually after a few weeks has formed special antibodies against the pathogen, is formed in tuberculosis infected at the injection site a reddened induration.
However, the test does not provide proof for or against an infection. If it occurs too soon after the infection, or if the immune system is weakened, it will not (yet) make enough antibodies. The tuberculosis skin test turns out to be negative despite infection.
IGRA (Interferon Gamma Release Assay): In this test, the blood of the patients is examined. If a person is infected with tuberculosis, special immune cells produce interferon gamma, which can be detected in this study.
The test is more accurate than the skin test. However, doctors are currently using it primarily in addition to the Tuberculin Skin Test (THT). If both the skin test and the IGRA test are negative, consumption is very unlikely.
Direct pathogen detection
For example, if the X-ray shows shadows in the lung tissue and the Tbc tests are positive, the tuberculosis bacteria must be detected directly. Exudate (sputum), gastric juice, urine, menstrual blood and brain water are examined. In some cases, doctors also take tissue samples from the lungs or lymph nodes (biopsies).
It is also examined whether the strain in question is resistant to certain antibiotics. However, the direct pathogen detection is complex and time consuming. It may take up to twelve weeks for results to be available.
Read more about the different test procedures in the article Tuberculosis Test.
roentgen
An X-ray of the thorax can reveal possible sources of inflammation. In primary tuberculosis, these appear as round shadows. If the hilum lymph nodes are infected, the shadow resembles a chimney. In a Miliar-TB, the doctor can recognize many small dots.
In addition, one can see in the picture fluid accumulation, for example, in an infestation of the pleura. If a fresh Tbc infection is suspected, make a re-admission after three months at the earliest. Thus, the course of tuberculosis can be assessed.
CT (computed tomography)
If you can not detect anything or only little on an x-ray, the doctor will arrange for a CT scan. Thus, tuberculosis herds can be discovered, which are covered for example by the collarbone. Also for inflammation elsewhere in the body (extrapulmonary tuberculosis) CT images are helpful.
blood test
Through a comprehensive examination of the blood, the doctor checks values whose change is in favor of the disease of a particular organ. In addition, certain blood levels, such as CRP and white blood cells, may be elevated, suggesting inflammation in the body.
Tuberculosis: treatment
Thanks to antibiotics, tuberculosis is curable today. Nevertheless, the disease can still be severe, especially in immunocompromised people.
Active tuberculosis must always be treated. Speak for an active Tbc:
- Due to disease caused cavity (cavern) in the airways
- Inflammatory focus (to be recognized as a shadow in the lungs)
- Enlargement of an old (already known) stove with reactivated TB
- pathogen detection
Inpatient treatment and quarantine
Take special care with open tuberculosis. Patients are usually hospitalized and hospitalized. If effective tuberculosis therapy has been initiated, isolation can usually be reversed after three weeks. Thereafter, the person affected can also be cared for at home (outpatient).
antibiotics
Tuberculosis is mainly treated with antibiotics, which have proven particularly effective in the treatment of the disease. They are called antituberculotics. At the beginning of therapy, four medications are prescribed as standard for the first two months:
- isoniazid
- rifampicin
- pyrazinamide
- ethambutol
- alternatively: streptomycin
Subsequently, two antituberculosis drugs, usually rifampicin and isoniazid, are given for another four months. For example, if the patient has a condition such as HIV that weakens the immune system or relapses, the duration of the treatment will be extended.
The treatment of complicated tuberculosis may take more than a year. Since the drugs can have side effects, regular medical checks of important blood levels and organ functions are performed. In doing so, the doctor pays particular attention to the liver, kidneys and eyes.
cortisone
If tuberculosis patients have meninges, pericardium, peritoneum, or adrenals inflamed, doctors initially administer additional corticosteroids. This should be throttled an excessive inflammatory process.
Anti-cough medication
In the case of open pulmonary tuberculosis, the doctor also administers anti-cough medications. This also protects the environment as the patient spreads fewer pathogens in the air.
surgery
In some cases, drug tuberculosis therapy fails inadequately or not at all. This is the case, for example, with very large sources of inflammation. But even with bacterial strains that are resistant to drugs, surgery may be useful. Surgeons try to remove the tuberculous inflammatory foci.
Accompanying measures
Those who suffer from tuberculosis should avoid anything that can worsen the course of the disease. This includes the consumption of alcohol and tobacco. In addition, in addition to tuberculosis, doctors are also treating other conditions that could exacerbate tuberculosis.
Tuberculosis: disease course and prognosis
If a patient is treated properly and on time, tuberculosis is usually curable. However, there are a few factors that make it difficult to treat a child.
Weakened patients
If the patient suffers from chronic illnesses or has a weakened immune system, the chances of a cure for tuberculosis decrease. In severe cases, there may be pulmonary bleeding, lung collapse or blood poisoning with severe organ damage.
Galloping consumption
Especially dangerous is the rapid death of the inflamed lung areas, the so-called “galloping consumption”. In this case, the lung tissue becomes yellowish and friable, which is why professionals call this process caseation. If the dead material liquefies (melting), the Tbc stove can scatter.
Resistant pathogens
A particular problem is represented by TB bacteria which have become resistant to tuberculosis medicaments. In Germany, about twelve percent of tuberculosis cases are currently caused by pathogens in which at least one antituberculosis drug fails.
In about two percent of cases, the bacteria are even resistant to multiple drugs. Experts then speak of a multi-resistance. In this complicated TB, doctors then have to resort to reserve resources. The treatment lasts one and a half to two years.
Lack of compliance
For the success of therapy is crucial that the patient takes the prescribed medication regularly and permanently, even if the side effects can be uncomfortable. Otherwise the pathogens will not be sufficiently killed and resistances build up faster. Due to the long duration of treatment and the side effects of some medications, some patients do not keep their treatment plan.
Isolate contact persons
It is especially important to recognize and treat infected patients in good time. In particular, in contact with a patient with an open tuberculosis is immediately isolated. Only when three independent samples of the sputum are free of pathogens will the isolation be removed.
Preventive treatment
After unprotected contact with an infected person, a preventive treatment with the antituberculosis isoniazid is also useful. This prophylaxis usually lasts three to six months, provided the TB skin tests have failed. If the test result is positive, it will be treated preventively for nine months.
These measures are particularly important for immunodeficiencies, children and persons traveling in high-risk areas in the foreseeable future.
Hygiene measures in contact with infected persons
Strict hygiene measures are important in contact with patients with overt tuberculosis. The contact persons / nurses should wear gloves, gowns and a nose and mouth protection.
compulsory registration
Any patient who has tuberculosis and needs treatment is reported to the health department. There, personal data is registered and stored. In this way, the spread of the disease should be detected early and prevented.
Tuberculosis: vaccination
In the tuberculosis vaccine, an attenuated mycobacteria strain is injected into the skin. Since 1998, the vaccine is no longer recommended by the “Permanent Vaccination Commission in Germany. Because the risk of becoming infected is very low in this country.
Also, the vaccine does not protect reliably. After all, especially children in risk areas benefit from it: In case of tuberculosis infection, they are less likely to get sick.
Therefore vaccination is still recommended in some countries. Read more about this topic in the article Tuberculosis – Vaccination.
Additional information
guidelines
- S2k guideline “Tuberculosis in Adulthood” of the German Central Committee for the Control of Tuberculosis e.V. on behalf of the German Society of Pneumology and Respiratory Medicine e.V.