Prolactinoma is a benign tumor of the hypophysis (pituitary gland) which produces a high level of the hormone prolactin. As a result, the testicles and ovaries are stimulated too little, which impairs their function. Typical symptoms include the absence of the rule in women and impotence in men. The prolactinoma is usually successfully treated with medication or, in rare cases, surgically. Find out more about the prolactinoma here.
Prolactinoma: description
Prolactinoma is the most common tumor of the hypophysis (pituitary gland). It causes the hypohysis to release more of the hormone prolactin. A prolactinoma can occur in both men and women. Most commonly, prolactinoma develops in women younger than 50 years.
Depending on the size of the tumor, this is called a microprolactinoma (diameter less than ten millimeters) or macroprolactinoma (diameter greater than ten millimeters). Most prolactinomas fall into the first category, so they are less than ten millimeters. Besides, they are usually benign; Malignant prolactinomas are very rare.
The hormone prolactin
Prolactin plays an important role in reproductive function in women. During pregnancy and breastfeeding, blood prolactin levels are elevated. In pregnant women, the hormone is responsible for the mammary glands developing and growing. It also stimulates the cells of the mammary gland to produce milk. Sucking the baby on the nipple, this stimulates the small muscle cells of the mammary gland – milk emerges.
During breastfeeding, the high level of prolactin can suppress ovulation and prevent recurrence while breastfeeding. However, it is crucial, among other things, how often and how long the child is breastfed. Breastfeeding is by no means a reliable method of contraception.
Prolactinoma: symptoms
In two ways, a prolactinoma can cause symptoms:
- It produces a lot of prolactin, which affects the effects of other hormones.
- It grows and displaces adjacent tissue, such as nerves that lead from the eye to the brain.
Prolactinoma causes sexual dysfunction in men and in pre-menopausal women. Postmenopausal women do not have any symptoms with a prolactinoma because the ovaries have already stopped functioning.
Prolactinoma: symptoms in pre-menopausal women
A high prolactin level in women of childbearing age inhibits ovulation, resulting in irregular or even missed amenorrhoea (amenorrhea). About 10 to 20 percent of women who fail to receive high levels of prolactin. Due to the cycle disorders, women with a prolactinoma also have difficulty getting pregnant. Other symptoms include a dry vagina and hot flashes.
The prolactinoma also stimulates milk production and secretion. In about 24 percent of women with high levels of prolactin, small amounts of breast milk (galactorrhoea) are released, although the woman is not pregnant or nursing.
Another symptom is osteoporosis. Especially with long-term prolactinoma sufferers have a lower bone density.
Prolactinoma: symptoms in postmenopausal women
In postmenopausal women, a prolactinoma shows no symptoms. This is because prolactin can no longer influence the cycle. Affected women will only notice a prolactinoma if it has grown so much that it affects adjacent tissues and causes headaches or blurred vision. However, it can also be discovered by chance if, for another reason, the head is examined with an imaging technique (magnetic resonance imaging, MRI).
Prolactinoma: symptoms in men
Prolactinoma causes too high a prolactin level in men and inhibits the gonads, in this case the testicles. These consequently produce less sperm and testosterone, the most important sex hormone of men. Typical symptoms include libido, impotence, infertility and listlessness.
Potency disorders and libido loss are the first symptoms of prolactinoma. In some cases enlargement of the breast (gynecomastia) and spontaneous milk flow (galactorrhoea) may occur. However, this is more common in women because the male mammary glands are less sensitive to prolactin.
If the prolactinoma has been around for a long time, the muscle mass may decrease. In addition, pubic hair and beard growth can regress. As with women, bone mass also decreases in men. A long-standing prolactinoma can lead to osteoporosis.
Macroprolactinoma causes more symptoms
If the prolactinoma becomes larger than one centimeter and thus becomes a macroadenoma, it can press on neighboring structures of the brain. Frequently, the optic nerve is under pressure, resulting in impaired vision. Most sufferers have bilateral lateral visual field defects. In some cases, only one eye may be affected.
The pressure exerted by the prolactinoma on the pituitary gland may interfere with the production of other hormones of the gland, such as hormones of the thyroid or adrenal cortex. As a result, the function of the institutions concerned is reduced.
The pressure of the tumor on brain structures can also cause headaches.
Prolactinoma: causes and risk factors
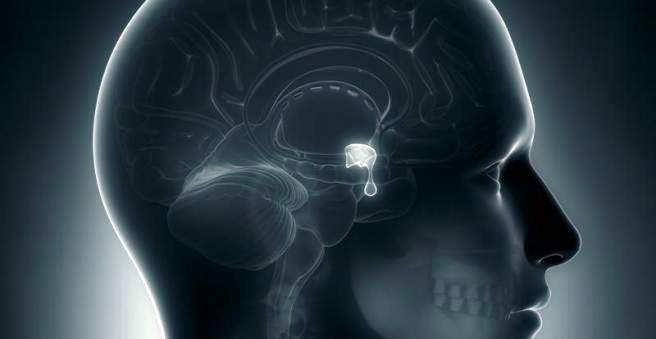
The prolactinoma consists of altered cells of the pituitary (pituitary gland), a hormone gland just below the cerebrum. More specifically, the prolactinoma develops from cells in the anterior pituitary gland (adenohypophysis). The pituitary gland has different cells that produce different hormones. The so-called lactotrophic cells produce the hormone prolactin.
A prolactinoma develops when a lactotrophic cell mutates and begins to divide uncontrollably. So, finally, a large mass of altered cells, which all form prolactin – the prolactin level increases. About 10 percent produce growth hormone in addition to prolactin.
Mostly a prolactinoma develops without a recognizable cause. In rare cases, it develops as part of a genetic disease, the multiple endocrine neoplasia type 1 (MEN 1).
Prolactinoma: examinations and diagnosis
To detect a prolactinoma, there are several tests. The competent expert in suspected prolactinoma is an endocrinologist, a specialist in hormone balance. The doctor will first record the medical history (anamnesis). For example, he asks the following questions:
- Are you pregnant?
- Do you use estrogens or certain medications such as risperidone, metoclopramide, antidepressants, cimetidine, methyldopa, reserpine or verapamil?
- Do you suffer from a headache?
- Do you have blurred vision? If so, what kind?
- Are you sensitive to cold, powerless or tired?
Subsequently, the doctor will perform a physical examination. He will examine you for visual disturbances such as visual field defects, signs of hypothyroidism and estrogen or testosterone deficiency.
The next step will be to have the doctor take a blood sample to measure prolactin levels. The blood test should be performed at least one to two hours after waking up, as the level of prolactin is higher during sleep than during wakefulness.
In the case of a prolactinoma, the measurement result can range from a small increase in prolactin to a thousand-fold increase in prolactin. Generally, larger prolactinomas cause higher levels of prolactin. Prolactin levels in excess of 250 micrograms per liter (μg / L) are most likely associated with a prolactinoma. Then the findings should be secured with a magnetic resonance tomography (MRI, also called magnetic resonance tomography) of the head. However, very small prolactinomas (microadenomas) are not always visible on MRI.
Other causes of high prolactin levels
An increased prolactin level (hyperprolactinemia) is not always necessarily due to a prolactinoma. In addition to stress and other illnesses, certain medications can cause high levels of prolactin, such as dopamine antagonists such as metoclopramide (in case of nausea and vomiting) or some agents used to treat mental illnesses (such as antidepressants, neuroleptics).
Prolactinoma: treatment
Not every prolactinoma needs treatment. If it is very large or causes symptoms, treatment is advisable. For small prolactinomas, which show no symptoms, can also be dispensed with a treatment. Doctor and patient together will weigh the benefits and risks of treatment options.
Medication
If treatment is necessary, the prolactinoma usually responds very well to the administration of so-called dopamine agonists. These are drugs that cause a similar effect in the body as the body’s own messenger dopamine. Dopamine agonists can thus lower the level of prolactin and shrink the prolactinoma or even make it disappear altogether.
It usually takes about two to three weeks for the prolactin level to drop. However, the prolactinoma usually does not shrink until after a few weeks to months. If the tumor interferes with the visual field, an improvement in the visual disturbance usually occurs a few days after the start of treatment.
Dopamine agonists usually need to be taken for several years. The prolactin levels are constantly monitored during this time.
For a prolactinoma, the following dopamine agonists may be given:
bromocriptine
Bromocriptine has been used for prolactinoma treatment for about 30 years. It is taken twice a day and works very effectively by quickly lowering the level of prolactin. However, bromocriptine can cause many side effects: sufferers complain of dizziness, nausea and a stuffy nose. However, many of the side effects can be prevented by taking the medicine before eating or at bedtime.
cabergoline
Cabergoline is taken only once or twice a week and causes fewer side effects. It can lower prolactin levels by about 90 percent and is therefore the treatment of choice. However, it is not recommended for women who want to become pregnant.
Drug treatment in pregnancy
During pregnancy, the pituitary gland is doubled in size to produce more prolactin – the hormone is important for milk production. Especially in women with a macroprolactinoma, this can be dangerous. If you have a prolactinoma and would like to have a baby, you should talk to a health care provider about getting treatment before you become pregnant. Among other things, the following questions need to be clarified:
- When should the therapy with dopamine agonists be stopped?
- What is the risk of prolactinoma growing during pregnancy?
- What are the treatment options if the prolactinoma grows again?
- Can I breastfeed my child?
If vision problems or headaches occur during pregnancy, this may indicate that the prolactinoma has regrown. To be able to recognize this at an early stage, an eye test is performed every month. After treatment for a prolactinoma, most women can become normal pregnant.
Surgical treatment
If the patient does not respond to dopamine agonists, the prolactinoma must be surgically removed. In a woman with a very large macroprolactinoma, surgery is the treatment of choice. The risk that the prolactinoma will continue to grow during a possible pregnancy is too high in this case.
At surgery the prolactinoma is removed via the nose. The surgeon uses an endoscope, ie a long, thin instrument, which is equipped with a light source and a camera.
The increased prolactin levels usually fall off directly after the operation, in microadenomas sometimes even to the normal value.
radiotherapy
Radiation therapy is rarely used, even if drug and surgical therapies have not been sufficiently successful. Irradiation can decrease prolactinoma and lower blood prolactin levels. However, the therapy often shows its full effect only after years and also has many side effects such as nausea, fatigue, loss of taste and sense of smell and hair loss. In addition, half of the patients who have received radiation therapy develop a pituitary dysfunction over the past 10 years, with hypophysectomycosis reduced blood levels.
Prolactinoma: disease course and prognosis
If it is a microprolactinoma, drug therapy with dopamine agonists can almost always achieve a normal prolactin level. If surgery is necessary, even with a small prolactinoma, this usually leads to normal prolactin levels in the long term. Nevertheless, it can come later to a relapse. This also applies to a large one prolactinoma (Macroprolactinoma).