African sleeping sickness is a tropical disease caused by parasites. These are transmitted through the bite of the tsetse fly. Sleeping sickness exists only in Africa, but related diseases also occur on other continents. It is mainly locals who suffer from it, but tourists are rare. Since sleeping sickness usually ends in death if left untreated, it is important to diagnose and treat it early. Read more about African sleeping sickness here.
Sleeping sickness: description
The sleeping sickness (Trypanosomiasis) is caused by the unicellular parasite Trypanosoma brucei triggered. There are two forms of illness – the West African and the East African variant:
The East African form accounts for only about 2 percent of all cases of sleeping sickness. She is progressing very fast. This means that there is very little time left for diagnosis and therapy. But this form of sleeping sickness mainly affects animals and, more rarely, humans.
The West African form of sleeping sickness is more common, progressing more slowly and sometimes diagnosed only years after infection.
The geographical boundaries of the two forms of disease are becoming increasingly blurred. Thus, in Uganda, an East African country, both forms already occur in different areas. Although the data is difficult to understand, the DRC and the Central African Republic in particular are affected by the tropical disease. Since the data come from different health systems, it can be assumed that sleeping sickness is also found in other countries in this region.
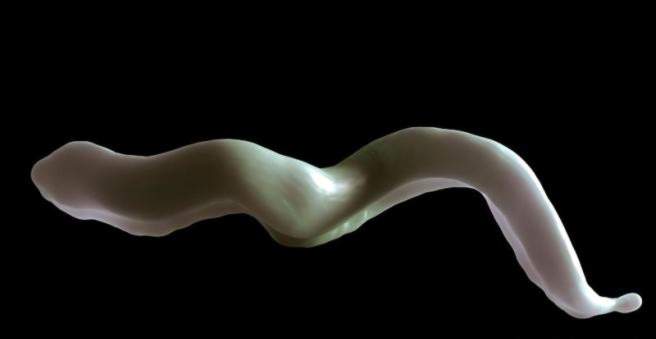
The pathogen: trypanosomes
Trypanosomes belong to the protozoa, as well as the causative agent of malaria. Like malaria, the disease can not be transmitted from person to person. Rather, they are transmitted by the bloodsucking tsetse fly during stinging on humans. The parasites spread through the bloodstream in the human body and multiply by division. The immune system can poorly recognize and fight the intruder because it is constantly changing its surface.
The West African variant of sleeping sickness is from the subspecies Trypanosoma brucei gambiense caused the East African variant of Trypanosoma brucei rhodesiense.
Sleeping sickness: symptoms
After the sting of a tsetse fly and the transmission of the trypanosomes, painful, inflamed redness may develop at the injection site within days to weeks. Doctors speak of a so-called Trypanosomenschanker. Often the puncture site is in the face or neck area.
In the next stage (hemolymphatic stage) of the disease, the parasites spread through the blood and lymphatic system throughout the body. There are strong lymph node swelling and periodic fever phases. Also severe headache and body aches, chills and fatigue may occur. Kidney infection (nephritis) can be the result if the kidneys are affected.
Finally, the trypanosomes affect the central nervous system (meningoencephalitic stage). As a result, it comes to the eponymous disorders of the sleep-wake cycle. In addition, paralysis, cramps or Parkinson-like symptoms (rigor = muscle stiffness, tremor = tremor, ataxia = disturbed motion coordination) are possible. Behavioral disorders and irritability also occur. Finally, the patient falls into a coma and dies.
This general course of disease is evident in both forms of sleeping sickness. In detail, there are some differences:
West African sleeping sickness
In West African sleeping sickness, the course of the disease is slower than in the East African form. It may take up to three weeks for a lesion to show at the injection site. The feeling of tiredness can last for several months, until it comes to the actual complaints of sleeping sickness. After months to years personality changes occur. The patient is easily irritable. He complains of increased fatigue. The distortion of the day-night rhythm often occurs only slowly over several months. The feeling of hunger is disturbed and the patients lose weight. After a few years, those affected fall into a coma and eventually die of multiple organ failure.
East African sleeping sickness
The germ Trypanosoma brucei rhodesiense triggers the East African form of sleeping sickness. It is ultimately a fast and more serious variant of the more prevalent West African form. Fever and chills as well as a sore, inflamed puncture site can already be seen days after the bite of the tsetse fly. The parasites quickly infect the lymphatic and blood systems and spread throughout the body. Lymph nodes, liver and spleen swelling are palpable after only a few weeks. Irritability, sleep disturbances and paralysis can already occur after weeks to months. After a few months, the patient falls into a coma and dies of parasitic infestation and failure of various organs.
Sleeping sickness: causes and risk factors
The sleeping sickness is caused by the parasite (Protozoon) Trypanosoma brucei caused, where there are two subspecies: T. b. rhodesiense and T. b. gambiense, They are transmitted through the bites of the bloodsucking tsetse fly either from infected animals or infected humans to healthy humans.
When sucking blood, the causative agent of sleeping sickness from the tsetse fly reaches the human skin. Through the lymphatic system and the bloodstream, it spreads in the body and finally affects the central nervous system. Since the trypanosomes regularly change their surface, they are not recognized by the immune system fast enough. This so-called antigen change explains why the human immune system is so helpless against sleeping sickness.
Sleeping sickness: examinations and diagnosis
The suspicion of sleeping sickness arises when someone comes to the doctor with symptoms such as fever, headache and body aches and lymphadenopathy and tells of a recent extended stay in Africa (short-term travelers are not the typical patients).
The diagnosis can be secured by the detection of trypanosomes in the body of the patient. For this purpose, the doctor may take sample material from the puncture site, a blood sample or a sample of cerebrospinal fluid (CSF).
The diagnosis and treatment of sleeping sickness should be carried out by a specialist physician (tropical medicine).
Sleeping sickness: treatment
The sooner sleeping sickness is treated, the better the chances of recovery. The therapy depends among other things on the stage of the disease. Especially in the last stage (Meningoenzephalitisches stage), the treatment is often very difficult and requires the use of highly effective drugs.
Sleeping sickness: therapy before infestation of the brain
If the trypanosomes have not yet attacked the central nervous system, the drugs pentamidine and suramin are used. They fight the protozoa, but due to their toxicity they have some side effects. Both drugs were developed before or during the Second World War and strongly affect important metabolic processes, such as sugar and kidney metabolism.
Sleeping sickness: Therapy in case of attack of the nervous system
If the brain is already affected by sleeping sickness, further medication is needed. Because pentamidine and suramin can not cross the blood-brain barrier and therefore does not work in the brain. Some of these drugs are chemotherapeutic agents that are also used in cancer and HIV therapy. Unfortunately, these drugs are associated with severe side effects.
- Melarsoprol: arsenic compound. Kills trypanosomes but has dangerous side effects, such as brain damage that ends fatally in about three to ten percent of cases.
- Eflornithin: Used in this country against women’s beards. Possible side effects include hair loss, gastrointestinal discomfort, abnormal blood counts, and transient hearing loss.
Sleeping sickness: disease course and prognosis
If left untreated, sleeping sickness usually ends fatally. However, if the disease is detected early and treated consistently, physicians can often cure the patient. However, this is a process that often takes months to years. Regular blood draws, as well as spinal cord functions are part of the surveillance, which should guarantee a therapeutic success.
For a long time, many of the medicines for sleeping sickness were not available. Since 2001, there has been cooperation between the World Health Organization (WHO) and several private pharmaceutical companies to ensure that the most important sleeping sickness medicines can be delivered to affected countries free of charge. The “Doctors Without Borders” (MSF) is responsible for the logistics of this cooperation. In this way, the number of sleeping sickness cases could be significantly reduced.
Sleeping sickness: prevention
When traveling to the risk areas of sleeping sickness, it is important to effectively protect against mosquito bites. This includes wearing long pants and long sleeves and using repellents. Before traveling to the appropriate risk areas, you should always visit a tropical health professional to familiarize yourself with the most important precautionary measures sleeping sickness and other tropical diseases.