Reye syndrome is a serious cellular disorder that can occur in young children and adolescents. It particularly affects the brain and liver and can be fatal. The exact causes are not yet clear. However, the Reye syndrome is particularly associated with influenza, herpes and chickenpox viruses. Scientists also believe that drugs such as acetylsalicylic acid can trigger the Reye syndrome after a virus infection.
Reye syndrome: description
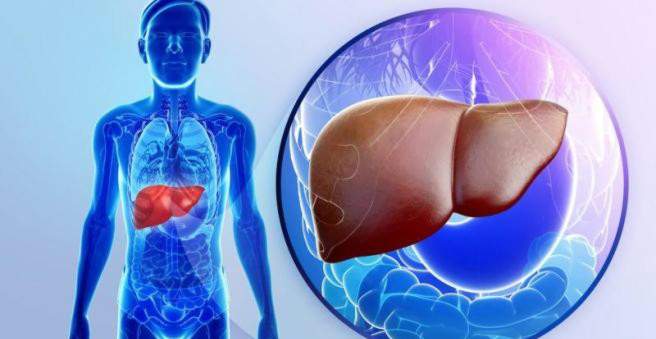
Reye syndrome is a rare, serious and potentially life-threatening disease of the brain and liver (“hepatic encephalopathy”) in children. It occurs especially after a virus infection and the intake of acetylsalicylic acid (ASA). The exact context is so far unclear. For example, the Reye syndrome was observed after infection with cold and flu viruses or chickenpox viruses. Even viruses that cause gastrointestinal infections with diarrhea or vomiting may be related to Reye syndrome. The list of potentially involved viruses may be much longer.
The Reye syndrome was discovered in Australia in the 70’s. Shortly thereafter, many cases of severe liver and brain diseases in America were attributed to Reye’s syndrome. But it took a few more years before the first assumptions about a connection with viral diseases and the pain and fever drug acetylsalicylic acid came up. The consequence was a broad education by the media that acetylsalicylic acid should not be given to children. Although Reye’s syndrome has been much rarer since then, the association between the virus, ASA and Reye’s syndrome has never been clearly established.
Reye syndrome: symptoms
Reye syndrome often occurs in children when parents are thinking that the viral infection has been overcome. There is increased vomiting without nausea. The child becomes increasingly confused, restless, irritable or even just weak and is always less responsive. In addition, a child with Reye syndrome can seizure and eventually even fall into a coma.
The reason for these symptoms is that in Reye’s syndrome, intracranial pressure increases as fluid accumulates in the brain (edema formation). The increased pressure affects important nerve centers and nerve tracts in the brain.
At the same time, Reye syndrome causes liver damage and fatty degeneration. Their function is severely limited, leading to a variety of metabolic disorders with different symptoms. Thus, in addition to the neurotoxin ammonia also bilirubin increasingly enters the blood, which can provide a yellow skin color.
In general, the child is seriously ill, and urgently needs intensive care.
Reye Syndrome: Causes and Risk Factors
The exact causes of Reye syndrome are unknown. However, it is known that Reye syndrome causes damage to the mitochondria. Mitochondria are often referred to as the powerhouses of cells because they are essential for energy production. The malfunction of the mitochondria in Reye’s syndrome is particularly evident in the cells of the liver and brain, but also in the muscles, for example.
Salicylates like ASA can interfere with the metabolism of the mitochondria, making them more susceptible to further damage. Some experts explain the relationship between ASA and Reye syndrome. This connection, which has been accepted by experts, has never been scientifically proven. The same applies to the assumption that certain viruses are the trigger for the Reye syndrome.
In addition to viral infections, salicylates and age, there may also be a genetic risk for the disease. Some people are apparently more susceptible to Reye syndrome than others. The exact genetic causes are still unclear here.
Reye syndrome: examinations and diagnosis
The doctor first raises the medical history (anamnesis). For example, he asks the child’s parents if he has recently had a viral infection and / or has taken salicylates. Also important are the description of the symptoms such as vomiting, possible convulsions and increasing confusion and restlessness. They are possible signs of brain involvement.
Depending on the extent of the disease, the liver may be enlarged in Reye syndrome, which the doctor can detect when palpating the abdomen. In addition, a blood test may provide evidence of liver involvement.
blood test
In the case of liver damage, certain substances increasingly enter the blood, such as liver enzymes (transaminases) as well as waste products, which the liver actually filters out of the blood and breaks down. For example, elevated liver enzyme levels and elevated levels of ammonia may indicate liver damage.
Since the liver is also responsible for the blood sugar level, a simple blood glucose test can give a quick information about the liver function – in the case of Reye’s syndrome, hypoglycaemia may be present.
The liver is also involved in blood clotting. In Reye’s syndrome, therefore, the blood clotting time may be prolonged. This can be determined by the Quick value or the INR (international normalized ratio), determined by means of a blood sample.
tissue sample
To confirm the diagnosis “Reye Syndrome”, the doctor can take a tissue sample (biopsy) of the liver and examine it for a corresponding cell damage. Especially the mitochondrial damage is noticeable here. In addition, there are increased accumulations of fat in the cells in Reye’s syndrome. This is a sign that the liver can no longer adequately process the fat.
Other investigations
Information about the condition of the liver can also give an ultrasound examination. If the doctor suspects an increased intracranial pressure, this is checked by a computed tomography (CT).
The Reye syndrome is not easily distinguishable from other diseases. The various symptoms can also be caused by other diseases, including those that are much more common than the rare Reye syndrome. For this reason, several other diagnostic tests are made to exclude, for example, meningitis, septicemia or severe bowel disease.
Reye syndrome: treatment
The Reye syndrome can not be treated causally. The doctors can only try to alleviate the symptoms and ensure the survival of the patient. This requires intensive care treatment.
The focus is particularly on brain swelling (brain edema) and liver failure. With the help of drugs that you directly into the bloodstream, and other measures (such as elevation of the upper body), you can try to reduce the pressure in the brain. In severe liver damage, the organ must be supported in its tasks (such as filter function and the regulation of sugar metabolism). For example, an excessively high level of ammonia in the blood (hyperammonaemia) can be treated by medication (with sodium benzoate) or by dialysis (hemofiltration). In severe cases of liver damage, a liver transplant may be required.
The work of all body organs is related. Especially the kidney and the liver form a well-rehearsed team. Renal failure (hepatorenal syndrome) therefore threatens sudden liver damage. With the help of medications, the medical team can uphold urinary excretion via the kidney.
Cardiac and pulmonary functions are also closely monitored, as, for example, artificial respiration may become necessary due to brain damage.
Reye syndrome: disease course and prognosis
The Reye syndrome is very rare, but usually takes a fast and difficult course. About 50 percent of the patients die. Many survivors suffer permanent damage. So stays after a surviving Reye’s syndrome often a brain injury, which manifests itself for example by paralysis or speech disorders.