Retinal detachment is a rare disease of the eye, in which the retina on the ocular fundus is detached. Affected persons perceive flashes of light and complain about various visual disturbances. Left untreated, retinal detachment can lead to blindness, so it is an ophthalmological emergency. Read all important information about retinal detachment here!
Retinal detachment: description
In retinal detachment (retinal detachment, retinal detachment), the retina (retina) that lines the eyeball separates from the inside. Since the retina consists primarily of sensory cells that register, process and relay the visual information, the detachment usually affects the visual performance.
Retinal detachment untreated leads to blindness
Retinal detachment is a rare disease. Every year about one in 10,000 people are affected. Acute courses take place especially between the ages of 45 and 65 years. In addition, the retinal detachment occurs familial. The disease has a special significance in ophthalmology, because an untreated retinal detachment can lead to blindness in the affected eye.
How fast this happens depends on the extent of retinal detachment. Retinal detachment was a virtually untreatable disease as late as the 1920s. Fortunately, this has changed as a result of the rapid development of ophthalmology, so that today blindness can usually be prevented. Nevertheless, the earlier the retinal detachment is treated, the better the chances of recovery.
Retinal detachment: symptoms
The disease is characterized by some classic symptoms: Retinal detachment is generally noticeable by a distorted vision. Characteristic are flashes of light (photopsias) in the affected eye. Patients see this especially in the dark. The effect is caused by tensile forces exerted on the retina by structures inside the eye (for example connective tissue strands). In addition, you may still encounter:
Black dots or flakes
This “soot rainstorm” also called “flying mosquitoes” are black dots or flakes that seem to be moving. So you do not always stay in the same place visually. The reason for this are usually tears or bleeding in the retina.
Visual field loss (scotoma)
The vision in certain areas is completely absent. Affected people often report that this is like a black shadow slowly spreads. The starting point of the increasing shadow is often also the place of incipient replacement. The fact that the shadow increases, indicates an increasing detachment of the retina. For example, if the shadow descends from top to bottom like a curtain, retinal detachment probably began at the bottom and continues upward. Such an increasing visual field loss is a absolute alarm signal for an acute retinal detachment. Signs like these should by no means be ignored as they require immediate action.
The symptoms may all be present, depending on the cause of the cause, or they may occur one at a time. For a long time, however, a retinal amotio can also completely symptom-free run. This is especially the case when the retinal detachment is small and located in the margins of the retina.
The severity of retinal detachment discomfort depends primarily on the location of the damage to the retina. If, for example, the area of the retina on which most of the nerve cells are present (“place of sharpest vision” or macula) is affected, vision is particularly impaired.
Retinal detachment: causes and risk factors
The retina is only about 0.1 to 0.5 mm thick and consists, in simplified terms, of two superposed different layers. On the one hand, the layer containing the nerve cells (Stratum nervosum). Underneath, towards the back of the eye, lies the second layer. This is due to their dark color as Stratum pigmentosum designated.
Normally, there is one between these two layers of the retina wafer-thin, liquid-filled gap, In this gap, there is a slight negative pressure, which “sucks” the two layers. Different reasons can cause the upper layer of the retina to detach from the lower one. This is called retinal detachment.
The separation of the two layers is problematic because the Stratum pigmentosum is responsible for the nutrition of the overlying stratum nervosum. When the connection between the layers is interrupted, the sensory cells die there after a short time and cause the typical retinal detachment symptoms.
Important for the stability of the retina: the vitreous body
Very often it comes because of diseases of the vitreous (Corpus vitreum) in the eye to a retinal detachment. This is a structure that fills the inside of the eye to almost two-thirds. The gelatinous substance of the vitreous body gives the eyeball its stable form. At the same time he presses the retina against the ocular fundus, thus preventing a detachment of the upper retinal layer from the lower. The vitreous thus plays a very important role in the stabilization of the retina.
The most common causes of retinal detachment
There are several causes for the entry of fluid into the cleft between the two retinal layers:
Rhegmatogen (due to cracks)
By far common Form of retinal detachment, the so-called rhegmatogenous amotio, penetrates through a small tear in the retina fluid from the eyeball between the two retinal layers. As a result, the upper retinal layer rises and dies in the course. However, not every tear causes retinal detachment. It often happens that this remains completely symptomless.
Cracks in the retina often occur in the case of damage to the vitreous, for example in the so-called rear vitreous detachment, As a result of age-related fluid loss, the vitreous body collapses somewhat and tears a hole in the retina, where it adheres to its posterior surface. This is noticeable through impaired vision and blurred vision. Especially when looking around quickly, such a visual disturbance moves further than the actual eye movement that was made. This is because the movement of the liquid of the vitreous body is slower than the movement of the head. These may therefore be signs of retinal detachment. Another cause of retinal cracking is Blows to the eye (traumatic retinal tear).
Traktiv (due to traction)
In the so-called traction-related retinal detachment, also called complicated retinal detachment, the upper retinal layer is literally pulled away by connective tissue strands inside the eye. It arises mainly in the context of diseases in which forms abnormal connective tissue in the interior of the eye. This connective tissue is firmly attached to the upper layer of the retina. Over time, the connective tissue strands shrink and pull on the upper retinal layer. This causes the detachment from the lower retinal layer. Examples of such diseases: diabetic retinopathy, retinal vein occlusions, retinopathy of prematurity, retinal necrosis or cataracts (after surgery).
Exudative (due to fluid)
Under the lower retinal layer is the so-called choroid, This is a very vascular layer that supplies the overlying retina with blood. A exudative retinal detachment arises when, from the vessels of the choroid, fluid penetrates between the two layers of the retina and there leads to a detachment of the upper retinal layer. The main causes of fluid leakage from the vessels of the choroid are inflammation or tumors of the choroid.
Combination traction-rhegmatogen
In the traction-induced rhegmatogenous retinal detachment Both retinal tear and connective tissue strands inside the eye are responsible for retinal detachment. The tear is usually caused by the train, which is often caused by an overgrowth of the connective tissue. This form is common in diabetics.
Risk factors for retinal detachment
Various risk factors increase the likelihood of retinal detachment. Which includes:
- Surgeries on the eye (for example cataracts)
- repeated inflammation of the eye
- Accidental injuries
- Myopia
In shortsighted eyes, the eyeball is too long, which is why the retina is already slightly stressed and thus easier tear. While in the normal-sighted population only about 0.2 percent of people are affected by retinal detachment, about seven percent of the short-sightedness suffer from it.
Other risk factors include eye diseases such as diabetic retinopathy, Coats’s disease and retinopathy of prematurity. In these diseases, regular ophthalmological examinations should take place in order to detect a pathologically changed retina as soon as possible.
Retinal detachment: examinations and diagnosis
The ophthalmologists are the specialists for retinal detachment. If necessary, a clinic with an ophthalmological department (Ophthalmology). This is especially true when the symptoms develop suddenly and quickly. Frequently, the symptoms described by the patient already indicate the presence of retinal detachment. The doctor could ask this question in conversation:
- Did the symptoms come on suddenly?
- Do you see black dots, dashes or flashes of light?
- Are you taking shade in your field of vision?
- Have you noticed a vision deterioration?
- What diseases are known to you?
investigations
Both eyes must always be examined, even if only one is affected. First, a determination of visual acuity is helpful. This can be used to determine whether vision is reduced and whether there are differences from known visual acuity.
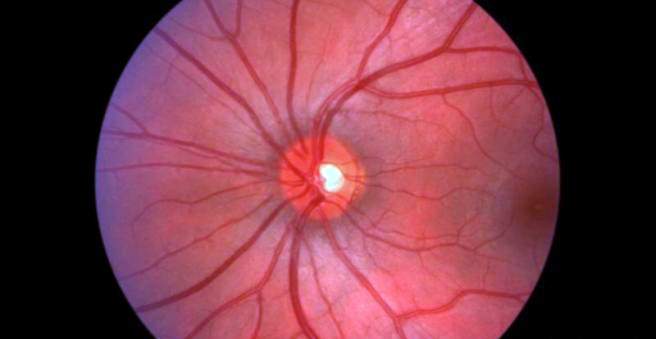
The most important examination in suspected retinal detachment is the Ophthalmoscopy. This is usually performed by the ophthalmologist with a certain apparatus, the so-called slit lamp. Prior to this, the doctor drips a drug into the eye, which dilates the pupils. This facilitates his view of the retina. In the examination, the doctor looks at the ocular fundus, which is why the ophthalmoscopy as funduscopy is designated (lat. Fundus oculi = ocular fundus). He can see directly on the retina and recognize any abnormalities immediately.
In a retinal detachment fall usually bubble-like withdrawals of the retina. Rhegmatogenous retinal detachment is characterized by a red hole surrounded by blisters. In addition, the form of retinal damage can already give a first indication of the cause. Horseshoe-shaped holes with their round side towards the center indicate rhegmatogenous damage. Peripheral round holes are more likely to indicate damage from tissue regression, for example, in old age. Tractive retinal detachment is usually caused by gray strands, while exudative retinal detachment shows bleeding and fatty deposits.
If it is not possible to make a clear diagnosis, the ophthalmologist can also use the retina to diagnose the retina ultrasound investigate. If the retinal detachment lies in the area of the macula, a so-called Optical coherence tomography (OCT) be helpful.
Retinal detachment: treatment
Retinal detachment is an ophthalmological emergency! So if you notice signs of retinal detachment, consult an ophthalmologist as soon as possible. The sooner the retinal detachment is treated, the sooner the detached retina recovers.
For treatment so far no drug therapy is available. On the other hand, there are a number of procedures that re-apply the upper retinal layer to the lower layer, thus repairing the damage. Basically, retinal surgery requires a hospital stay of several days. After retinal detachment therapy has been completed, check with an ophthalmologist regularly.
Laser / cold probe in the early stage
In the early stage of the disease, when there is only a small tear in the retina or only a slight detachment of the retina, the upper retinal layer can be covered by a special laser (Photocoagulation) or one cold probe (Cryopexy) can be reconnected to the lower layer. These two procedures are possible on an outpatient basis. Where the laser or the cold probe hits the retina, small scars form on the fundus, which firmly connect the two retinal layers and fix them to the fundus. Although the crack persists, the retina around the damage is fixed. The vision loss is usually low.
The laser and cold probe are particularly important as preventative procedures, so to close cracks before it comes to retinal detachment. However, it should be noted in this regard that most patients with asymptomatic retinal tears do not follow retinal detachment. Two weeks after the surgery, stable scars have been formed, eliminating the risk of retinal detachment.
Therapy procedure for large-scale retraction
For large-area retinal detachment, there are two main types of procedure.
Constricting surgical procedures
An effective way to treat larger retinal detachments is the Dentation of the eyeball from the outside. The procedure is usually under local anesthesia, takes about 20 to 60 minutes and requires depending on the course of a hospital stay of about three to seven days. This is done from outside the eyeball by an operatively attached seal or cerclage Pressure exerted and thereby the detached upper retinal layer pressed back to the lower layer.
Seal and cerclage are made of silicone and differ mainly in their shape. While the seal is rather flat, the cerclage is a kind of loop that surrounds and circles the eye in a circle. To attach to the eye, they are sutured to the outermost layer of the eyeball (dermis = sclera). These methods are used primarily in those cases in which a shrinking vitreous pulls on the retina.
Removal of vitreous body (vitrectomy)
A newer method for treating a retinal detachment is the partial removal or replacement of the vitreous body. The procedure is usually performed in local anesthesia, takes about 30 to 60 minutes and requires a hospital stay of about three to seven days.
In the vitrectomy Three small punctures are made in the eye: one for the introduction of fine surgical instruments, a second for a light source and a third for a flush drainage. Afterwards the liquid of the glass body is sucked off. This is followed by the introduction of a special liquid into the eye. This displaces the fluid that has accumulated between the two separate retinal layers. As a result, the upper retinal layer rejuvenates the lower one. In the next step, this liquid is sucked off again. In the final step, the interior of the eye is filled with silicone oil, perfluorocarbons or gas. This restores pressure in the eyeball, preventing retinal detachment. The gas is usually reabsorbed within several weeks by itself. If silicone oil has been used, it must be removed after about two to seven months. Following this, normally enough of the body’s own fluid builds up in the eye, which maintains the pressure in the eye.
After the procedure you should not read at first, but you usually do not have to hold a bed rest. Around two to three weeks later, there are usually no restrictions. If a gas mixture has been used to replace the vitreous humor, additional information may be important. So sufferers should not fly first.
Retinal detachment: disease course and prognosis
Without treatment, retinal detachment is progressively worsening. There is almost always a blindness. The faster the diagnosis and treatment, the better the prognosis. However, it also depends on which area of the retina is affected and which specific cause is responsible for retinal detachment. Slightly less than half of all retinal detachments can be prevented by preventive measures.
The best prognosis is the ruptured (rhegmatogenous) retinal detachment. Almost all rhegmatogenous retinal detachments can be repaired by surgery. However, when retinal detachment is at the point of sharpest vision, there is usually a limited field of vision and reduced visual acuity despite therapy. Even a few hours existing detachment of the retina leads there to irreversible damage. However, severe impairments can often be alleviated or prevented by a rapid start of therapy.
Prolonged retinal detachment can become a so-called proliferative vitreoretinopathy to lead. This is a reactive proliferation of tissue around the vitreous, which can lead to the most severe vision disorders, including blindness. Another complication of retinal detachment is the involvement of the second eye. For example, if one eye is affected by rupture (rhegmatogenous) retinal detachment, there is a 20 percent risk that the other eye will be affected by retinal detachment over time.
Risk patients should undergo a retinal inspection (ophthalmoscopy) once a year from the age of 40. If retinal holes on healthy eyes are noticeable, it is possible and sometimes advisable to prevent them with a laser or refrigeration application. In case of sudden worsening or (recurrence) of the symptoms of a Retinal detachment Immediately visit an ophthalmologist.