Crohn’s disease is a chronic inflammation of the intestine, which is usually bumpy. Typical symptoms include abdominal pain and severe diarrhea. Crohn’s disease can not be cured so far. But the symptoms can be favorably influenced by medicines and a corresponding lifestyle. Read here what is Crohn’s disease, what causes the disease and how to treat it.

Crohn’s disease: short overview
- Description: chronic inflammatory bowel disease
- Causes: not yet fully understood. Possible genetic predisposition, disturbed barrier function of the intestine, autoimmune reactions, unfavorable lifestyle
- Main symptoms: spasmodic abdominal pain, diarrhea, fatigue, abscesses
- Treatment: Cortisone, immunosuppressants, surgery, psychotherapy
- Forecast: very different courses and degrees of severity, not curable
Crohn’s disease: description and causes
Crohn’s disease is one of the ulcerative colitis to the chronic inflammatory bowel disease (CED). Main symptoms are spasmodic abdominal pain and diarrhea. The complaints usually occur in batches. Patients can therefore be symptom-free for a longer period of time.
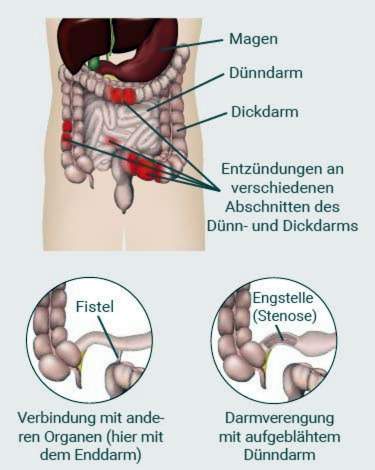
Crohn’s disease can occur throughout the digestive tract – from the mouth to the anus. In most cases, however, only the last section of the small intestine, the large intestine or these two bowel parts are affected together. This can be healthy with diseased intestinal sections alternate. In the diseased areas not only the mucous membrane is inflamed, but all wall layers of the intestine can be affected.
Crohn’s disease varies from patient to patient. In the case of an unfavorable course ulcers, narrow passages (stenoses) or connecting passages (fistulas) form to other organs.
Why some people get Crohn’s disease, is still not fully understood. But there are different hypotheses.
Genetic changes
It is known that certain genetic changes increase the risk of Crohn’s disease. For example, about half of the patients have mutations in the gene NOD2, which plays a role in the immune system.
Disturbed barrier function in the intestine
A possible explanation is a disturbed barrier function of the intestinal wall. The intestine must be permeable on the one hand, so that nutrients can enter the body, on the other hand, but also prevent pathogens from entering. If this balance is disturbed, problems arise. For example, bacteria can nest in the intestinal wall and thus provoke the immune system to violent defense reactions.
Autoimmune reaction
Another hypothesis is that the inflammation of the intestinal wall is caused by misguided actions of the immune system. Doctors call this an autoimmune reaction. The trigger can then be, for example, an infection to which the body’s immune system reacts excessively strong.
lifestyle
The lifestyle also influences the disease risk and the course. Smokers are more likely to develop Crohn’s disease. Stress, on the other hand, can trigger new relapses of the disease.
Crohn’s disease: symptoms
Crohn’s disease varies greatly. The severity of Crohn’s disease depends on how well Crohn’s disease has developed in the gut. In some patients, the disease is mild and may go undetected for many years.
Stomach pain: The pain in Crohn’s disease is usually colicky and occur especially in the lower right abdomen. This resembles the symptoms of appendicitis.
Diarrhea: Diarrhea occurs during a push usually three to six times a day. As a rule, they do not contain blood.
Weight loss: Due to a lack of appetite or fear of pain, those affected often do not eat enough. Due to the diarrhea, many nutrients are lost. That’s why patients often lose weight.
Abscesses and fistulas: Inflammation can lead to the formation of encapsulated pus (abscesses). Also connecting passages (fistulas) to other organs, into the abdominal cavity or to the outside can arise. They often occur in the anal area and are often a first indication of Crohn’s disease.
Scarring and intestinal obstruction: When the inflamed intestinal sections heal, scars often form. In severe cases, such an intestinal obstruction (ileus) can arise, which must be operated on.
Fatigue, fatigue, fever: Due to the inflammatory processes, the patients feel tired and limp. Often, fever is added and causes a general malaise.
Nutrient deficiency: The inflamed intestinal sections can no longer properly absorb the food components. The diarrhea causes additional nutrients to be lost. Therefore, patients often suffer from deficiency symptoms. Zinc deficiency promotes, for example, skin changes and inflammations such as aphthae in the oral mucosa. In the long term, due to calcium deficiency also threatens osteoporosis
General inflammation tendency: Patients with ulcerative colitis more often suffer from arthritis, eyes or liver inflammation.
Chronically or in turns
If the symptoms of Crohn’s disease persist for at least six months, it is called a chronic course. More often, however, the disease progresses in batches. At the same time the symptoms can disappear completely for a while.
Crohn’s disease: treatment
Crohn’s disease can not be cured yet. However, the treatment can slow down the inflammatory processes, relieve discomfort and delay relapses. The doctor takes into account which sections of the digestive tract are inflamed and how severe the disease is.
drugs
Crohn’s disease is all about getting rid of the inflammation and relieving the symptoms. Serve with drugs that weaken the activity of the immune system. With certain medications can also prevent a relapse (recurrence) over a period of time.
corticosteroids, also colloquially called cortisone, are very effective drugs that quickly reduce inflammation. The dose depends on the severity of the course. Most cortisone is prescribed in tablet form, for example prednisone or prednisolone. For severe symptoms, an infusion may be required.
Steroids affect the entire body. Therefore, they should not be used for long-term therapy. For long-term use, the patient often puts on weight and gets a characteristic “full moon face”. Also, blood sugar and blood lipid levels rise. In addition, susceptibility to infections increases and the risk of osteoporosis increases.
budesonide is a cortisone derivative. Its effect unfolds especially in the lower small intestine and its transition to the colon. For inflammatory foci in this area, it is the better choice because it is better tolerated than other cortisone preparations.
aminosalicylate is better tolerated than cortisone, but less effective. It is therefore used only in mild disease progression.
TNF antibody like infliximab and adalimumab are antibodies that target certain inflammatory factors. They are administered as an infusion or as an injection under the skin. Their effect occurs comparatively quickly. But they can trigger allergies. TNF antibodies are also prescribed for the prevention of a new push and for the long-term treatment of anal fistulas.
ustekinumab is an active ingredient that blocks the inflammatory messengers interleukin 12 and 23, thus reducing inflammatory reactions. The drug is prescribed if other medicines are not effective.
Antibodies to integrins (Vedolizumab) must also be given by infusion, but are well tolerated. The drug is prescribed if other medicines are not effective.
immunosuppressants Like azathioprine, 6-mercaptopurine or methotrexate also reduce the immune activity. They are used to prevent a new disease spurt. However, it takes at least three months for them to take effect. Sometimes the intake reduces the number of white blood cells, also nausea and liver inflammation are possible.
Acute treatment of the main symptoms: Diarrheal medications such as loperamide and anticonvulsants such as butylscopalamine for abdominal pain
Treatment of anal fistulas: For anal fistulas, short-term antibiotics such as cipofloxacin and metronidazole are prescribed. In the long term, TNF antibodies can be used.
|
Low to moderate thrust |
Heavy thrust |
Prevention of new relapses |
|
|
Corticosteroids (oral) |
standard therapy |
standard therapy |
not suitable |
|
Corticosteroids (intravenous) |
No |
Yes |
No |
|
budesonide |
In mild small intestinal infestation |
No |
No |
|
TNF antibody |
No |
Yes |
When immunosuppressants fail |
|
Vedolizumab |
No |
Yes |
Yes |
|
ustekinumab |
No |
Yes |
Yes |
|
immunosuppressants |
No |
No |
Yes |
Crohn’s disease: operations
If treatment with medication is not enough, surgery may be necessary. In the context of such interventions are
- narrowed areas stretched with a balloon
- Fistulas closed
- Abscesses removed
- Bowels closed
- severely diseased intestinal sections removed
Crohn’s disease: diet
There is no universal diet for Crohn’s disease. Overall, Crohn’s disease patients should rather spare their gastrointestinal tract.
- Eat several small meals rather than a few!
- Do not eat too hot and not too cold!
- Eat and not too sour and not too spicy!
Try out
Bloating foods, raw foods, fat or sweet, but also coffee, fruit juices and alcohol can stress the digestive tract. What is well tolerated is individually different. Try out what you get.
Observe incompatibilities
Many Crohn’s disease patients suffer from intolerances to lactose, gluten or fructose. These once again have a very reinforcing effect on an already susceptible intestine. If that’s the case, they should avoid it.
Eat rich in nutrients
About the damaged intestine get less nutrients into the body. Make sure that you are particularly nutrient-rich to compensate for this.
Diet during a push
During a push stomach and intestine need special protection. Most patients then tolerate a light, low-fiber diet. Purification of the food can also be relieving. Possibly, in case of a severe episode, a temporary artificial diet via the drip may be useful, so that the digestive tract can calm down.
psychotherapy
Persistent clogging, abdominal pain, slackness – in severe cases, Crohn’s disease severely impairs a patient’s quality of life and self-esteem. Some develop depression or anxiety disorder. Psychotherapy can help to better manage the stress and to develop a positive attitude to life and a strengthened self-image despite the illness.
As part of a cognitive behavioral therapy, the patient questions and corrects negative thought patterns and practices new behaviors. In addition, because stress can aggravate the symptoms, patients learn strategies that help them avoid unnecessary mental stress.
stress reduction
Patients with Crohn’s disease benefit from learning relaxation techniques. This reduces stress that can adversely affect the course of the disease. Helpful methods include:
- Autogenic training
- Progressive muscle relaxation according to Jacobson
- meditation
Crohn’s disease: examinations and diagnosis
For the diagnosis of Crohn’s disease several examinations are necessary. At the beginning is the detailed medical history (medical history), which also includes the family medical history.
As part of a physical examination, the doctor scans the lower abdomen and checks whether there are pressure pains. He also examines the oral cavity and anus for symptoms such as fistulas.
colonoscopy: The most important examination for the diagnosis of Crohn’s disease is colonoscopy (colo-ileoscopy). The doctor introduces a flexible instrument with a camera (endoscope) into the intestine in order to be able to observe the mucous membrane.
The instrument is also equipped with fine pliers. With them, the doctor can take tissue samples (biopsies), which are then examined in the laboratory for pathological changes.
Also constrictions (stenoses) and fistulas, in which pathological connections in the abdominal height, to other organs or to the outside are formed, are recognized and, if possible, treated the same.
Gastroscopy: In gastroscopy, an endoscope is inserted through the oral cavity. So the doctor can see the stomach and duodenum.
Ultrasonic: With an ultrasound machine can be found inflammatory thickened intestinal walls, constrictions, fistulas and abscesses. However, mucous membrane changes can only be found with the endoscope. An ultrasound does not just help with the diagnosis. Since it is less stressful for the patient, the doctor can also regularly check the disease process.
Magnetic Resonance Imaging (MRI) and Computed Tomography (CT): With these examinations, the doctor can see changes in parts of the intestine that can not be seen during colonoscopy.
Blood analysis: As part of a blood test is mainly on a specific protein, called CRP, tested. An elevated value indicates inflammation. In most cases Crohn’s disease is also a complete blood count.
Crohn’s disease: disease course and prognosis
Complete cure for Crohn’s disease does not exist. The disease varies greatly from patient to patient. While some may be completely symptom-free for a long time or have little pronounced symptoms, other patients often experience recurrent, severe disease episodes. Overall, the likelihood that Crohn’s disease patient must be operated on is high.
However, you can do a few things yourself to reduce the severity of the symptoms and prolong the symptom-free stages:
- Consistently take the prescribed medication
- Sleep enough,
- Relax regularly
- Eat yourself as it is good for you
- Move a lot
In addition, Crohn’s disease patients have a slightly higher risk of developing colon cancer. This can be minimized with regular examinations for early detection.
Overall, the life expectancy of people with Crohn’s disease is normal, although Crohn’s disease is not curable.
Additional information
Books:
- Chronic Inflammatory Bowel Disease (CED): 40 Questions and Answers for Patients (Ulrike von Arnim, 2016, Thieme)
- Healthy Eating – Crohn’s Disease & Ulcerative Colitis: Over 100 Recipes of Inflammatory Bowel Disease (CED) (Gudrun Biller-Nagel, 2017, Trias)
- Shit up the socks: living and loving with Crohn’s disease (Ingrid Beck, 2017, Books on Demand)
guidelines:
- Update S3 guideline: Diagnosis and treatment of Crohn’s disease, German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS), (as of 2015)
Self-help:
- Competence Network Bowel Diseases
- Living with CED