In hypercholesterolemia, sufferers have high levels of cholesterol in their blood. Hypercholesterolemia is one of the lipid metabolism disorders. The causes of elevated cholesterol levels are manifold. A dangerous consequence is vascular calcification. It can lead to serious cardiovascular diseases such as a heart attack. To treat hypercholesterolemia, sufferers should change their lifestyle, have causes treated, and eliminate risk factors. Read all important information about hypercholesterolemia here.
Hypercholesterolemia: description
Hypercholesterolemia is a disorder of lipid metabolism in the body. Here, the amount of cholesterol in the blood is increased. Cholesterol (cholesterol) is a vital natural product of animal cells. It is extremely important for the construction of the cell membrane. In addition, cholesterol is required for the production of bile acids for digestion of fat in the intestine and for the synthesis of sex hormones (testosterone, estradiol, progesterone). The stress hormone cortisol and the messenger aldosterone (water and salt balance) are also formed from cholesterol.
Only a small portion of cholesterol is taken up with food. A much larger proportion is produced by the body itself, mainly in the liver and intestinal mucosa. This process is called cholesterol biosynthesis. This forms as an intermediate 7-dehydrocholesterol. This substance is the precursor to vital vitamin D.
Normally, the total blood cholesterol is below 200 milligrams of cholesterol per deciliter. Slightly elevated cholesterol levels (200-239 mg / dl) are considered medically borderline. Increasing levels are too high a cholesterol level, ie hypercholesterolemia.
lipoproteins
Cholesterol is only about 30 percent free in the human body. The remaining 70 percent are associated with fatty acids (cholesterol esters). As a fat-like substance, cholesterol is water-insoluble. However, in order to be transported in the blood, it must become water-soluble. In addition, cholesterol and cholesterol esters combine with other substances. Together with lipids (fats: triglycerides, phospholipids) and proteins (apoproteins) it forms fat-protein complexes called lipoproteins.
Depending on the composition, a distinction is made between different lipoproteins. Among the most important are chylomicrons, very low density lipoproteins (VLDL), low density lipoproteins (LDL) and high density lipoproteins (HDL). In addition, there is IDL (intermediate density lipoproteins), which stands between LDL and VLDL, and the lipoprotein a, which is similar in structure to the LDL.
Chylomicrons transport dietary fats (triglyceride content 85 percent) from the intestine into the body. VLDL in turn consists mainly of triglycerides that are produced in the liver. This lipoprotein is eventually converted to IDL and LDL. It loses its fats, whereas the cholesterol increases.
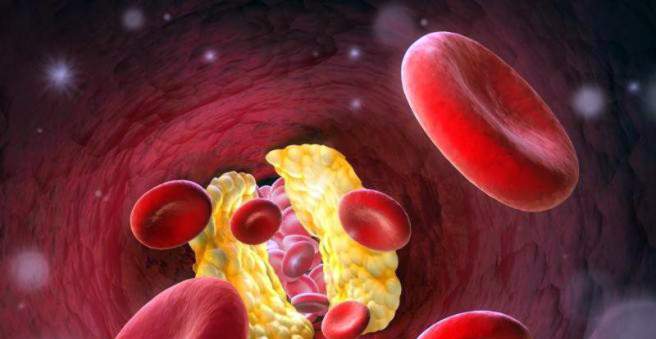
In hypercholesterolemia, the lipoproteins LDL and HDL play a crucial role. They consist mostly of cholesterol and keep the cholesterol balance. LDL transports cholesterol from the liver via the blood to the remaining body cells. Increased LDL also means increased cholesterol levels up to hypercholesterolemia. As a result, the cholesterol deposits in the blood vessels and leads to arteriosclerosis (plaques, “vascular calcification”). This is counteracted by the lipoprotein HDL. It transports excess cholesterol back to the liver, preventing increased cholesterol levels.
Therefore, LDL is also known as “bad” and HDL as “good cholesterol”.
Hypercholesterolemia as a group of lipid metabolism disorders
Hypercholesterolemia is the result of a disorder in fat metabolism and is associated with elevated cholesterol levels. Lipid metabolism disorders are also referred to as hyperlipoproteinemia, hyperlipidemia or dyslipidemia. In addition to hypercholesterolemia also includes the hypertriglyceridemia. In addition, there is a combined hyperlipidemia. Patients have a high cholesterol and high triglyceride fats in the blood.
Hypercholesterolemia: symptoms
Hypercholesterolemia, which means elevated cholesterol levels in the blood, does not cause any discomfort. Rather, hypercholesterolemia is a sign of other diseases. In the long run, however, high blood cholesterol can have serious consequences.
arteriosclerosis
The distribution of cholesterol in the body is due to LDL, which is typically elevated with hypercholesterolemia. If the HDL lipoproteins are reduced, the cholesterol return transport to the liver is disturbed. The result is hypercholesterolemia. The excess cholesterol deposits in the vessel walls. Then a process is set in motion, which ultimately harms the vessels (arteries = arteries). With cholesterol, fats, carbohydrates, blood components, fibrous tissue and lime enter the vessel wall. Hypercholesterolemia thus leads to arteriosclerosis, popularly known as vascular calcification.
CHD and heart attack
In vascular calcification, the arteries are increasingly narrowed. If the heart disease is affected, doctors talk about coronary heart disease (CHD). In this way, hypercholesterolemia can also lead to heart attack. Thus, the risk of heart attack is approximately doubled with a total cholesterol level (HDL plus LDL) of 250 mg / dl. With a total value of over 300 mg / dl, it is four times as high as in people with normal cholesterol levels. The coronary arteries are sometimes almost completely closed and the heart muscle can not be properly supplied with oxygen. Affected persons complain of a feeling of pressure or pain in the chest. Tachycardia, dizziness, sweats and shortness of breath are also signs of heart attack.
PAD and stroke
If the arteries of the legs are damaged by hypercholesterolemia, it can lead to intermittent claudication. Physicians speak of a PAD (peripheral arterial disease). Patients suffer from painful circulatory disorders, especially under stress (e.g., walking). If the neck and cerebral arteries are narrowed due to hypercholesterolemia, an oxygen deficiency in the brain may occur. Threatening short-term (TIA = transient ischemic attack) neurological deficits such as hemiplegia to stroke (ischemic cerebral infarction).
xanthome
Xathomas are fatty deposits in the tissue, especially in the skin. Due to hypercholesterolemia, but also due to hypertriglyceridemia, fats and cholesterol, for example, accumulate on the trunk or on the hands, forming yellow-orange skin thickening (plane xanthomas). If there is an increase in cholesterol in the eyelids, doctors talk about xanthelasma.
Larger skin thickenings of yellow-brownish color on elbows or knees are called tuberous xanthomas. Xanthomas on the finger or Achilles tendon are also symptoms of hypercholesterolemia. Also typical of hypertriglyceridemia are yellowish nodules on reddened skin, in particular on the buttocks and the extensor sides of the arms and legs. Medically, these skin manifestations are called eruptive xanthomas. Fat deposits on the lines of the hand usually indicate an increase in IDL and VLDL.
Hypercholesterolemia on the eye
High cholesterol may also be deposited in the cornea of the eyes. There, a visible turbidity ring of gray-white color forms at the edge of the cornea. Doctors in this case speak of an arcus (lipoides) corneae. This lipid ring is common in the elderly and is considered harmless. In adults less than 45 years, however, it is a clear indication of hypercholesterolemia.
Hypercholesterolemia: causes and risk factors
Hypercholesterolemia is more of a symptom than a pure disease. This also applies to other hyperlipidemias. Mostly they are the consequence of another illness or lifestyle. Depending on the cause of hypercholesterolemia, three groups are distinguished.
Reactive physiological form
For example, a high-cholesterol diet falls into this group. In response, fat metabolism in the human body is overloaded. Increased intake of cholesterol can not be eliminated fast enough and causes high cholesterol in the blood. Alcohol can also lead to hypercholesterolemia, especially with increased IDL in the blood. In the reactive-physiological form, however, elevated cholesterol levels are only temporary. After a short time, the values normalize again.
Secondary form
In the secondary form of hypercholesterolemia, other diseases cause high cholesterol levels. These include, for example, the diabetes mellitus diabetes. LDL is normally taken up by certain recipient structures (LDL receptors) of the body cells. The high cholesterol level in the blood decreases as a result. This particular LDL intake is delayed in Type 1 diabetes because it lacks insulin. The cholesterol therefore remains in the blood and the patient gets hypercholesterolemia. Obesity (adiposity) increases the production of LDL cholesterol. In addition, insulin does not work properly (insulin resistance, type 2 diabetes). Fatty acids are more likely to enter the liver, increasing VLDL (hypertriglyceridemia).
thyroid
Thyroid hypofunction (hypothyroidism) can also lead to hypercholesterolemia. In hypothyroidism, the messenger substances of the thyroid are reduced. However, they significantly influence the metabolic processes in the body. With low thyroid hormones, for example, fewer LDL receptors are formed, which ultimately leads to an increased cholesterol level.
Nephrotic syndrome and cholestasis
The nephrotic syndrome arises due to damage to the kidneys. Typically there are increased protein levels in the urine (proteinuria), decreased protein in the blood (hypoproteinemia, hypoalbuminemia) and water retention in the tissue (edema). But hypercholesterolemia and triglyceridemia are also classic signs of nephrotic syndrome. The “good” HDL cholesterol is often reduced. Furthermore, congestion of bile in the bile ducts (cholestasis) leads to increased lipoprotein levels and thus to hypercholesterolemia.
drugs
Many medications can also adversely affect lipid metabolism. Most cortisone preparations lead to hypercholesterolemia. Treatments with estrogens, the pill, water tablets (thiazides) or beta-blockers usually increase the triglycerides in the blood. Furthermore, high cholesterol levels were observed in pregnant women. In this case, however, the hypercholesterolemia hardly has a disease value.
Primary form
Here one speaks of a familial or hereditary (hereditary) hypercholesterolemia. The cause of high cholesterol levels lies in a defect of the genome. Experts distinguish a polygenetic from a monogental hypercholesterolemia. In polygenic hypercholesterolemia, multiple defects in the building blocks of the human genome (genes) lead to slightly elevated cholesterol levels. External factors such as poor nutrition and physical inactivity are usually added.
Familial monogenic hypercholesterolemia
In monogenetic hypercholesterolemia, the defect is solely in the gene containing the information for the production of LDL receptors. They are used to eliminate LDL cholesterol from the blood. In monogenetic familial hypercholesterolemia, these receptors or their function are either completely lacking (homozygous carriers) or the receptors are less active (heterozygous carriers). Affected without a healthy gene (homozygotes) have already in childhood or adolescence first signs of illness. Heterozygotes have a sick as well as healthy gene and suffer mostly in middle age first heart attacks, provided their hypercholesterolemia is not treated. Familial hypercholesterolemia can be inherited (autosomal dominant inheritance).
Hypercholesterolemia by various apolipoproteins
Another genetic defect may involve the apolipoprotein B100. This protein is involved in the construction of LDL and helps in the absorption of LDL cholesterol into the cell. More specifically, it accomplishes the binding of LDL to its receptor. If the function of the apolipoprotein B100 is disturbed, more cholesterol remains in the blood. This hypercholesterolemia can also be inherited (autosomal dominant). In addition to the apolipoprotein B100, there are also various apolipoprotein E forms. Medicine has found that hypercholesterolemia occurs mainly in humans with the apolipoprotein E 3/4 and E 4/4. You also have a higher risk of Alzheimer’s disease.
Hypercholesterolemia by PCSK9
PCSK9 (Proprotein Convertase Subtilisin / Kexin Type 9) is an endogenous protein (enzyme) found predominantly in liver cells. This enzyme binds LDL receptors, whereupon they are degraded. As a result, the liver cells can “fish out” less cholesterol from the blood. It comes to hypercholesterolemia. Studies have shown that certain defects in the genome (mutations) of the enzyme increase its effect (gain-of-function). As a result, high cholesterol levels continue to rise. However, cases have also been described in which PCSK9 has lost its function through mutations (loss-of-function), which reduces the risk of hypercholesterolemia.
Other hereditary dyslipidemias
Other disorders of lipid metabolism may also be due to genetic defects. Patients also have elevated cholesterol levels in their blood:
|
illness |
disorder |
disease characteristics |
|
Familial combined hyperlipoproteinemia |
|
|
|
Familial hypertriglyceridemia |
|
|
|
Familial dysbetalipoproteinemia |
|
|
|
hyperchylomicronaemia |
|
|
|
Familial hypoalpha lipoproteinemia |
|
|
In addition, the lipoprotein a may be increased. It is composed of LDL and apolipoprotein a. It inhibits inter alia processes in the blood clotting, especially in the dissolution of blood clots (plasminogen competitor). This speeds up vascular calcification (blood clots are involved in plaque formation in the vessel walls). With LDL hypercholesterolemia, lipoprotein a also increases the risk of cardiovascular diseases.
Hypercholesterolemia: diagnosis and examination
Hypercholesterolemia is detected by a blood test. In many cases, the elevated cholesterol levels are coincidental. You can have your cholesterol levels determined by your family doctor or a specialist in internal medicine (internist). For this he takes blood samples. This blood collection should be done on a fasting basis, ideally after a 12-hour fast (especially important for triglycerides). Subsequently, the blood is analyzed in the laboratory for triglycerides, LDL and HDL as well as total cholesterol and possibly also lipoprotein a. If the values are increased, blood is taken again, this time after food intake. For healthy adults without risk factors for vascular calcifications, the following guidelines apply:
|
LDL cholesterol |
<160 mg / dl |
|
HDL cholesterol |
> 35-40 mg / dl |
|
total cholesterol |
|
|
triglycerides |
<150-200 mg / dl |
|
Lipoprotein a (Lp a) |
<30 mg / dl |
If hypercholesterolemia has been detected at the time of blood collection, the physician will check the values after about four weeks. Furthermore, he can determine the “arteriosclerosis risk index” based on the LDL and HDL cholesterol levels. For this purpose, the LDL value is divided by the HDL value (LDL / HDL quotient). A result below two means a low, and over four mean a high risk of vascular damage.
Since hypercholesterolemia is a symptom, doctors need to make a more accurate diagnosis. For this purpose, the German Society of Fat Science has published a scheme with which hypercholesterolemias can be assigned to a disease.
|
LDL cholesterol blood level |
Family history of coronary heart disease (CHD) |
diagnosis |
|
> 220 mg / dl |
positive |
Familial hypercholesterolemia |
|
negative |
Polygenic hypercholesterolemia |
|
|
190-220 mg / dl |
positive |
Familial combined hyperlipidemia (especially with elevated triglycerides) |
|
negative |
Polygenic hypercholesterolemia |
|
|
160-190 mg / dl |
positive |
Familial combined hyperlipidemia (especially with elevated triglycerides) |
|
negative |
Pure diet-related hypercholesterolemia |
Medical history (anamnesis)
The medical history (history) is crucial for hypercholesterolemia. It provides the physician with information on possible causes and risk factors. The doctor will ask you about your eating habits and alcohol or cigarette consumption. Also tell the doctor about known illnesses that you suffer from, such as diabetes, thyroid or liver disease. Among other things, the doctor could ask the following questions:
- Do you smoke? How much alcohol do you drink?
- Are you already suffering from illness? If so, under which?
- Do you take medications permanently and what are they called?
- Do you sometimes feel pain in your legs when going for a walk, sometimes so much that you have to stop?
- Has hypercholesterolemia been detected in your family?
Physical examination
After the detailed questioning, your doctor will examine you physically. Risk factors such as severe overweight can be determined at first glance. It is also important how the fat is distributed. Especially the belly fat is considered to be questionable in connection with hypercholesterolemia. The doctor may calculate your BMI (body mass index) based on body weight and height. In addition, the doctor measures blood pressure and heart rate and listens to the heart and lungs (auscultation). In addition, water (edema) and fat deposits in the skin or on the muscle tendons (xanthomas) may indicate hypercholesterolemia. Also fat deposits in the eye (turbidity ring, Arcus corneae) indicate a disturbed lipid metabolism.
risk calculation
As part of the body and blood tests, the physician can determine a risk of cardiovascular disease. The value indicates how high the risk is that the respective patient will suffer a heart attack in the next ten years. There are different calculation systems for this. The PROCAM and CARRISMA risk calculators, the Framingham score, especially in the USA, and the ESC score for fatal events are widespread. In all, among other things, increased cholesterol levels are taken into account.
Further research
Under certain circumstances, the doctor will carry out further examinations. If there are signs of diseases that cause hypercholesterolemia, they need to be clarified. With the help of ultrasound (sonography), the doctor can also make the condition of large arteries – such as the carotid arteries (carotid arteries) – visible and assess the degree of vascular calcification. The so-called Doppler probe (duplex sonography) can also audibly check the blood flow of the arteries. If there is a suspicion of hereditary hypercholesterolemia, genetic and family studies can confirm the diagnosis.
Hypercholesterolemia: treatment
The goal of hypercholesterolemia therapy is primarily to reduce the risk of dangerous vascular calcification and thus of cardiovascular disease. Treatment should target LDL and HDL cholesterol and triglycerides within a specific target range. The triglycerides are reduced below 150 mg / dl in all cases. Ideally, HDL cholesterol is above 40 mg / dL in men and above 50 mg / dL in women. When lowering LDL hypercholesterolemia, the target value will be affected by any risk factors or existing diseases. Risk factors include:
- Hypertension (arterial hypertension)
- Smoke
- Heart disease in close relatives (CHD / heart attack in first-degree relatives, in men before the 60th, in women before the 70th year)
- Age (men over 45 years, women over 55 years)
- HDL cholesterol <40 mg / dl
There are currently different guideline values. For primary hypercholesterolaemias, a target below 160 mg / dl is sought after less than two of these risk factors, as recommended by the German Society for the Control of Dyslipidemia and its Consequences (Lipid-Liga, 2011).
If a patient with hypercholesterolemia has two or more risk factors, LDL cholesterol should be below 130 mg / dL. If a sufferer suffers from vascular disease (e.g., myocardial infarction, CHD, PAD) or diabetes, hypercholesterolemia is reduced to below 100 mg / dl. The same applies if the calculated 10-year risk (e.g., PROCAM) is above 20 percent. If a patient has both vascular disease and diabetes, the LDL cholesterol level should be less than 70 mg / dL.
Hypercholesterolemia Therapy Goals of the German Society of Cardiology
Here the experts are following the recommendations of the European Association of Cardiologists ESC (2011). She has developed a SCORE model that focuses on gender, age, smoking status, systolic (upper) blood pressure, and overall elevated cholesterol levels. The resulting ESC score records the risk of a fatal cardiovascular event within the next 10 years. In addition, the patients are divided into four groups:
|
risk |
condition (if one is true, the patient is already assigned to this risk group) |
|
low |
|
|
moderately increased |
|
|
high |
|
|
very high |
|
Patients at low risk should change their lifestyle at high cholesterol levels above 100 mg / dl. Drug treatment is only considered for prolonged LDL hypercholesterolemia above 190 mg / dl. At moderately high risk, experts recommend that elevated cholesterol levels be reduced to less than 115 mg / dl by improving dietary habits and possibly medication.
High-risk hypercholesterolemia should be reduced to less than 100 mg / dL with medication. And patients at very high risk should have LDL levels below 70 mg / dL. If this treatment goal is not achieved, the experts recommend lowering the high cholesterol by at least half of the initial value.
Strictly speaking, these guidelines are not therapy for actual hypercholesterolemia. If the cholesterol level in low-risk patients is between 70 and 100 mg / dl, for example, no treatment is necessary. However, at very high risk, medicines are immediately used in this area to prevent further cardiovascular disease.
Accordingly, hypercholesterolemia is not simply defined by elevated cholesterol levels above 200 mg / dl. Rather, it depends on the type and number of existing risk factors to a different high cholesterol value for the affected person.
Therefore, some experts do not speak of a hypercholesterolemia treatment, but of a lipid- or cholesterol-lowering therapy. This prevents cardiovascular diseases at high risk – especially when hypercholesterolemia is present – before (secondary prevention) and should prevent, for example, after a heart attack again life-threatening disease events (tertiary prevention).
Levels of hypercholesterolemia treatment
First and foremost is the change in lifestyle and eating habits. Overweight patients should try to reach normal body weight. Normal weight should keep their weight. Many patients always ask themselves the question “Cholesterol too high, what to do?”. The following tips can help you fight or prevent hypercholesterolemia.
Do sport or make your everyday life active!
For example, climb stairs instead of using the elevator! Ride a bike instead of a car to work! This not only counteracts LDL hypercholesterolemia, but also decreases your value for triglycerides. In addition, the “good” HDL is rising. In addition, you will take the most effective route and prevent further cardiovascular disease or diabetes!
Avoid excessive use of butter!
Many sufferers already help to replace butter with diet margarine and vegetable oils. In general, a high proportion of unsaturated fatty acids is beneficial, whereas saturated fatty acids should be avoided. Some experts assume that the excessively high cholesterol level can be reduced by about eleven percent in this way. Recommended are products containing phytosterols (e.g., sitostanol). They inhibit the absorption of cholesterol and should also be able to limit its production in the body. For children and adolescents with hypercholesterolemia, a daily intake of about one to three grams is recommended. However, too much phytosterols cause the opposite effect. They are very similar to cholesterol and in turn can trigger vascular calcifications.
Pay attention and avoid hidden fat!
This is mainly found in milk and dairy products (cheese!), Sausages, sauces and ready meals. Fast food is also high in fat. Instead, use reduced-fat products to counteract hypercholesterolemia. Also choose lean meats and sausages that contain low levels of saturated fat. These include, for example, low-fat fish such as trout or cod, game, veal and poultry.
Prepare your meals low in fat! Eat fruits and vegetables every day!
Cook without cooking oil! Grilling and stewing are suitable ways of preparing to reduce or prevent hypercholesterolemia. Experts also recommend eating fruits and vegetables as raw food (for example, in a salad).
Reduce high-cholesterol foods!
These include, above all, egg yolk (and its further processing, such as mayonnaise), offal or shell and shellfish.
Watch out for protein and fiber!
Above all, vegetable protein, which is contained in particular in soy products, can reduce hypercholesterolemia. Because this increases the intake of LDL and lowers the high cholesterol level. Fibers, on the other hand, fill you up for a long time and often prevent overeating. Oat bran, pectin, guar and psyllium should even act directly on the hypercholesterolemia. However, many dietary fiber can also reduce or eliminate the effects of cholesterol-lowering drugs.
Stop smoking and drink alcohol in moderation!
In severe hypertriglyceridemia, doctors even recommend a complete renunciation of alcohol. So you can also prevent other health problems such as liver damage. In addition, if you have hypercholesterolemia with elevated triglycerides you should also refrain from sugar-containing soft drinks.
Prefer “complex” carbohydrates!
Carbohydrates consist of sugar molecules that are strung together like pearls in a chain. Short chains are absorbed quickly and are more damaging to the sugar balance in the body. They are in particularly sweet foods (such as sweets). However, carbohydrates are an important source of energy. Therefore, eat long-chain, complex carbohydrates like whole grains.
Stay balanced!
Too hard diets harm the body rather than use it! Therefore, a change is about training other eating habits in the long run and not giving up everything abruptly. Frequent unsuccessful dieting even increases the risk of cardiovascular disease. Deshalb sprechen Ernährungswissenschaftler auch lieber von einer fettmodifizierten Kost: Sie müssen nur einen Teil Ihrer Ernährungsgewohnheiten ändern und sich auf pflanzliche statt tierische Fette konzentrieren.
Nahrungszusammensetzung
Die Deutsche Gesellschaft zur Bekämpfung von Fettstoffwechselstörungen und ihrer Folgeerkrankungen (Lipid-Liga) spricht sich für folgende Empfehlung aus, wie sich die tägliche Nahrung zusammensetzen sollte:
|
Nährstoff |
Menge bzw. Anteil an gesamter Energiezufuhr pro Tag |
geeignete Lebensmittelbeispiele |
|
Kohlenhydrate |
50-60 Prozent |
Obst, Kartoffeln, Gemüse, Getreideprodukte |
|
Eiweiß |
10-20 Prozent |
Fisch, mageres Geflügel, fettreduzierte Milch(produkte) |
|
roughage |
mehr als 30 Gramm/Tag |
Gemüse, Obst, Vollkornprodukte, Haferkleie (Cerealien) |
|
Fett |
25-35 Prozent |
Butter, Bratfett, fetthaltige Fleisch- und Milchprodukte Achtung vor verstecktem Fett! |
|
Fettsäuren |
gesättigte 7-10 Prozent |
tierisches Fett |
|
einfach ungesättigte 10-15 Prozent mehrfach ungesättigte 7-10 Prozent |
Raps-, Oliven-, Soja-, Maiskeim-, Sonnenblumenöl, Diät-Margarine |
|
|
cholesterol |
weniger als 200-300 Gramm/Tag |
Eigelb (nicht mehr als zwei pro Woche), Eigelbprodukte (z.B. Eiernudeln, Mayonnaise), Innereien |
Behandlung anderer Erkrankungen
Es gibt eine Reihe an Krankheiten, die eine Hypercholesterinämie begünstigen können. Daher wird Ihr Arzt auch diese Krankheiten behandeln. Leiden Sie an einer Zuckerkrankheit (Diabetes) oder an einer Schilddrüsenunterfunktion, sollten Sie die Therapievorschläge Ihres Arztes unbedingt beachten. Nehmen Sie auch Ihre Medikamente konsequent ein, um einer Hypercholesterinämie erfolgreich entgegenwirken zu können. Haben Sie Zweifel oder Fragen, zögern Sie nicht, Ihren Arzt um Rat zu fragen.
Medikamentöse Hypercholesterinämie-Behandlung
Ist die Hypercholesterinämie durch eine Umstellung des Lebens- und Ernährungsstils nicht ausreichend gesenkt worden, verschreibt Ihnen der Arzt Medikamente gegen den erhöhten Cholesterinspiegel. Kinder mit Hypercholesterinämie erhalten in der Regel erst ab sieben bis acht Jahren eine medikamentöse Behandlung. Zu Beginn einer medikamentösen Hypercholesterinämie-Behandlung verordnet der Arzt in der Regel nur ein Präparat, meist Statine. Werden die hohen Cholesterinwerte nicht ausreichend gesenkt, erhöht er die Dosis. Kommt es nach drei bis sechs Monaten zu keiner nennenswerten Besserung, erweitert er die Therapie mit anderen Hypercholesterinämie-Medikamenten.
Statine (CSE-Hemmer)
Statine hemmen ein Eiweiß namens HMG-CoA-Reduktase. Dieses Enzym benötigen die Leberzellen, um das körpereigene Cholesterin herstellen zu können. Wird das Enzym gehemmt, sinkt der Cholesterinspiegel in den Zellen (Cholesterin-Synthese-Enzymhemmer = CSE-Hemmer). Infolgedessen werden vermehrt LDL-Rezeptoren in die Zellhülle eingebaut. Über diese “Fangarme” kann die Zelle Cholesterin aus dem Blut aufnehmen. Die Hypercholesterinämie sinkt.
Anionenaustauschharze – Gallensäurebinder
Gallensäuren werden in der Leber produziert. Aus ihnen besteht die Gallenflüssigkeit, die zur Verdauung in den Dünndarm abgegeben wird. Die cholesterinhaltigen Gallensäuren werden später wieder aufgenommen und gelangen über das Blut zurück zur Leber, wo sie erneut zu Galle werden (enterohepatischer Kreislauf). Anionenaustauschharze beziehungsweise Gallensäurebinder binden eben diese Gallensäuren im Darm. Dadurch verschwinden sie mit ihrem Cholesterin aus dem enterohepatischen Kreislauf. Um neues Cholesterin für die Galle zu gewinnen, regen die Leberzellen ihre LDL-Rezeptoren an. Cholesterin wird aus dem Blut aufgenommen und die Hypercholesterinämie bessert sich. Bekannte Wirkstoffe sind Colestyramin und Colesevelam. Beide werden häufig mit Statinen kombiniert, um eine Hypercholesterinämie ausreichend zu behandeln.
Cholesterinabsorptionshemmer
Der Wirkstoff heißt Ezetimib und verhindert die Aufnahme (Absorption) von Cholesterin aus dem Darm. Für die Hypercholesterinämie-Behandlung gibt es eine feste Kombination mit dem CSE-Hemmer Simvastatin.
Fibrate
Neben der Hypercholesterinämie-Therapie werden Fibrate vor allem eingesetzt, um einen erhöhten Triglycerid- und erniedrigte HDL-Spiegel zu behandeln. Die Wirkung ist vielschichtig. Unter anderem steigt der Abbau triglyceridreicher Lipoproteine. Hinsichtlich einer Hypercholesterinämie muss jedoch eines beachtet werden: In Kombination mit Statinen steigt das Risiko, dass es zu Muskelschäden kommt (Myopathie; selten auch Rhabdomyolyse mit Auflösung der Muskelfasern).
Nikotinsäure
Dieses Arzneimittel wird ebenfalls mit Statinen kombiniert, um eine Hypercholesterinämie zu behandeln. In einer 2011 in den USA durchgeführten Studie mit dem Nicotinsäurepräparat Niaspan in Kombination mit Statinen konnte ein Nutzen allerdings nicht bestätigt werden. Das Risiko von Herz-Kreislauf-Erkrankungen sank nicht im Vergleich zu Hypercholesterinämie-Patienten, die nur CSE-Hemmer einnahmen. Vielmehr kam es sogar vermehrt zu Schlaganfällen, weshalb Niaspan vom Markt genommen wurde. Auch der Nachfolger Tredaptive ist nicht mehr erhältlich.
Omega-3-Fettsäuren
Den Omega-3-Fettsäuren werden zahlreiche Vorteile nachgesagt. Die europäische Behörde für Lebensmittelsicherheit EFSA veröffentlichte 2010 einen Bericht zu behaupteten Wirkungen verschiedener omega-3-Fettsäuren, da es diesbezüglich viele zum Teil widersprüchliche Studien gibt. Gemäß den Expertenaussagen unterstütze die Einnahme von omega-3-Fettsäuren eine normale Herzfunktion. Allerdings verneinten die Experten den positiven Effekt auf eine Hypercholesterinämie. Auch vorteilhafte Wirkungen auf das Immunsystem oder den Blutzuckerhaushalt wurden nicht bestätigt. Da omega-3-Fettsäuren jedoch sehr nebenwirkungsarm sind, werden sie von manchen Ärzten empfohlen, um eine Hypertriglyceridämie zu senken. Sie sind zudem gut mit anderen Fettsenkern kombinierbar.
PCSK9-Hemmer
Nach langer Forschung wurden im Herbst 2015 schließlich PCSK9-Hemmer zur Behandlung hoher Cholesterinwerte in Europa zugelassen. Bei den Wirkstoffen dieser Medikamentengruppe handelt es sich um Eiweiße, genauer um Antikörper, die an PCSK9-Enzyme binden und diese somit wirkungslos machen. Dadurch stehen wieder mehr LDL-Rezeptoren zur Verfügung, die einer Hypercholesterinämie entgegenwirken.
PCSK9-Hemmer kommen vor allem bei schweren (familiären) Hypercholesterinämien in Kombination mit Statinen zum Einsatz, insbesondere wenn vorangegangene Therapien einen hohen Cholesterinwert nur unzureichend gesenkt haben. Außerdem kann der Arzt diesen Wirkstoff verordnen, falls der Patient Statine nicht verträgt. PCSK9-Antikörper werden in der Regel alle zwei bis vier Wochen mit Hilfe einer Spritze unter die Haut (subkutan) verabreicht. Aufgrund der hohen Behandlungskosten erfolgt der Einsatz von PCSK9-Hemmern jedoch eher zurückhaltend.
LDL-Apherese
In manchen Fällen kann eine Hypercholesterinämie auch durch mehrere Medikamente nicht ausreichend gesenkt werden. Dies ist beispielsweise bei schweren familiären Hypercholesterinämien der Fall. Bestehen zudem Gefäßschäden, “wäscht” man das Blut außerhalb des Körpers und beseitigt das zu hohe Cholesterin. In einem künstlichen Kreislauf wird das Blut über Schläuche zu einer Maschine geleitet. Dort wird es entweder in Plasma und Zellen aufgeteilt oder direkt von LDL gereinigt. Anschließend wird das nun “saubere” Blut wieder über Schläuche zum Körper zurückgeführt. Mittels der LDL-Apherese können auch erhöhte Lipoprotein a-, IDL- und VLDL-Spiegel gesenkt werden. Das Verfahren wird für gewöhnlich einmal in der Woche durchgeführt. Parallel wird die Hypercholesterinämie weiterhin mit Medikamenten behandelt.
Hypercholesterinämie: Krankheitsverlauf und Prognose
Der Verlauf einer Hypercholesterinämie kann sehr unterschiedlich sein. Je nach Ursache unterscheidet sich das Ausmaß des erhöhten Cholesterinspiegels. So haben Menschen mit erblich bedingter Hypercholesterinämie ein deutlich höheres Risiko, an einem Herzinfarkt zu sterben. Untersuchungen zeigen, dass betroffene Männer und Frauen oft schon vor dem 60. Lebensjahr ein Blutgerinnsel in den Herzkranzgefäßen hatten als Personen mit einem normalen Cholesterinspiegel.
Beim Risiko einer Gefäßverkalkung und folgender Herz-Kreislauf-Erkrankungen spielen zudem viele verschiedene Faktoren eine Rolle. Achten Sie deshalb auf einen gesunden Lebensstil. Befolgen Sie außerdem den Rat Ihres Arztes und gehen Sie regelmäßig zu Kontrolluntersuchungen. Die einzelnen Therapieformen sprechen nämlich bei jedem Patienten unterschiedlich an. Letztendlich können Sie durch Ihren persönlichen Einsatz den Erfolg der Behandlung erzielen und den gefährlichen Folgeerkrankungen einer Hypercholesterinämie prevent.