Toxoplasmosis is an infectious disease caused by parasites. It is distributed worldwide. For the pathogens, humans are only an intermediate host; the final host is cats. Toxoplasmosis transmission is often via raw or underheated meat products. Most toxoplasmosis causes no complaints. Especially with immunodeficiencies and pregnant women but it can have serious consequences. Read all about toxoplasmosis and how you can protect yourself against the disease.

Quick Overview
- What is toxoplasmosis? Infectious disease caused by the parasite Toxoplasma gondii is caused. Man acts as an intermediate host of the pathogen; the end host are cats.
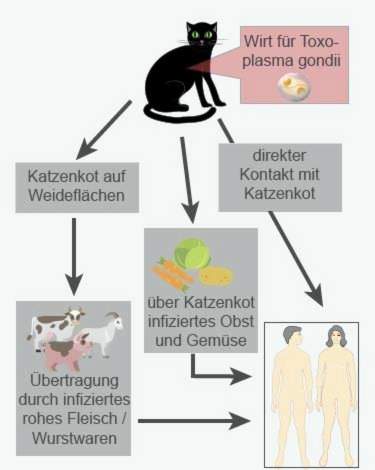
- Infection: Eating raw or insufficiently heated meat and sausage products, contact with cat droppings, insufficiently washed vegetables or salad.
- symptoms: In healthy immune system usually no, only occasionally flu-like symptoms and swollen lymph nodes. Rarely infestation of organs (such as eyes). In immunodeficiency (such as HIV / AIDS) and unborn in the womb toxoplasmosis can have serious consequences.
- Diagnosis: Blood test for antibodies against toxoplasma, possibly direct detection of the pathogens or their genetic material in patient samples (such as lymph node tissue); In the case of unborn amniocentesis (amniocentesis) or umbilical cord puncture.
- Treatment: with no / few symptoms usually not necessary. Otherwise, drug treatment with antibiotics and / or antiparasitics. A first infection in the Schwangegrschaft must always be treated.
Toxoplasmosis: description
Toxoplasmosis is an infectious disease caused by the parasites Toxoplasma gondii is caused. Actually, it is an animal disease (zoonosis). However, humans can “capture” toxoplasmosis as an intermediate host of the parasite.
Toxoplasmosis can be given to people of all ages. The infection is ongoing mostly unnoticed, Rarely, symptoms such as mild fever, headache and body aches occur. However, in people with weakened immune systems, toxoplasmosis can be serious. The same applies to a primary infection during pregnancy.
In a toxoplasmosis infection, the body produces specific antibodies to the parasite. Part of it continues to circulate in the patient’s blood even after it has healed. So this is future protected against a re-infection (lifelong immunity) – unless it eventually develops an immunodeficiency (such as HIV). Then you can get another toxoplasmosis.
Toxoplasmosis: frequency
It is estimated that about half of the adult population in Germany has a toxoplasmosis infection behind them. Generally, with age, the number of people who have ever been with the parasite increases Toxoplasma gondii have infected. In the age group 70 plus, this applies to more than seven out of ten people (throughput rate: 70 percent).
If a child is born with a toxoplasmosis acquired in the wombcongenital or congenital toxoplasmosis), this must be reported to the Robert Koch Institute (RKI). The RKI is the central facility for disease surveillance and prevention in Germany. In the years 2002 to 2015, between 10 and 23 cases of congenital toxoplasmosis were registered annually at the RKI. However, experts assume a high number of unreported cases. One reason for this is that usually only those children are reported who already have symptoms of illness at the time of birth. Often, but only in the course of months or years, consequential damage to the toxoplasmosis infection in the womb.
Toxoplasmosis: Prevention
There are a number of behavioral rules that reduce the risk of toxoplasmosis infection:
- Wash your hands with soap if you have touched raw meat or vegetables.
- Also clean used kitchen utensils (cutting board, knife, etc.) thoroughly after processing meat or vegetables.
- Do not eat raw meat or sausage products (minced meat, tartare, carpaccio, sausage, salami, prosciutto, etc.).
- Avoid also insufficiently heated meat and sausage products (especially from pork, lamb or goat meat). In order to kill the “eggs” (oocysts) of the parasite, meat must be heated to a core temperature of at least 50 ° C (roasting, cooking).
- Keep earthy foods (potatoes, carrots, etc.) separate from other foods so that they may not be contaminated as well.
- Wash, peel or cook vegetables, salads and fruits before eating.
- Wear gloves when gardening and wash your hands thoroughly afterwards.
- Do not feed cats with raw meat.
- Do not kiss a cat and wash your hands after contact with the animals.
- Clean the litter box daily with hot water. Particularly vulnerable people like pregnant women should leave this task to others.
- Cover a sandbox when not in use. To prevent cats from using it as a litter box.
- Particularly vulnerable people should not pet free-roaming cats.
- In open nature, do not drink unfiltered water from lakes, streams, etc. It may be contaminated with the “eggs” (oocysts) of the toxoplasmosis pathogen.
pregnant womanwho have not yet undergone toxoplasmosis infection and therefore do not have antibodies to the parasite, should follow the recommended preventive measures. Special advice applies when dealing with cats:
- Pregnant women should leave the daily cleaning of the cat lavatory with hot water (more than 70 ° C) to other family members.
- Cats should not be fed with raw meat, but only with canned and / or dry food. If this is not possible, pregnant women should stay away from the cat.
Toxoplasmosis: symptoms
Between the infection with toxoplasmosis and the appearance of the first symptoms usually pass two to three weeks. This period of time is called incubation period.
Toxoplasmosis symptoms in a healthy immune system
In people with a healthy immune system, toxoplasmosis occurs in about nine out of ten cases symptom-free, Rarely gets the infection flu-like symptoms such as mild fever, headache, body aches and fatigue. In addition, the Swell lymph nodes (mostly in the neck and neck area, occasionally on the whole body). Doctors then speak of lymphadenitis.
Rarely, toxoplasmosis affects the eyes or other organs. For example, inflammation of the retina and retina in the eye (retinochoroiditis or chorioretinitis), a form of pneumonia or encephalitis may develop.
A toxoplasmosis infection can also chronic run. The affected people usually do not notice it (latent course).
Toxoplasmosis symptoms in weakened immune system
In immunodeficiency, toxoplasmosis may be severe. This applies, for example, to HIV and AIDS patients as well as people after an organ transplant. Often it is not a primary infection. Instead, most people have been infected with the toxoplasmosis pathogen before. This then dormant for some years unnoticed (latent) in the body, before it was reactivated. Very often then one develops encephalitis (Encephalitis). The symptoms that occur depend on which brain region is affected by the inflammation. For example, headaches, fever, changes in nature, paralysis and epileptic seizures may develop.
Rarely does a toxoplasmosis in immunocompromised patients eyes, However, all other organs may also be affected, especially in AIDS patients (Heart, lungs, liver etc.).
Toxoplasmosis: causes and risk factors
Toxoplasmosis is caused by the unicellular parasite Toxoplasma gondii caused. Humans serve the parasite only as an intermediate host (as do pigs and cattle); The main hosts are cats and feline predators.
In the intestine of the cat, the parasite proliferates and develops egg-like precursors (oocysts). They are excreted in large numbers with the feces. After one to four days of air ripening, the oocysts become infective and remain so for several months.
routes of infection
Mammals, birds and humans are usually infected with contaminated food with the toxoplasmosis pathogen: The “eggs” of the parasite are mainly with insufficiently heated or raw meat or sausage products added. Most are pork, sheep and goat meat, but sometimes also with game and poultry. Even the one-off taste of raw meat dishes is sufficient for infection with toxoplasmosis!
Also foods that grow in the ground or near the ground (Vegetable fruit), may be contaminated with the toxoplasmic eggs (such as cat feces) and thus infectious. There is also one contact infection possible, ie the direct transmission of Toxoplasmen. For example, if you come into contact with infectious feces when cleaning the litter box and then touch your mouth with your unwashed hands, you may get infected with toxoplasmosis. You can also become infected when gardening in the soil contaminated with cat feces.
Relatively rare are the parasites in the womb transferred from the pregnant woman to the unborn child, This can happen when the woman becomes infected with the toxoplasmosis pathogen for the first time during pregnancy. If the infection occurs before pregnancy, there is usually no danger to the unborn child: The antibodies that the maternal organism has produced against the pathogen protect the child from infection.
Among the equally rare infection routes is the Parasite transmission in transplants – So if a patient’s organs are transferred to a donor suffering from toxoplasmosis.
Toxoplasmosis: examinations and diagnosis
The symptoms mentioned can give a doctor first indications of a possible infection with Toxoplasma. To clarify the suspicion, various diagnostic methods are available:
Toxoplasmosis: test for antibodies
Patients with healthy immune system As a rule, a blood sample is taken in order to examine them for antibodies to the body against toxoplasma. The type and amount of antibodies indicate whether the patient was previously infected with toxoplasmosis or whether it is a current infection. In the second case, the antibody test also reveals the stage of the disease the patient is in.
Toxoplasmosis: Direct detection
To determine an active infection beyond doubt, must the pathogen itself or its genome (DNA) be detected in patient samples. In this way, one can detect a toxoplasmosis even in people with weakened immune systems. In fact, the toxoplasmosis test for antibodies can be negative for them (due to the immune deficiency, not enough antibodies can be generated).
For direct pathogen detection, the doctor takes a tissue sample from the patient (for example, from the swollen lymph nodes). From this one tries to culture the Toxoplasmen in cell culture or animal experiment.
To detect the genetic material of the parasite, tissue samples or body fluids of the patient are examined (by polymerase chain reaction, PCR).
Toxoplasmosis: treatment
Toxoplasmosis, which has no symptoms or only mild lymphadenopathy, does not need to be treated. But a treatment is absolutely necessary with:
- clear clinical symptoms
- immunocompromised patients
- a primary infection in pregnancy
- Newborns who have become infected with the parasite in the womb (congenital toxoplasmosis)
The toxoplasmosis therapy is usually carried out with special antibiotics and / or antiparasitics such as sulfadiazine, spiramycin and pyrimethamine.
Toxoplasmosis & pregnancy
If a woman becomes infected with toxoplasmosis during pregnancy, there is a risk that she will transfer toxoplasma to the unborn child. This so-called transmission risk increases with the duration of pregnancy: In the first trimester of pregnancy (1st trimester) it is about 15 percent and then increases to about the last third of pregnancy to about 60 percent. At the same time, however, the danger of serious complications is reduced. The danger for the unborn baby depends on the time of the infection.
Toxoplasmosis infection in early pregnancy
Toxoplasmosis infection in the first trimester of pregnancy is rare. It either leads to a miscarriage or stillbirth or causes serious damage to the unborn child. These include:
- Enlargement of liver and spleen (hepatosplenomegaly)
- Jaundice (jaundice)
- Myocarditis (myocarditis)
- Pneumonia in the connective tissue layer between the alveoli and the blood vessels (interstitial pneumonia)
- Water accumulation in the cranial cavity (“hydrocephalus”, hydrocephalus)
- Inflammation of the retina and choroid in the eye (chorioretinitis)
- Calcifications within the skull (intracranial calcifications)
Toxoplasmosis infection in later pregnancy
Toxoplasmosis infections in the later pregnancy are usually initially without symptoms. However, many of the affected children will develop over the next twenty years consequential damages like squinting (strabismus), deafness or epilepsy. Also, a psychomotor developmental delay (retardation) is one of the possible late damage of acquired in the womb toxoplasmosis.
Pregnancy: toxoplasmosis studies
In principle, a toxoplasmosis examination is only provided in Germany if there is a reasonable suspicion of an infection. For all women who want to have children or at the latest in early pregnancy but a blood test for toxoplasmosis is advisable. The toxoplasmosis test may be repeated in the course of pregnancy if the woman has become infected in the meantime.
If toxoplasmosis is detected as a primary infection during pregnancy, one must check whether the unborn child is also infected. This usually happens over one Amniocentesis (Amniocentesis): A sample of the amniotic fluid is examined for genetic material of the pathogen.
In exceptional cases, a toxoplasmosis in the unborn child is diagnosed by an examination of the child’s blood: Under ultrasound control, the doctor uses a fine hollow needle blood from the umbilical cord (ultrasound-guided umbilical cord puncture). It is examined in the laboratory for genotype snippets of toxoplasma.
In case of proven congenital toxoplasmosis, the doctor may use Ultrasonic determine if the infection has led to organ changes in the child.
Newborns can be tested for congenital toxoplasmosis by searching for antibodies to toxoplasma in their child’s blood.
Pregnancy: Toxoplasmosis treatment
A primary infection with toxoplasmosis in pregnancy must be treated promptly, Pregnant women up to the 16th week of pregnancy receive the antibiotic spiramycin. Later, a combination of pyrimethamine (antiparasitic) and sulfadiazine (antibiotic) is usually recommended. In addition, folinic acid is added to prevent severe bone marrow damage.
During treatment, the patient’s blood count and liver function are closely monitored.
Treatment of newborns
Newborns born with toxoplasmosis will also receive the three supplements pyrimethamine, sulfadiazine and folinic acid. The duration of treatment depends on the severity of the disease.
Toxoplasmosis: disease course and prognosis
The course of a toxoplasmosis is usually favorable. Only in very rare cases (such as in immunodeficiency) develop serious symptoms such as inflammation of the brain, heart or retina.
If a toxoplasmosis is treated consistently during pregnancy, babies are often born without any special symptoms. However, some have scars on the retina. In addition, some of the children develop symptoms such as attention deficit disorder only after years.
In case of infection with Toxoplasma gondii The body forms antibodies (antibodies) against the pathogen. As a result, sufferers are usually for life against renewed infection withtoxoplasmosis protected.
Additional information
guidelines:
RKI advisor “Toxoplasmosis” of the Robert Koch Institute (2018)