In thyroid hyperfunction (hyperthyroidism) the thyroid gland produces too much of the hormones thyroxine (T4) and triiodothyronine (T3). This manifests itself for example in restlessness and nervousness, weight loss despite cravings and fast heartbeat. Hyperthyroidism is a common disease. It mainly affects women and the elderly. Read all important information about symptoms, causes, diagnosis and treatment of hyperthyroidism.

Hyperthyroidism: short overview
- What does thyroid hyperfunction mean? The thyroid produces too many thyroid hormones. As a result, the metabolic processes in the body are accelerated.
- Common symptoms: Restlessness, nervousness, mood swings, loss of weight despite cravings, rapid heartbeat, increased sweating, moist skin, increased thirst, hypersensitivity to heat, enlarged thyroid (goiter), protruding eyeballs and other eye problems (in Graves’ disease) etc.
- Causes: Graves’ disease (an autoimmune disease), autonomy of the thyroid (independent, uncontrolled hormone production), more rarely: inflammation of the thyroid gland, thyroid cancer etc.
- Treatment: Medicines that reduce the amount of thyroid hormones (antithyroid drugs), radioiodine therapy, surgery
Hyperthyroidism: symptoms
Hyperthyroidism is manifested by a variety of symptoms. The excess of thyroid hormones accelerates the metabolism. Common hyperthyroidism symptoms include:
- Restlessness, nervousness, irritability, mood swings
- sleep disorders
- Palpitations and palpitations (tachycardia) to arrhythmia
- increased blood pressure
- increased sweating
- moist, warm skin
- Hypersensitivity to heat
- increased thirst
- Diarrhea, sometimes vomiting
- Weight loss despite cravings (because the metabolism is accelerated)
- hair loss
- muscle weakness
- Muscle pain and muscle sluggishness
- Trembling (tremor)
- menstrual disorders
- enlarged thyroid (goiter, goiter) in 70 to 90 percent of patients

Very often, hyperthyroidism develops due to a malfunction of the immune system. This autoimmune hyperthyroidism will Graves’ disease called. The affected people develop next to the above symptoms also eye problems (endocrine orbitopathy). Typical symptoms here are:
- Pressure sensation behind the eyes and / or foreign body sensation
- increased tears
- Visual disturbances (double pictures)
- photophobia
- prominent eyeballs (exophthalmos)
The protruding eyes in combination with the often rigid look are popularly called “Glubschaugen” or “Goggle Eyes”. The intensity of the eyeballs does not say anything about the extent of hyperthyroidism: in some people, the eyes are very prominent, although they have only mild hyperthyroidism and vice versa.
The three symptoms of protruding eyeballs, palpitations and goiter are referred to as the Merseburg Trias. “It is typical of Graves’ disease.
Hyperthyroidism in old age is often expressed differently than in younger years: many of the typical symptoms may be absent, and the existing symptoms are usually less pronounced. For example, some of the older patients have only a fast, irregular pulse or lose weight only. Cardiac arrhythmias are sometimes the only symptoms of hyperthyroidism in this age group.
Has hyperthyroidism with existing diabetes (Diabetes mellitus) has yet another effect: Through hyperthyroidism, the metabolism is significantly accelerated. That’s why patients need more insulin than usual.
Hyperthyroidism: treatment
Hyperthyroidism is a serious condition. It should be treated by a specialist, such as an internal medicine specialist or an endocrinologist. The doctor will suggest a suitable treatment for each patient. This depends mainly on the severity of hyperthyroidism. The age and general health of the patient also influence the treatment plan.
Hyperthyroidism: medications
In the drug treatment of hyperthyroidism patients receive “thyroid blocker”, so-called thyreostatics, They ensure that fewer thyroid hormones circulate in the blood. This is what the various antithyroid drugs achieve in different ways. Mostly today in the hyperthyroid therapy so-called thionamides such as carbimazole or thiamazole are used. These antithyroid drugs directly inhibit the formation of thyroid hormones.
During treatment with such drugs, the doctor regularly monitors the blood levels of thyroid hormones in the patient. The elevated hormone levels usually go back within a few weeks. Then the signs of hyperthyroidism improve. If not, usually a different therapy is considered (radio-iodine therapy, surgery).
Is it in the thyroid hyperfunction around Graves’ disease, the antithyroid drugs must be taken for at least one year. In about half of the patients, the thyroid gland then works normally again: After stopping the medication, the symptoms of hyperthyroidism do not return.
For the other around 50 percent of the patients, however. But to give the antithyroid drugs even longer, but makes no sense. In addition, it is not advisable due to the side effects. Instead, doctors recommend that patients receive radioiodine therapy or surgery.
Hyperthyroidism: radioiodine therapy
In this hyperthyroid therapy, the patient receives radioactive iodine. It is either administered with a syringe into a vein or swallowed as a capsule. Radioactive iodine (like normal iodine) is stored in the thyroid gland. Cells that produce more thyroid hormones absorb a lot of it. The decomposition of radioactive iodine produces so-called beta-rays. They destroy the cells. In this way, the hormone production decreases and the metabolism of the thyroid normalizes gradually.
Properly performed, radioiodine therapy poses no danger to other organs in the body. The range of the radioactive rays that arise when decaying the administered iodine is only a few millimeters.
Due to the radiation exposure associated with radioactive iodine therapy, patients should temporarily not have close contact with other people. It usually takes only a few days until the amount of radiation has left the body. In Germany, however, radioiodine therapy is carried out on a stationary basis for safety’s sake. The patients are isolated on a special infirmary, at least for a few days.
Because of the radiation exposure, radioactive iodine therapy is not suitable for pregnant and nursing women.
In many patients, the radioactive iodine therapy develops hypothyroidism: If the treatment destroys too much active thyroid tissue, insufficient thyroid hormones can be produced. The deficiency can be but relatively easy with the intake of hormone preparations (usually levothyroxine, L-thyroxine) compensate.
Hyperthyroidism: surgery
Surgery may be an option for hypothyroidism, for example, if the other therapies do not help or if a large goiter has formed. Even if it is suspected that hyperthyroidism is the result of a malignant tumor of the thyroid gland (thyroid cancer), surgery is performed.
Before the operation, the hormone metabolism of the thyroid gland must be normalized with medication. During the procedure, the patient is then partially or completely removed under general anesthesia. The more thyroid tissue that needs to be excised, the less thyroid hormones can be produced afterwards. The operation can therefore cause hypothyroidism. Patients will then have to take hormone pills for life.
Hyperthyroidism: diet
Diet plays an important role in hyperthyroidism: Due to the “high-speed” metabolism, many patients lose weight. Then it is important to eat enough calories with meals. At the same time, the diet should be balanced and varied. Once the metabolism normalizes (such as with medication), the calorie intake must be throttled again. The best way to discuss patients with their doctor, such as the personal meal plan should ideally look like.
Generally, in hyperthyroidism: patients should refrain from coffee, coke and alcohol, These drinks boost the already highly active metabolism even further.
Hyperthyroidism: more tips
If you have hyperthyroidism, you should be careful not to add too much iodine to your body. This means, for example, that you should not use iodine-containing disinfectants.
Caution is also required in X-ray examinations and magnetic resonance imaging (MRI): sometimes iodine-containing contrast agents are administered in advance. You should therefore inform the doctor about your hyperthyroidism before such an examination. This can then give you additional medication that prevents the absorption of iodine into the thyroid gland. Or he uses a non-iodinated contrast agent for the examination.
If you have a hypofunction due to the treatment of your hyperthyroidism and need to take thyroid hormones, you should have your blood tests regularly examined by the doctor. This allows you to determine on an ongoing basis whether your medications are correctly dosed and whether your thyroid levels are within the normal range.
Hyperthyroidism: causes and risk factors
In hyperthyroidism, the thyroid gland produces too much of two hormones: thyroxine (T4) and triiodothyronine (T3). These hormones affect the heart and circulation and play an important role in the energy metabolism of the body. Produced in excess, they accelerate the metabolism – this runs to a certain extent at full speed.

Why the thyroid gland makes too many hormones can have several causes. The most common are Graves’ disease and thyroid autonomy. In addition, there are also rarer causes of hyperthyroidism.
Graves’ disease (immunohyperthyroidism)
Very often, thyroid hyperfunction is on one Autoimmune reaction of the body due. Physicians speak of an autoimmune reaction when the immune system with its antibodies falsely attacks the body’s own tissue. These antibodies are called autoantibodies.
In Graves’ disease, the immune system forms autoantibodies to the thyroid gland: they stimulate the cells of the organ to produce more thyroid hormones. This creates a hyperthyroidism.
Why the immune system attacks the thyroid is unknown. However, experts suggest that genetic predisposition, mental stress and smoking favor the onset of Graves’ disease.
The disease usually breaks up between the 30th and 50th year of life. Women are affected much more frequently than men. Even in childhood, the disease may occur: Graves’ disease is even the most common cause of hyperthyroidism in children.
thyroid autonomy
In older people, hyperthyroidism usually develops through autonomy of the organ. In other words: The thyroid gland “decides” in parts or as a whole to independently increase hormone production – without continuing to obey the brain as a central control organ. Physicians then speak of thyroid autonomy or functional autonomy of the thyroid gland.
There are three types of thyroid autonomy:
- In the disseminated autonomy the autonomous cells are distributed diffusely throughout the thyroid.
- In the unifocal autonomy There is a single accumulation (= one node) of autonomic cells in the thyroid gland. Such a knot was formerly called “autonomous adenoma”.
- In the multifocal autonomy The thyroid gland has several nodes with autonomous cells.
The most common reason for thyroid autonomy is chronic iodine deficiency: if there is too little iodine, the thyroid gland does not make enough hormones. She then tries to compensate for this through increased growth. It can produce thyroid nodules that produce hormones without control by the brain. If these nodes are large enough, there will be an unrestrained production of hormones with renewed iodine intake in the thyroid gland. This can also occur quite suddenly, for example when affected persons receive large amounts of iodine (for example in the form of iodine-containing X-ray contrast media).
Other causes of hyperthyroidism
One of the rare causes of hyperthyroidism include one Inflammation of the thyroid gland (Thyroiditis) and certain forms of Thyroid, Also who too much thyroid hormone as a drug may be hyperthyroidism (such as hypothyroidism). Doctors call this a “hyperthyroidism factitia”.
Sometimes it is also involved Tumor of the pituitary gland (Pituitary gland) behind: This brain region controls the function of the thyroid gland with its own hormone (thyrotropin = TSH). A pituitary gland tumor can cause increased TSH production. This hormone production in the thyroid is excessively stimulated – a hyperthyroidism arises.
Occasionally, hyperthyroidism is also caused by the fact that the body fed too much iodine becomes. This can happen both with iodine-containing drugs and with iodine-containing contrast agents. The latter are for example administered before X-ray examinations or magnetic resonance imaging (MRI). Even people who consume large quantities of iodine-rich foods over long periods of time (for example, sea algae) can develop hyperthyroidism.
Hyperthyroidism & pregnancy
The pregnancy hormone hCG (chorionic gonadotropin) is similar to the hormone TSH of the pituitary gland. It therefore acts as this stimulating on the hormone production of the thyroid gland. As a result, some pregnant women develop a transient, mild hyperthyroidism. Treatment with drugs (antithyroid drugs) is usually not necessary.
However, if hyperthyroidism persists for several weeks and / or is marked (with palpitations, tremors, etc.), it is probably due to another cause. In most cases, this is Graves’ disease. The hyperthyroidism must be treated then necessarily. Otherwise, it can have serious consequences. These include premature labor, low birth weight, miscarriage and stillbirth and preeclampsia.
Tip: Women with known hyperthyroidism should seek treatment and normalize their hormonal levels before they become pregnant. An optimal thyroid function is important for the healthy development of the child (especially in the first weeks of pregnancy). In addition, an excess of thyroid hormones reduces the likelihood of becoming pregnant.
Hyperthyroidism: examinations and diagnosis
If you suspect hyperthyroidism, the doctor will first discuss it with you To raise medical history (Anamnesis): For example, he inquired about your complaints, any previous illnesses and their eating habits (iodine deficiency!). He is also interested in thyroid disorders in your family. He also asks what medications you are taking and if you have recently had a contrast agent (X-ray, MRI) scan done.
The next step is followed by one physical examination, The doctor will, among other things, scan your neck. So he checks if your thyroid is enlarged and may feel tubercular. He can also measure the circumference of the neck.
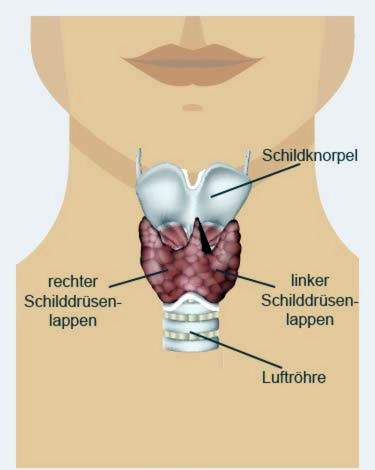
To better examine the thyroid gland, the doctor may ultrasound (Sonography) of the neck. This allows him to assess the location, shape, size and structure of the thyroid more accurately. If Graves disease is suspected, the eye sockets are also examined ultrasonically (by specialist ophthalmologists),
Significant evidence of hyperthyroidism revealed blood tests, The concentration of the thyroid hormones T3 and T4 as well as the TSH (pituitary hormone) is determined. In hyperthyroidism, the T3 and T4 concentration is increased, but the TSH level is lowered. Further investigations help to discover the cause of this hormonal disorder.
If suspected of Graves’ disease, the blood is on special antibodies against the thyroid gland investigated (for example, TSH receptor-stimulating antibodies = TRAK).
With the help of Thyroid scintigraphy the function of the organ can be examined more closely. For this, the doctor injects the patient with a radioactive substance that accumulates in the thyroid, especially in the active, hormone-producing areas. A special camera then takes pictures of the thyroid gland in order to visualize the accumulation of the radioactive substance in the various tissue areas. So the doctor can distinguish between “hot” and “cold” nodes:
- “Hot knots” are areas that are very active (that is, they make up a lot of thyroid hormones) and therefore have accumulated much of the radioactive substance.
- In the “cold knot”, on the other hand, less radioactive substance has accumulated than in the surrounding tissue. These areas are significantly less metabolically active than healthy tissue. The reason is usually a harmless tissue change.
Despite cold knots, hyperthyroidism may be present when other areas of the thyroid gland produce more hormones.
Sometimes the doctor also takes a small one using a thin hollow needle Tissue sample of the thyroid gland (FNAB). It can be examined more closely in the laboratory. For example, it can be determined whether changes in the tissue are benign or malignant. Also, an inflammation of the thyroid gland can be seen in the analysis of the tissue sample.
Severity of hyperthyroidism
Hyperthyroidism is classified according to its severity:
A latent hyperthyroidism is in a sense a hyperfunction in the initial stage: the thyroid hormones (T3 and T4) here still have normal blood levels, while the TSH level is lowered.
A manifest hyperthyroidism is a persistent hyperthyroidism with more or less pronounced symptoms. The blood levels of T3 and T4 are increased here, the TSH level is lowered.
A large excess of thyroid hormone is poison for the body. It evolves one thyrotoxicosis or – in the worst case – one thyrotoxic crisis, The signs range from high fever, palpitations, diarrhea, vomiting, muscle weakness, sweating and consciousness disorders to coma and circulatory failure. Such a life-threatening complication is very rare. It can arise, for example, if hyperthyroidism is not or not adequately treated. Another possible cause is the excessive intake of iodine (such as via contrast media and iodine-containing medications).
A thyrotoxicosis can also occur independently of hyperthyroidism. This can happen, for example, with a thyroid infection or if someone takes a large dose of thyroid hormones (even if he does not need them).
Hyperthyroidism: course and prognosis
If a thyroid hyperfunction is detected and treated in time, the prognosis is good. Graves’ disease is reverted to drug treatment in about half of all patients. However, the disease can also recur after therapy.
By contrast, thyroid autonomy as the cause of hyperthyroidism does not return by itself. The tissue, which independently produces excessive hormones, may even increase over time. A treatment is therefore absolutely necessary. But then those affected can usually lead a normal life.
Will one Hyperthyroidism If detected too late or not treated, complications may arise. These include heart failure (heart failure) and osteoporosis.
Additional information
Books:
- Hyperthyroidism. With more knowledge about the right diagnosis and treatment: Graves’ disease – Hashitoxicosis – hot knots. Thyroid Foundation Book (Irene Gronegger, CreateSpace Independent Publishing Platform, 2015)
guidelines:
- Guideline “Hyperthyroidism” of the German Society of Paediatrics and Youth Medicine (2011)
Support Groups:
- Thyroid League Germany e.V.