Sheath fungus (vaginal mycosis, sokololpitis) is a common fungal infection in women. It is usually caused by yeasts. Typical symptoms include itching and burning of the vagina, as well as a crumbly discharge. The vaginal fungal infection is treated with drugs that are especially effective against fungi (antimycotics). Read here everything important about causes and symptoms of vaginal thrush, diagnosis, treatment and prognosis!

Quick Overview
- What is vaginal fungus? Infection of the vagina with fungi, usually with yeasts (especially Candida albicans). An estimated three out of four women get a vaginal thrush at least once in their lives. The infection can occur at any age.
- Common symptoms: Itching and a burning sensation in the vagina and usually in the pubic area, increased, whitish-crumbly discharge (reminiscent of curdled milk), possibly pain during sexual intercourse; with additional involvement of the urethra also painful urination.
- Treatment: Antifungal agent (antifungals), usually applied externally (cream, vaginal suppositories etc.), only in severe cases also internally (tablets). Possibly antiseptics (generally act against pathogens).
- Forecast: Sheath fungus is usually harmless, but very unpleasant and sometimes persistent. In case of a severely weakened immune system, the fungus may spread in the body and infect internal organs.
Vaginal fungus: symptoms
The most important vaginal yeast symptoms are one strong itching and a burning feeling in the vagina (vagina). Most of the complaints also show in the pubic area (vulva). You can strengthen yourself before menstruation. Incidentally, itching is the first indication of vaginal yeast. It often occurs long before further symptoms.
A characteristic change in vaginal discharge is another sign of vaginal thrush: women always have some discharge. This is often so small that it is hardly noticed. Its amount changes over the course of the menstrual cycle. It is usually transparent to milky and odorless. One intensified, crumbly-whitish discharge is one of the characteristic symptoms of vaginal thrush. He is – like the healthy discharge – odorless.
If the discharge from the vagina smells bad (fishy smell), infected with bacteria and not with mushrooms behind it. Such a bacterial vaginosis must necessarily be treated by a doctor!
Possible vaginal yeast symptoms are too Pain during intercourse (Dyspareunia). If the vaginal mycosis has spread to the urethra, they often come Pain when urinating (Dysuria).
What does vaginal fungus look like?
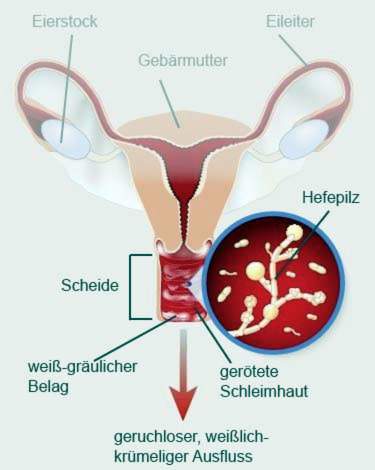
Vagina and pubic can be swollen in vaginal fungus. Often (but not always) there are grayish-white deposits on the mucous membrane at the entrance to the vagina and in the vagina. These pads can be wiped off. Below it shows an inflammatory reddened mucous membrane.
The genital fungal infection of the woman can also lead to small nodules on the skin surface in the genital area.
Vaginal fungus: treatment
Fungal infections can be treated with drugs that are especially effective against fungi – so-called antifungals, For vaginal fungus treatment, antifungals are recommended applied locally become. They are available without prescription in pharmacies and usually contain active ingredients from the group of imidazoles (such as clotrimazole and miconazole) or nystatin. Often, combination packs are offered, consisting of an antifungal cream for use in the outer pubic area as well as vaginal suppositories or vaginal tablets, which are introduced into the vagina. But there are also products that contain only an antifungal cream and an applicator, with the help of which you can introduce the cream deep into the vagina. The use of these local antimycotics is depending on the preparation only once or as a three- or six-day cure.
If this local vaginal yeast treatment does not help, or if the infection keeps returning or flaring up repeatedly, internal (systemic) treatment can be used Antifungals (in tablet form) to be necessary. These medications contain so-called triazoles (such as fluconazole) and are prescribed by the doctor.
Vaginal fungus treatment with antiseptics
Also with so-called antiseptics one can treat vaginal fungus. These are agents that act nonspecifically against many pathogens, but not specifically against fungi. Therefore, they are not as effective as antifungals in the treatment of vagina. Therefore, antiseptics are used especially for mild vaginal or vaginal fungus in the early stages. Even with mixed infections – ie infection with different pathogens – they can be helpful.
The antiseptic agents against vaginal fungus are used locally as an ointment, solution or suppository. They contain the active substance povidone iodine.
For thyroid disorders, povidone iodine should not be used. The contained iodine can cause serious complications in this case!
Pregnancy: What to do with vaginal fungus?
Vaginal fungus in pregnancy should be treated medically. It is recommended to use local antifungals (like antifungal cream) over seven days, Suitable active ingredients are imidazoles such as clotrimazole, econazole or mitconazole. These antifungals are considered to be very effective, well tolerated and safe for the child throughout the pregnancy. Oral antifungals (tablets) must not be taken during pregnancy or only if the doctor considers it absolutely necessary.
In the last four to six weeks before the birth, a medicated vaginal thrush treatment in pregnant women is particularly important. It is important to free the birth canal from all fungi in good time. Otherwise there is a risk that the infection will be transmitted to the child at birth.
In addition to the local antifungal application, pregnant women with vaginal thrush can Doederlein bacteria be administered. These are lactic acid bacteria that belong to the normal vaginal flora. Their application can help to displace the pathogenic fungi in the genital area.
Co-treatment of the partner
Vaginal fungus is contagious. It can be transmitted through direct physical contact between two people, but also over contaminated objects. So if you have a vaginal yeast infection, your partner can easily catch you and develop a penile fungus (see below).
That’s why it makes sense for your partner to be examined as well and treated if necessary. This is especially important if you have a vaginal fungus repeatedly. The co-treatment of the partner helps to reduce the risk of re-infection after successful treatment with the vaginal thrush. Under the foreskin of the penis are often some fungus, but cause no discomfort. However, contact with these may soon be enough to cause a re-infection in the woman shortly after a vaginal yeast treatment.
Home remedies for vaginal fungus
In the media, as well as in the family and friends often different home remedies for vaginal fungus are touted. Although many women are convinced of their effectiveness: Many home remedies harm the vaginal flora rather and do not help at all against vaginal thrush.
Home remedies most commonly recommended for vaginal thrush treatment include yogurt, vinegar and garlic. They should be applied in the outer pubic area or introduced into the vagina. This is supposed to kill the mushrooms. Instead, vinegar, garlic, and other harsh substances disrupt the vaginal milieu, making it even easier for fungi and other pathogens to multiply.
Yogurt is also not recommended in case of vagina fungus: yogurt naturally contains different bacteria. These include lactobacilli (Lactobacilli), which help to maintain a healthy vaginal environment. For this reason, yogurt is a secret against all sorts of vaginal problems. However, yoghurt also contains bacteria that can damage the vaginal flora. Thus, in addition to the vaginal fungus can also develop a bacterial infection (bacterial vaginosis).
Basically: Use the above-described antifungal vaginal fungus drugs from the pharmacy. You can get rid of the infection fairly quickly, especially if used early. Home remedies for vaginal thrush, on the other hand, only aggravate the symptoms.
Other tips for vaginal fungus
- Because vaginal fungus is contagious, you should abstain from sexual intercourse during the infection. After treatment, you and your partner should use condoms at first.
- To prevent spread of the fungal infection, you should only use pH neutral soaps (or even better: only lukewarm water) in the genital area and lubricate the skin regularly.
- Wear air-permeable underwear to prevent the formation of a moist and warm environment in the vagina area – such conditions are ideal for fungal growth.
- Shorten your pubic hair.
- Do not share your towel with others.
- Change your laundry and towels every day and wash them at 60 degrees with a heavy duty detergent.
Often, a sugar-free diet is recommended to “starve” the vaginal fungus. So far, however, could not be proven that this actually works.
penis mushroom
The counterpart to the vaginal fungus in the woman is the penile fungus in the man. It is also usually caused by yeast Candida albicans. The infection is first noticeable with a redness on the foreskin and the glans. Within a few days the tissue swells. Itching, burning and even pain join. In addition, small, liquid-filled bubbles can form on the glans.
Some patients “fetch” the fungal infection through sexual intercourse with a woman with vaginal fungus. However, yeasts – in small numbers – are also part of the healthy skin flora of a man. Under certain conditions, they can proliferate and cause discomfort. This can happen, for example, if the man has a weakened immune system, perhaps as a result of diabetes. Also lack of hygiene in the genital area may favor a fungal infection on the penis.
More about symptoms, causes and treatment of a fungal infection in the male genital area read in the article penile fungus.
Vaginal fungus: causes and risk factors
A healthy vagina is never germ-free, but houses a natural vaginal flora: This consists mainly of lactic acid bacteria (lactobacilli). Some other bacteria and, to a lesser extent, fungi may also (temporarily) be part of the natural vaginal flora. The lactic acid bacteria convert the sugar derived from the sheath cells into lactic acid. This creates an acidic environment in the vagina in which pathogenic germs can hardly multiply.
But if the balance of healthy vaginal flora disturbed, for example, yeasts have the chance to spread – vaginal fungus arises. About 80 percent of all cases of vaginal fungus are caused by the yeast fungus Candida albicans caused. For the remaining 20 percent of the diseases, for example, Candida glabrata or Candida tropicalis are responsible.
Risk factor: sexual intercourse
Sexual intercourse is a common transmission pathway for a genital fungal infection: women and men can infect each other with fungi; in the case of the woman, this can lead to the vaginal fungus, in the case of the man to the penile fungus.
Risk Factor: Weak immune system
A disorder of the vaginal milieu can be due to various causes. Most of the time, a weakened immune system is behind it. This may, for example, be the result of treatment with drugs that suppress the immune system. To these so-called immunosuppressants For example, cortisone and cancer drugs from the group of cytostatics (chemotherapeutic agents).
Also some diseases can weaken the body defense and thus favor a vaginal fungus. This applies, for example, to HIV or AIDS as well as diabetes (diabetes mellitus).
Risk factor: antibiotics
Some women get a vaginal fungus by antibiotics: antibiotics are effective against bacteria in which they inhibit their multiplication or kill the germs. They make no distinction between beneficial and harmful bacteria. An antibiotic therapy can therefore also eliminate the lactic acid bacteria in the vagina and thus trigger a vaginal fungus. The longer the antibiotics are taken, the higher the risk of fungal infection.
Risk Factor: Hormonal Changes
Hormonal changes also lead to a change in the vaginal milieu. They occur naturally in women during the menstrual cycle as well as in the course of life. For example, women after the menopause more susceptible to a vaginal fungus.
Also, the frequent occurrence of vaginal fungus in the pregnancy can be attributed to hormonal changes: These cause in pregnant women, for example, an increased sugar content and reduced acidity in the vagina – ideal growth conditions for mushrooms. The danger is that the fungi can be transmitted to the child during normal (vaginal) birth. The possible consequences are, for example, a fungal infection in the mouth area (oral thrush) or in the diaper area (diaper rash).
A hormone treatment also favors the development of vaginal fungus. For example, some women who use hormonal contraceptives with progestins are prone to fungal infections in the genital area. A treatment with antiandrogens (such as severe acne) is considered a risk factor.
There are also some diseasesthat cause disorders in hormone balance and make them more susceptible to vaginal thrush. These include, for example, hyperthyroidism, hypothyroidism and Cushing’s disease.
Risk Factor: Excessive or poor hygiene
Both an excess and a lack of personal hygiene may favor a vaginal fungus. Excessive personal hygiene can interfere with the delicate balance of the natural vaginal flora, paving the way for a vaginal fungus. Similarly, a lack of personal hygiene can promote the development of fungal infection.
Risk Factor: Wrong clothes
Mushrooms grow particularly well in a warm and moist environment. Therefore, skin-tight clothing and underwear made from synthetic fabrics can promote vaginal thrush: they promote sweating and can cause heat build-up.
Risk factor: stress and mental stress
According to recent research, stress and psychological stress also have a negative effect on the vaginal milieu. They can therefore also promote a vaginal yeast infection.
Vaginal fungus: examinations and diagnosis
If a vagina is suspected, a gynecologist is the right person to contact. He will talk to you in detail first about yours To raise medical history (Anamnese). Possible questions of the doctor are:
- Which complaints do you have exactly?
- Since when do the symptoms exist?
- Have you had such complaints before?
- Have you already done any therapy attempts (for example with over-the-counter antifungals from the pharmacy)?
- Do you have any underlying diseases (like diabetes, HIV)?
- Do you use any medications (antibiotics, cortisone, etc.)?
- Is your partner suffering from a sexually transmitted disease?
After the anamnesis finds one physical examination instead of. The doctor will do the same as with the regular gynecological examination. A vaginal fungal infection can often be recognized by a whitish to grayish deposit on the mucous membrane. If it is wiped off carefully, an inflammatory reddened vaginal mucous membrane comes to light.
To determine which pathogens are responsible for the infection, the doctor takes one Smear of the vaginal mucosa, This can be examined under the microscope. Filamentous structures in the microscopic picture (so-called hyphae) indicate a fungal infection.
Rarely, this microscopic examination gives no clear finding. Then the Germs grown in the smear (pathogen culture): In the laboratory, the smear is placed on a suitable nutrient medium and creates optimal growth conditions for germs, so that they multiply. This makes it easier to identify them.
Vaginal fungus: history and prognosis
With timely and consistent therapy, the prognosis for vaginal fungus is favorable. As a rule, a fungal infection lasts no longer than a few weeks and heals without consequences. Rarely, the infection proves to be very tedious, such as weakened immune system. Under certain circumstances, the vaginal fungus can even spread in the body in very strong immunodeficiency and infect internal organs.
After the healing of a vaginal yeast infection, it can (repeatedly) come to a relapse, if there are still favoring factors such as a false genital hygiene, continued antibiotic therapy or a defense weakness. As far as possible, one should therefore eliminate or reduce such risk factors.
Vaginal fungus: prevention
If you want to prevent vagina, you should avoid or reduce known risk factors as much as possible. This means:
- Avoid synthetic clothing and clothing that is very tight in the genital area and may even be abrasive.
- Wear only underwear made of breathable materials such as cotton. This prevents heat and moisture in the genital area.
- Avoid using plastic-coated panty liners and bandages. Also, they can cause moisture and heat to accumulate in the vaginal area. Perfumed bandages are also unfavorable: the fragrances can irritate the sensitive mucous membrane and thus make them more susceptible to infections.
- Tampons dry out the vaginal mucosa and can thus favor vaginal fungus in sensitive women. Then it can be helpful to change tampons often or switch to breathable sanitary napkins (organic pads).
- Pay attention to a careful but not excessive intimate hygiene. Use only lukewarm water to clean the genital area, or at most pH-neutral or slightly acidic products (syndets), so as not to disturb the vaginal environment. Do without intimate sprays and vaginal douching.
- When using the toilet you should always wipe yourself from the front (vaginal entrance) to the back (anus). If you do it the other way round, fungi could get out of the intestine into the vagina. In this way, according to some experts, a vaginal yeast infection may arise.
In certain cases, a medicinal prophylaxis of vaginal yeast infection make sense. For example, a doctor may recommend women taking diabetes or receiving antibiotic therapy for preventive use of antifungals at intervals (from twice a week to monthly).
Additional information
Guideline:
- Guideline “Diagnosis and Treatment of Candida Infections” by the German-speaking Mycological Society and the Paul Ehrlich Society for Chemotherapy (206)