Coronary heart disease (CHD) is the leading cause of death in Western industrialized countries. Arteriosclerosis (“vascular calcification”) causes a constriction of the coronary arteries (coronary arteries). Coronary heart disease is also referred to as ischemic heart disease, as a constriction in a coronary artery can lead to hypoxia (ischemia) in parts of the heart. Coronary heart disease can cause a heart attack. Read all important information about coronary heart disease here.
Coronary heart disease (CHD): description
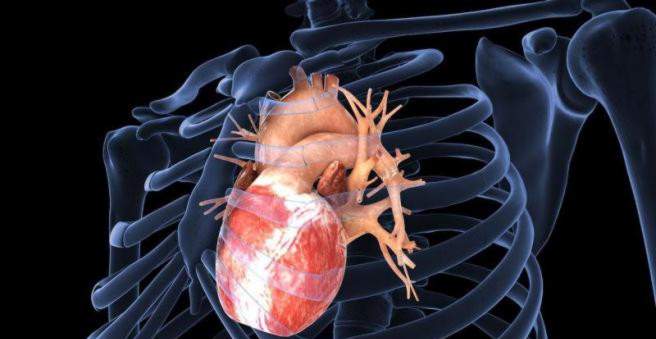
Coronary heart disease (CHD) is a serious heart disease that causes circulatory disorders of the heart muscle. Reason for this are narrowed coronary vessels. These arteries are also called “coronary arteries” or “coronaries”. They surround the heart muscle in a wreath and supply it with oxygen and nutrients.
The cause of coronary heart disease (CHD) is arteriosclerosis (vascular calcification) of the coronary arteries: blood lipids, blood clots (thrombi) and connective tissue are deposited in the inner walls of the vessels. This reduces the inner diameter of the vessel so that blood flow is impeded.
A typical symptom of coronary heart disease (CHD) is chest tightness (angina pectoris), which increases with physical exertion, as there is a mismatch between oxygen supply and oxygen consumption (coronary insufficiency). A heart attack or sudden cardiac death can be triggered by the coronary heart disease. Coronary heart disease (CHD) is one of the most important common diseases and has been leading the cause of death statistics in Germany for years. Coronary heart disease (CHD) is more likely to affect men who, on average, contract earlier than women.
Coronary artery disease: definition
Coronary heart disease (CHD) is defined as a condition in which arteriosclerosis (“vascular calcification”) leads to deficient circulation and thus to a mismatch of oxygen supply and oxygen consumption (coronary insufficiency) in parts of the heart muscle.
Coronary artery disease: classification:
Depending on the extent of arteriosclerotic changes, coronary heart disease can be classified into the following degrees of severity:
- Coronary artery disease – edema disease: One of the three main branches of the coronary arteries is affected by one or more narrow passages (stenoses).
- Coronary artery disease – branch vascular disease: Two of the three main branches of the coronary arteries are affected by one or more narrow passages (stenoses).
- Coronary artery disease – three-vessel disease: All three main branches of the coronary arteries are affected by one or more narrow passages (stenoses).
Coronary heart disease: symptoms
The symptoms depend on how much the coronary arteries are constricted by the coronary heart disease and where the bottleneck is located. Mild constrictions often cause no symptoms. However, when the blood vessels are severely restricted, coronary heart disease causes typical symptoms:
chest pain
Coronary heart disease is typically characterized by chest pain, chest tightness or burning behind the sternum. Doctors refer to this condition as angina pectoris. The coronary heart disease symptoms occur mainly in cases of increased oxygen demand of the heart, that is, during physical or mental stress. The pain in angina pectoris often radiate in the left arm, but sometimes also in the neck, neck, back, jaw, teeth or in the upper abdomen. (“Feeling like a ring around the chest”). Responsible for the pain is an oxygen deficiency in the heart muscle, if the coronary vessels are narrowed in the context of a CHD. If the pain decreases with the administration of the vasodilator drug nitroglycerin, this is a clear indication of the presence of angina pectoris. If a coronary artery is narrowed by 70 percent of its normal width (stenosis), angina pectoris complaints usually occur even at rest. So-called heart bites (short stitches in the chest) are not a specific indication for coronary heart disease.
Arrhythmia
The coronary heart disease often causes cardiac arrhythmias. The lack of oxygen in the heart muscle also affects the electrical impulses (excitation conduction) in the heart. Cardiac arrhythmias due to coronary heart disease can be confirmed by an ECG (electrocardiogram) and evaluated for their potential dangers. Because many people have harmless cardiac arrhythmias and do not suffer from CHD.
Diabetics and the elderly are often symptomless
Some people with CHD, especially diabetics, have no complaints. In this case one speaks of a silent ischemia (deficiency circulation). Most of the nerves in the heart and throughout the body by the diabetes are so damaged that they can no longer pass the pain signals through the coronary heart disease (diabetic neuropathy). The heart muscle is thus damaged without the diabetic noticed. Even in people older than 75 years, the coronary heart disease symptoms may be atypical. For example, you may experience nausea and dizziness without typical chest or left pain.
Coronary artery disease: causes and risk factors
Coronary heart disease (CHD) develops over the years through the interplay of various causes and risk factors. Numerous scientific studies prove that coronary heart disease has a connection with the risk factors mentioned here. Many of them can be avoided by a lifestyle and thus drastically reduce the risk of developing a CHD.
Oxygen deficiency in the heart (ischemic heart disease)
In people with coronary heart disease, the perfusion of the heart muscle is disturbed. The reason for this is a constriction of the coronary vessels by fat deposits or limescale (arteriosclerosis or coronary sclerosis). These deposits are located in the vascular wall of the coronary vessels and form a so-called plaquewhich narrows the vessel diameter at one or more locations. As a result, too little blood flows through the coronary vessels and there is an oxygen deficiency in the heart muscle (ischemic heart disease). It creates a mismatch between oxygen demand and oxygen supply (coronary insufficiency). This is noticeable especially under load. If the diameter of the coronary arteries is reduced by half, usually also circulatory disorders occur.
Influencing risk factors for coronary heart disease:
| risk factor | statement |
| Unhealthy diet and overweight |
Overweight people usually have elevated blood lipids: too much cholesterol and other blood lipids are harmful, because this excess cholesterol particles in the vessel walls of the arteries deposit and there lead to inflammation and calcification. As a result, the vessels become more rigid and narrower. In addition, inflammatory messengers are formed in the abdominal fat, which have a direct harmful effect on the vessel walls and cause coronary heart disease |
| lack of exercise | Sufficient exercise lowers blood pressure, improves cholesterol levels and increases insulin sensitivity of muscle cells. In case of physical inactivity these protective effects are missing and a coronary heart disease can be the result after years. |
| Smoke | Substances from tobacco smoke (cigarettes, cigars, pipes) promote, inter alia, the formation of unstable deposits (plaques) in the vessels. These can come loose and clog a coronary vessel. According to the German Society of Cardiology (DGK), each cigarette shortens life by about 30 minutes. |
| Increased blood pressure | High blood pressure (hypertension) directly damages the vessel walls. |
| Increased cholesterol level | High levels of LDL cholesterol and low levels of HDL cholesterol promote plaque formation, which is of great importance for coronary heart disease. |
| Diabetes mellitus | A poorly controlled diabetes (diabetes) leads to permanently elevated blood sugar levels, which in turn damage the vessels and promote coronary heart disease. |
Uncontrollable risk factors for coronary heart disease:
| risk factor | statement |
| Male gender | Women have a lower risk of coronary heart disease (CHD) before the menopause (menopause), as they are initially better protected by the female sex hormones (especially estrogen). Men are at higher risk for coronary heart disease. |
| Genetic predisposition | Cardiovascular disease is common in some families and genes also seem to play a role in coronary heart disease. |
| Age | The incidence of males rises from the 45th, that of women over the age of 50. The older a person is, the more likely a coronary heart disease is. |
Coronary artery disease: examinations and diagnosis
A coronary heart disease (CHD) is caused by a Specialist in cardiology diagnosed and treated. Also the family doctor is a contact for signs of ischemic heart disease. The anamnesis interview (medical history) is very important for the diagnosis and the follow-up. The physical examination can identify risk factors for coronary heart disease (CHD) and give a rough assessment of overall physical performance. The coronary heart disease is confirmed by various apparatus investigations.
Medical history (anamnesis):
Before the actual examination, the doctor asks a few questions to find out more about the nature and duration of the current symptoms. Possible pre-existing conditions or concomitant symptoms are relevant for the physician. Describe the type, duration and severity of the symptoms and, most importantly, the situations in which they occur. The doctor will ask various questions, for example:
- What complaints do you have?
- When (in which situation) do the symptoms occur?
- Will the pain be more intense during exercise?
- Which medications do you take?
- Are there any similar complaints or a known coronary heart disease in your family, for example with your parents or siblings?
- Has there been abnormalities in your heart in the past?
- Do you smoke? If so, how much and how long?
- Are you active in sports?
- What is your nutrition like? Are you already aware of high cholesterol or lipid levels?
Physical examination
After the anamnesis interview, the doctor will examine you. Particularly important is listening to the heart and lungs with the stethoscope (auscultation). The physical examination gives the doctor a general impression of your physical performance. Some doctors will also press gently on their chest to check whether a musculoskeletal problem (such as spinal or muscular tension) is the cause of your chest pain.
Further investigations:
Whether coronary heart disease is present can be answered unambiguously, especially through targeted measurements and a pictorial representation of the heart. This includes:
Blood pressure measurement
Increased blood pressure (arterial hypertension) is a major risk factor for the development of coronary heart disease. The blood pressure is too high when systolic at rest it is over 140 mmHg and diastolic over 90 mmHg (over: “140 to 90”).
Blood test:
Firstly, the blood and cholesterol values are determined during a blood test. On the other hand, the doctor can check for acute chest pain by certain blood levels (markers: CK, CK-MB, Troponine), if the pain actually come from the heart muscle.
Resting electrocardiogram (resting ECG)
A basic exam is the resting ECG. The electrical potentials of the heart are derived via electrodes on the skin. The coronary heart disease (CHD) can sometimes show typical changes in the ECG.
Stress Electrocardiogram (Stress ECG)
In this variant of the ECG, the electrical potentials of the heart are not recorded at rest, but during physical exertion on a bicycle ergometer. This makes sense, since some pathological changes detectable on the ECG only become apparent when exerted.
Cardiac ultrasound (echocardiography)
With echocardiography you can visualize the size of the heart, the movement of the heart muscle and the pumping function as well as possible heart valve problems. This can be both during physical rest (Resting echocardiography), as well as during physical exertion (Stress echocardiography) respectively. If, for example, due to a pronounced coronary heart disease, no real stress on the patient on the bicycle ergometer possible, the heartbeat can also be accelerated by the administration of a drug (so-called Stress echocardiography)
Myocardial scintigraphy.
In myocardial scintigraphy, a low-level radioactive marker substance is injected into the vein, which, among other things, accumulates in the coronary vessels. The radioactive radiation can be recorded as in a photo and provides information about possible vasoconstriction (stenosis) in the coronary arteries.
Cardiac catheterization (coronary angiography)
For coronary heart disease (CHD), coronary angiography (“heart catheter”) is one of the most important diagnostic and treatment examinations. A thin tube (catheter) is advanced through an artery or artery access to the heart through a large artery , When the catheter tip is in the correct position, an X-ray contrast agent is released and an X-ray image is taken at the same time. In this study you can see the individual coronary vessels very accurately and can also recognize any wall movement disorders of the heart walls. Therapeutically, in the case of a constriction (stenosis), a stent (a tube made of metal) can also be used to hold open or widen the constriction.
Further imaging procedures
In some cases, special imaging techniques are needed to determine the severity of coronary heart disease (CHD). These include:
- Positron emission tomography (PET)
- Cardiac Multilayer Computer Tomography (CT)
- Cardiac Magnetic Resonance Imaging (MRI)
Diagnosis in case of suspected heart attack
If an acute coronary syndrome is suspected, for example a heart attack, an ECG and special blood tests (cardiac troponin) follow immediately. One acute coronary syndrome is a collective term for various phases of acute circulatory disorders of the coronary arteries, which can be directly life-threatening. If either diagnosis is confirmed, a cardiac catheter exam is performed.
Coronary artery disease: treatment
In the case of coronary heart disease (CHD), the main goal of the therapy is to improve the quality of life of patients and stop their progression. In addition, complications such as myocardial infarction are to be prevented. A cure of CHD is not possible. As a rule, however, the symptoms, for example angina pectoris, can be effectively treated and sequelae such as myocardial infarction successfully avoided. As a result, many patients have a similar quality of life to healthy people.
Coronary artery disease may also cause mental illness such as depression. Conversely, mental illness can have a negative impact on coronary heart disease. In the case of coronary heart disease, any possible mental health problems should be considered. In addition to the targeted elimination of risk factors, the treatment of coronary heart disease primarily includes a drug-based and often surgical procedure.
Reduction of risk factors
A regular physical activity of at least 30 minutes daily is useful for patients with coronary heart disease, because among other things, the blood pressure can be lowered and the blood sugar and blood lipid metabolism is positively influenced. Smoking is a major risk factor for coronary heart disease and should be urgently stopped altogether to prevent progression of the disease.
drugs
Coronary artery disease can be treated with a range of medications that not only relieve discomfort (for example, angina) but also prevent complications and increase life expectancy.
Medications that improve the prognosis of coronary heart disease and prevent heart attacks:
- Anticoagulants:Platelet aggregation inhibitors (blood thinners) prevent the deposition of platelets (thrombocytes) and prevent blood clots (thrombosis). First line drug for coronary heart disease is acetylsalicylic acid (ASA).
- Beta-receptor blocker (“beta-blocker”):They lower the blood pressure, slow down the heartbeat, thus reducing the oxygen demand of the heart and the heart is relieved. After a heart attack or CHD with heart failure, mortality risk is reduced. Hypertensive patients probably benefit as well.
- Cholesterol-lowering drugs (for example: statins):The statins lower cholesterol and slow the progression of atherosclerosis. Even patients with normal blood lipid levels benefit.
Medications that relieve the symptoms of coronary heart disease:
- nitrates:They expand the blood vessels of the heart and it is better supplied with oxygen. In addition, they expand the vessels throughout the body, which is why the blood flows back to the heart slower. The heart has to pump less and uses less oxygen. Nitrates are particularly effective and therefore suitable as an emergency drug in acute angina pectoris attack. Under no circumstances should they be combined with anti-impotence agents (phosphodiesterase 5 inhibitors) as this can lead to life-threatening hypotension.
- Calcium channel blockers:This group of substances also dilates the coronary arteries, lowers the blood pressure and relieves the heart.
Other medicines:
- ACE inhibitors:They dilate the blood vessels, lower the blood pressure and relieve the heart. In patients with heart failure or high blood pressure, they improve the prognosis.
- Angiotensin blockers:They are used in the case of an incompatibility of ACE inhibitors.
Cardiac catheterization and bypass surgery
If coronary heart disease is not adequately controlled by medication, an additional dilatation of the coronary arteries (PTCA / PCI) or a bypass operation is possible:
In the Bypass surgery the constriction is bypassed at the coronary vessel. To do this, first remove a healthy vessel from the rib cage or lower leg and sew it behind the constriction (stenosis) onto the coronary vessel. Bypass surgery is particularly useful when the three main trunk of the coronary arteries are severely constricted (three-vessel disease). Although the operation is complex, it improves the quality of life and the prognosis of most people considerably.
In the PCI (Percutaneous coronary intervention, also referred to as PTCA) is stretched as part of a cardiac catheter treatment, first the bottleneck with an inflatable balloon something on. Subsequently, a flexible metal cylinder (stent) is inserted at the constriction in the coronary artery to keep it open. In recent years, more and more drug-coated stents (so-called drug-eluting stents) have been used. These special stents stay longer longer than the usual, uncoated stents.
Coronary artery disease can be treated with bypass surgery or PCR even if multiple coronary arteries are involved or the constriction is at the beginning of a large vessel. The decision for a bypass operation or an expansion is always made individually. In addition to the findings, it also depends on comorbidities and age.
Coronary artery disease: disease course and prognosis
The prognosis of coronary heart disease (CHD) depends, among other things, on how many constrictions exist in the coronary arteries, where they are located and how far the disease has progressed. Also important for the prognosis is whether or not other diseases such as hypertension, diabetes, chronic liver disease, arterial circulatory disorders in other organs (brain, kidney, legs), chronic obstructive pulmonary disease, chronic inflammatory diseases, myocardial insufficiency and malignant tumors are present. It is prognostically unfavorable if a heart attack has already been survived in the past. Also loneliness, depression and a withdrawal from active social life have a negative effect on the prognosis of CHD.
In most cases, it is possible to treat coronary heart disease with medication and – if necessary – by eliminating the bottleneck. In a well-treated coronary heart disease, many sufferers can lead a similar symptom-free life as healthy people. The long-term prognosis for coronary heart disease also depends crucially on whether the person succeeds in his Sustainable lifestyle change, This means: abstinence from nicotine, a lot of exercise, avoiding overweight and a healthy diet. Also important are the continuous intake of prescribed medications and regular check-ups at the doctor.
If coronary heart disease (CHD) is discovered late or treated insufficiently, cardiac insufficiency (congestive heart failure) may develop as a consequence. In this case, the prognosis worsens. An untreated CHD increases the risk of heart attack.
Complication of coronary heart disease: the acute heart attack
Coronary heart disease (CHD) is usually the basis for the development of acute myocardial infarction. In CHD, one or more coronary vessels are narrowed by the so-called plaque formation in the vessel wall. If such a plaque breaks open suddenly (plaque rupture), the blood coagulation is initiated locally and platelets (thrombocytes) attach to the plaque. It comes thereby in a relatively short time to a closure (thrombosis) of the coronary artery. Those parts, which were previously supplied with blood by the now closed coronary artery, suffer from an oxygen deficiency (acute coronary insufficiency) and are thereby damaged.
In acute myocardial infarction usually other symptoms such as shortness of breath, sweating, nausea and agony are added. Suspected a heart attack is the most important measure, as soon as possible Hospital with cardiac cath lab visit. Through a cardiac catheter, the blood flow in the closed coronary artery can often be restored in time and thus greater damage can be averted. An existing one Coronary heart disease is the most important risk factor for the development of a heart attack and should therefore always be treated.