The abbreviation HPV stands for the Human Papillomavirus. The pathogen causes venereal disease and can be felt by warts on the skin and in the genital area. However, most HPV infections heal unnoticed. Nevertheless, malignant tumors can occur long after infection. Man and woman can be equally infected with HPV. Read more about HPV here.
HPV: Quick Reference
- Infection: especially via direct skin or mucous membrane contact (sexual intercourse); it is also possible to transmit viruses via infected objects (toys, towels, etc.) as well as at birth (from the infected mother to the child)
- Sequelae: Depending on HPV type v.a. Nipples, genital warts (genital warts), tissue changes (potential precancerous lesions) and cancer (such as cervical cancer, oropharyngeal cancer, anal cancer)
- Common symptoms: depending on the clinical picture; e.g. in case of genital warts, reddish, brownish or whitish papules in the genital and anal region, possibly with sensation of wetness and itching; in cervical cancer, vaginal discharge and vaginal bleeding
- Important investigations: Physical examination, cell smear, colposcopy (in women), HPV test, biopsy (analysis of a tissue sample)
- Treatment options: Depending on the clinical picture icing, laser therapy, electrocautery, medication, surgical procedures
HPV: causes and risk factors
The human papillomaviruses (HPV) belong to the DNA viruses. Their genetic information is stored on a DNA strand like the human genome. To multiply, HPV viruses require human cells. The infection works like this:
HPV viruses inject their genetic material into a human host cell (skin or mucosal cell) and force them to produce new viruses on an ongoing basis. At some point, the host cell bursts (and dies off), releasing the many new viruses. In turn, they can infect new human cells.
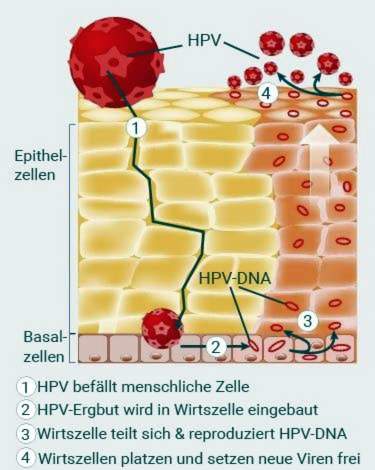
At the same time, in the case of HPV infection, the human genome can be changed so that uncontrolled growths of the skin or mucous membranes (tumors) arise. They can turn into malignant cancer. The risk of cancer depends on the HPV type.
HPV transmission
Many HPV viruses are made by mere skin contact transfer. This is especially true for those pathogens that cause harmless skin warts (papillomas).
HPV types, which infect the genitalia and cause such as genital warts or cervical cancer, are mainly by intercourse transfer. Genital HPV infections are therefore among the sexually transmitted diseases (STD). Also through Oral Sex HPV virus transmission is possible if the oral mucosa comes into contact with HPV-infected skin areas (such as labia or penis). The same applies Body contact while swimming togetherHowever, this is a much less common way of infection.
At least theoretically possible is also an HPV virus infection over infected items like sex toys, towels or the toilet.
Another possibility is the transmission of the pathogen from the mother to the child during birth.
No risk of infection exists according to the current state of knowledge through breastfeeding, normal kissing or blood donation.
Can bein the genital anus area of children Find warts, special attention is needed. Every individual case must be checked and sexual abuse excluded.
risk factors
Probably the most important risk factor of a genital infection results from the mechanism of HPV transmission: frequent and above all unprotected intercourse. Other risk factors for HPV infection are:
- first sexual contacts before the age of 16: This risk factor is especially true for girls.
- Smoke: Cigarettes & Co. not only increase the risk of HPV infection, but also the risk of cells degenerating and developing into cancer cells.
- Births at a young age and several children: When pregnant, the mucosa on the cervix changes and becomes more susceptible to infection. Tissue changes may persist for a few years after pregnancy.
- inconsistent use of condoms: Condoms can not prevent 100% HPV infection. However, consistently using them on sexual contacts reduces the risk of infection.
- suppressed immune systemIf the immune system is compromised due to a disease (such as HIV) or medication (immunosuppressants), the risk of HPV infection increases.
- other genital infections like chlamydia or genital herpes: they also seem to favor HPV transmission.
In addition, some factors increase the risk of HPV-infected cells becoming cancerous cells. These include smoking, many pregnancies, HIV infection and taking the contraceptive pill for five years or more.
HPV: sequelae
The sequelae that HPV infection can cause depends on the type of virus. So far, over 200 different HPV types are known. Most do not cause any symptoms or cause only harmless nipples. About 40 HPV types specifically infect the genital mucosa. They are grouped according to how likely they are to cause cancer:
Low-risk types (low-risk HPV) trigger in an infection hardly dangerous genital warts (genital warts). Although there is also a risk of cancer here, this is very low (low risk). The most common low-risk types are HPV 6 and 11. Other previously known members of this group are HPV 40, 42, 43, 44, 54, 61, 62, 70, 71, 72, 74, 81 and 83.
High-risk types (high-risk HPV) trigger tissue changes (dysplasias, neoplasias) that can develop into a malignant tumor for years, especially cervical cancer (cervical carcinoma). However, HPV infection can also increase the risk of other cancers such as penile cancer or throat cancer. The two major high-risk HPV types are HPV 16 and 18. It also includes HPV viruses 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 (and possibly others).
Some papillomaviruses such as HPV 26, 53 and 66 are more likely to be detected in precancerous lesions. Some authors speak of intermediate HPV. Cancer risk for these HPV types is between the low and high risk types. For example, HPV viruses 5 and 8 are also classified as intermediate HPVs. They are actually really only in defense weakness as well as in Epidermodysplasia verruciformis really dangerous. The latter is a rare hereditary skin disease.
Genital warts (Condylomata acuminata)
Genital warts (pointed condylomas) are benign tissue growths in the genital area and anus. They are transmitted through unprotected intercourse and are usually triggered by the low-risk types HPV 6 and 11, but sometimes also by other HPV representatives. Men and women can get sick.
From the infection with the HPV virus to the appearance of the genital warts (incubation period) can take up to eight months. Condylomas are the most common benign tumors of the external genital and anal regions. They can heal spontaneously, but can persist for months or years.
Condylomata plana
The condylomata plana are flat wart variants of the genital warts on the outer and inner genitals. The causative agents are mainly the HPV viruses 16, 18, 31 and 33. They can lead to cell changes, which are referred to as intraepithelial neoplasms. These cell changes are considered potential precursors of cancer and are classified according to their place of occurrence:
- Cervical intraepithelial neoplasia (CIN): on the cervix (cervix = cervix)
- Vulvar intraepithelial neoplasia (VIN): on the vulva (= labia, clitoris and pubic mound)
- Vaginal intraepithelial neoplasia (VAIN): in the vagina (vagina)
- Penile intraepithelial neoplasia (PIN): on the penis
- Perianal intraepithelial neoplasia (PAIN): in the anus region
- Anal intraepithelial neoplasia (AIN): in the anus
If you want to know more about the development and treatment of condylomata, read the article Genital Warts.
Cervical cancer (cervical carcinoma)
If cervical mucosal cells (cervix) are chronically infected with high-risk HPV types, they can degenerate over time and form a malignant tumor. But this does not happen with every infection, but relatively rarely: According to statistics, less than one in every 100 women infected with a high-risk HPV type has cervical cancer – on average 15 years after the HPV infection.
It therefore takes a long time for the malignant tumor to develop. Women should therefore go regularly to the gynecologist once a year for a check-up: The so-called Pap smear from the cervix can detect suspicious cell changes at an early stage.
Read more about the development, symptoms, treatment and prognosis of cervical cancer in the text Cervical cancer.
Other cancers
In cervical cancer, the association with the HPV virus is clearly proven. But elsewhere, one also studies the carcinogenesis of HPV. For example, oral sex can increase the risk of malignant growth in the throat and throat area (such as throat cancer). Genital and anal cancers such as vaginal cancers, vulvar carcinomas, penile and anal cancers can also be promoted by infection with high-risk HPV types. These cancers are all much less common than cervical cancer.
skin warts
Some HPV viruses cause common skin warts, called verrucae vulgares. They are the most common wart type. There are various special forms of it like the Fleischerwarze. It occurs when working in moist and cold environments with raw meat (ie mainly butchers) and is associated with the HPV virus type 7.
When an infection with HPV causes warts on the sole of the foot, they are usually plantar warts (verrucae plantares). The trigger is usually HPV 1. If there are a lot of warts in the form of warts, dermatologists speak of mosaic warts.
The often occurring in children flat warts are triggered by HPV 3 or 10. Her technical title is Verrucae planae juveniles.
Warts in the mouth
Sometimes individual warts form in the mouth. They are called oral papillomas. Some of them are associated with HPV infection.
If there are warts or wart-like structures in the mouth, it may also be the Heck disease (Heck’s disease or focal epithelial hyperplasia). These benign skin growths are always heaped up and not individually. It is associated with HPV 13 or 32. Heck’s disease is rare among the European population but is more common in other populations, such as the indigenous peoples of Central and South America.
Epidermodysplasia verruciformis
This rare disease is a chronic HPV infection of the skin. According to its discoverers, it is also known as Lewandowsky-Lutz syndrome. It occurs on a family basis and is one of hereditary skin diseases. Due to a genetic defect, the HPV viruses can spread more easily in those affected. Various HPV types play a role in the development of epidermodysplasia verruciformis, including HPV 3, 5, 8 and 10.
HPV: signs (symptoms)
In many cases, the human immune system can fight HPV viruses quite well, with little or no HPV symptoms. In a latent HPV infection, the human papillomavirus can only be detected in the laboratory. In a subclinical HPV infection, the virus-induced skin / mucosal lesions can be visualized only by special techniques.
On the other hand, if visible HPV symptoms are visible to the naked eye, physicians speak of a clinical HPV infection. The signs that trigger HPV viruses depend on the type of virus and the disease.
Symptoms of genital warts (Condylomata acuminata)
Genital warts or pointed condylomas may develop three to eight weeks (incubation period) after infection with certain HPV viruses. It is reddish, gray-brownish or whitish papules of the skin or mucous membrane of the genital and anal region. Their size varies between pinhead size and several centimeters. Often, the individual condylomas are close to each other and form so-called papilloma beds.
In the woman, such HPV signs are found mainly in the labia, at the posterior junction of the two labia majora (posterior commissure) and in the anal region. The genital warts can also develop in the vagina and cervix. In men, these signs of infection with HPV affect the penis and anal region.
Genital warts hardly cause discomfort. However, sometimes wetness and itching, burning and bleeding after intercourse are possible symptoms of HPV-caused genital warts. On the other hand, pain is reported only occasionally.
In rare cases, genital warts that have developed for years become the so-called Buschke-Löwenstein giant condyloma (Condylomata gigantea). These cauliflower-like growths displace and destroy the surrounding tissue. The cells can degenerate and become cancer cells (verrucous carcinoma).
Symptoms of condyloma plana
Those affected develop nondescript, flat raised thickenings (warts) on the outer genitalia, in the anal canal and (in women) in the vagina and cervix. The warts usually occur in greater numbers and are grayish white to reddish colored (like the mucous membrane).
Symptoms of intraepithelial neoplasia
In many people, intraepithelial neoplasia causes no symptoms. This applies, for example, to cervical intraepithelial neoplasia (CIN). In other cases, more or less significant complaints may appear. For example, an intraepithelial neoplasia in the area of the vulva (VIN) may be accompanied by itching, burning and pain during intercourse (dyspareunia), but may also be asymptomatic. An anal or perianal intraepithelial neoplasia (AIN and PAIN) causes itching in the anus, discrete bleeding from the anus and pain during bowel movements. Cell changes on the penis (PIN) can cause a velvety, irregular, shiny redness in the area of the glans or foreskin.
Symptoms of HPV-associated cancer
The most common cancer involved in the development of HPV viruses is cervical cancer. Most affected women show no symptoms at early stages of the disease. In other women vaginal discharge and bleeding after intercourse, between menstrual bleeding or after menopause, indicate a possible tumor disease. However, these symptoms may have other causes.
In advanced stages of cervical cancer, women often report cross-pelvic, urinary or bowel movements. Also, a lymph congestion in the legs can occur.
Sometimes other cancers are linked to HPV. Symptoms depend on the location of the tumor and the stage of the disease. In penile cancer, for example, skin changes such as swelling or hardening of the glans or foreskin, slightly bleeding skin on the penis, and sometimes foul-smelling discharge may occur. Cancer of the vagina is only noticeable at an advanced stage with symptoms such as bloody discharge or vaginal bleeding (eg after sex).
Symptoms of skin warts
Nipples can usually be recognized easily. They usually do not cause discomfort, except for occasional itching, pressure or distension. Warts on the sole of the foot can also cause pain. Sometimes warts (such as plantar warts) have small black dots. It is clotted blood from tiny capillaries of the skin.
Ordinary verrucae are pinhead-sized to pea-sized and have a rough, flaky surface. They form preferably on the back of the hand, on the fingers and nail edges as well as on the feet.
Plantar soles on the soles of the feet are pressed inwards like nails by the body weight when walking or standing. This can cause such pain that those affected can barely walk.
Mosaic warts are about pinhead size and white. They grow especially on the balls of your feet or under your toes. In some patients, they also cover the entire underside of the foot. Because they are shallower than the plantar warts, they usually cause no pain when walking or standing.
The verrucae planae juveniles that occur especially in children are flat, skin-colored warts. They form especially in the face and back of the hand. When children scratch it, they distribute the HPV viruses in a line, so that the warts are often arranged like a line.
Symptoms of warts in the mouth
Oral papillomas are single, cauliflower-like warts in the mouth. They are best found on the hard or soft palate or on the uvula.
In Heck’s disease, several round or oval papules develop on the oral mucosa. Especially children and adolescents are affected.
Symptoms of epidermodysplasia verruciformis
In this disease, generalized, that is, the whole body, abnormally many skin lesions that resemble flat, irregular warts (verrucosis). The slightly scaly papules or plaques are reddish to brownish in color. Especially adolescents are affected, less often older adults. Especially in open, sun-exposed skin regions, the risk of developing skin cancer is significantly increased.
HPV: diagnosis and examination
In most cases, there are no symptoms of HPV infection. For the most part, infection remains unnoticed. However, if the HPV viruses trigger disease symptoms, these are usually typical changes in the skin or mucous membrane. However, some manifestations are so inconspicuous that they can only be made visible through special procedures. As a rule, the necessary examinations are carried out by specialists, that is, depending on the clinical picture, either dermatologists, gynecologists, urologists or ear, nose and throat doctors.
Medical history (anamnesis)
First, the doctor asks the patient about any symptoms that might be related to HPV infection, for example:
- Where exactly are the complaints or skin changes?
- Is there genital itching or burning?
- Did it come to unexplained bleeding?
Since sexual activity plays a crucial role in HPV, the doctor will also formulate specific questions: Was the sexual partner frequently changed? Have you noticed altered mucosal sites, possibly significant warts?
General risk factors such as smoking or medication are also noted. In addition, the doctor asks for known medical conditions. These may weaken the immune system and thereby promote HPV infection.
Physical examination
The doctor usually examines the whole body. Most HPV symptoms, namely warts on the skin, are easily recognized. Further examinations are then usually not necessary. If a skin wart appears suspicious, the doctor removes it and sends it to a laboratory for further examination.
Changes in the female genital area are usually discovered during check-ups. The vagina is scanned and then examined with a speculum (“mirror”). Blanking is important because sometimes speccula cover deep-seated growths that can be triggered by HPV viruses.
HPV-suspicious appearances in the male genital area are usually recognizable and clear to the naked eye. The specialist for this region of the body, the urologist, primarily examines the penile penis, the urethral exit (external urethra meatus) and the enlargement (fossa navicularis) located there. He may spread this point to assess the last two inches of the urethra.
HPV can also be found in the anal area. Since tumors triggered by HPV can reach into the anal canal, some doctors perform a reflection of the anal canal (proctoscopy).
cell smear
In women over the age of 20, gynecologists regularly make a cervical smear for early detection of cervical cancer. By circular motions, the surface of the cervix is first stroked with a type of brush. The second smear takes the doctor from the cervical canal. Then the smears are fixed on a glass plate with the aid of a high percentage alcohol solution, then dyed and examined. This is not a specific HPV smear to detect the virus, but an investigation for suspicious cell changes that may result from HPV infection (or for other reasons).
To assess the possible cell changes is a scale, which was developed by the Greek physician Georges Papanicolaou. Therefore, this investigation is also called Pap test.
colposcopy
Colposcopy is to be understood as an extended reflection of the vagina. In this study, the gynecologist also uses a so-called colposcope (colpo = vagina, scopie = observation), ie a kind of microscope. With up to 40x magnification, the doctor can detect the smallest changes or bleeding on the cervix, cervix, vaginal walls and vulva. In extended colposcopy, the doctor dabbles two to three percent acetic acid on the mucous membrane. Altered upper layers swell up thereby and stand out whitishly from the remaining mucous membrane.
Another step is the so-called Schiller iodine test. The vaginal mucosa is dabbed with an iodine solution (4% Lugol iodine solution). As a result, the healthy mucous membrane turns brown red by the starch contained therein (glycogen). In contrast, cell layers that are altered, for example, by HPV, remain unstained.
biopsy
If the doctor discovers abnormalities during smear or colposcopy, he can specifically remove and examine tissue from the female genital area (biopsy). Depending on the location of the diseased mucous membrane, scrap the tissue sample with a sharp spoon (curettage) or cut a cone (cone) out of the vaginal tissue (conization).
HPV test
This test is designed to detect HPV infection and to identify the type of virus. Its use on the cervix is best tested: The test result helps to diagnose the malignant tumor or its precursors. Much less suitable is the test for detecting HPV infection at other body sites.
The HPV test is available in different variants. For the early detection of cervical cancer, it is currently recommended only in women over 30 years with the Pap test. If a conspicuous Pap test is available at an early age, testing for human papillomavirus may also be useful. In addition, it can help to control the success of treatment after treatment of precancerous lesions on the cervix.
If you would like to know more about the procedure, informative value and costs of this examination, please read the article HPV-Test.
HPV: treatment
Most HPV infections heal spontaneously because the immune cells kill the HPV viruses. Sometimes, however, existing diseases weaken the immune system and thus the fight against HPV. Therefore, they need to be treated.
Generally, the choice of HPV therapy will depend on the nature and extent of HPV symptoms. Disease symptoms such as condylomata or nipples can be treated in different ways. The HPV viruses themselves are rarely completely eliminated. Therefore, relapses often occur.
Icing (cryotherapy)
This possibility of HPV treatment is considered superficial Condylomas and nipples used. The doctor applies liquid nitrogen to the affected area of the skin with the aid of a spray or with a stick (cotton wool, metal), which causes the tissue to die. Sometimes a small bubble forms. The application is usually repeated every one to two weeks. However, the HPV virus survives this procedure. In many cases, new warts are formed as a result.
electrocautery
This treatment is also performed by a doctor. Electrocautery can be like icing Condylomas and warts of the skin be used. The HPV-modified tissue is destroyed by electric current. However, here too, the HPV virus remains in the body and can trigger renewed skin changes at any time.
The electrocautery is also used after an operative wart removal: The directly adjacent skin layers and their vessels are scorched. Although this reduces the risk of relapse, a scar is very likely to form.
Operational procedures
Any HPV symptom can also be treated surgically. Different instruments can be used. First, the affected body region is locally stunned. Then the growths can be excised with a sharp spoon (curettage), a loop electrosurgical excision procedure (LEEP) or a surgical scissors (excision).
In suspicious neoplasms (intraepithelial neoplasms, especially cervical) of the genital mucosa often a whole cone is cut out (conization). However, you usually have to carry out several follow-up checks: The doctor checks every six months how the condition changes. If the conspicuous area increases and high-risk HPV has been detected, removal of the tissue is necessary. If the tumor has already been identified as malignant, it will be operated as soon as possible. However, if the patient is pregnant, the operation is postponed until after birth. Depending on the stage of cancer, the surgeon will expand the procedure accordingly. For example, in advanced cervical carcinoma, the complete uterus is removed (radical hysterectomy).
In some cancer patients, radiotherapy and / or chemotherapy is performed as an alternative or in addition to the surgery.
laser therapy
Also, this option to treat HPV diseases is one of the surgical procedures. The laser (for example CO2– or Nd: YAG laser) is included HPV warts of every kind used. Under local anesthesia, the growths are cut out and evaporated. However, caution is advised: Due to the smoke, the HPV virus can spread easily. Therefore, sufficient protection by suction and filter is particularly important.
Medicines for HPV warts
There are some medications for the treatment of Genital or anal HPV warts, Some are administered by the doctor, others can use patients independently at home against the HPV symptoms. The careful and regular use of the medication is crucial to the success of the therapy. Examples:
|
drug |
user |
Remarks |
|
Podophyllotoxin 0.15% cream |
patient |
|
|
Imiquimod 5% cream |
patient |
|
|
trichloroacetic |
doctor |
|
In principle, there is a high risk of relapses (recurrences) in HPV infections. Therefore, you should carefully monitor the treated areas and consult the doctor at regular intervals.
HPV: disease course and prognosis
The classic course of an HPV infection does not exist. Often it goes unnoticed and heals without consequences. If HPV symptoms occur, spontaneous healing is also possible. As a general rule, most HPV infections heal within a few months. After two years, even about 90 percent of all HPV infections are cured.
Only a few patients keep certain HPV viruses longer and even lead to cancer. This can happen years or decades after HPV infection.
Healed HPV infection provides no protection against reinfection with the pathogens.
HPV: Prevention
It is often discussed how to protect against HPV infection. Prevention is not easy, because HPV viruses are very common and therefore the risk of infection is very high.
In general, it makes sense to pay attention to thorough hygiene and to strengthen the immune system. Um das Risiko einer Ansteckung mit normalen Hautwarzen zu verringern, sollte man zudem in Schwimmbädern, Sauna-Anlagen, öffentlichen Umkleidekabinen und Hotelzimmern nicht barfuß herumlaufen. Wenn im Umfeld jemand Warzen hat, sollte man sich mit diesem Menschen beispielsweise nicht das Handtuch, den Waschlappen oder die Socken (bei Warzen an den Füßen) teilen.
Zur Vorbeugung von HPV-Infektionen im Genital- und Analbereich sollte man vor allem bei häufig wechselnden Geschlechtspartnern immer ein Kondom verwenden. Einen sicheren Schutz vor HPV bietet Safer Sex zwar nicht, weil das HPV-Virus schon durch Schmierinfektion übertragen werden kann. Allerdings können Kondome das Ansteckungsrisiko reduzieren.
Es gilt als gesichert, dass das Risiko für HPV bei Männern, die beschnitten sind, niedriger ist als bei nicht-beschnittenen.
HPV: Impfung
Die Ständige Impfkommission (STIKO) des Robert Koch-Instituts empfiehlt, alle Mädchen und Jungen zwischen zwischen neun und vierzehn Jahren gegen HPV zu empfehlen (am besten vor dem ersten Geschlechtsverkehr). Wer mit 15 Jahren noch ungeimpft ist, sollte die Impfung bis spätestens zum 18. Geburtstag nachholen.
Die HPV-Impfung dient in erster Linie dazu, das Risiko von Gebärmutterhalskrebs zu senken. Außerdem kann sie das Risiko für einige weitere Krebserkrankungen verringern (Scheidenkrebs, Peniskrebs etc.) und bei beiden Geschlechtern der Entstehung von Genitalwarzen (Feigwarzen) vorbeugen.
Wie lange der Impfschutz anhält, ist bislang noch nicht genau bekannt. Studienergebnisse deuten darauf hin, dass geimpften Mädchen/Frauen auch 12 Jahre nach der Impfung noch wirksam vor einer HPV-Infektion geschützt sind. Noch lässt sich abschließend aber nicht sagen, ob der Impfschutz nicht doch irgendwann aufgefrischt werden sollte.
Mehr über die Durchführung, Wirksamkeit und Kosten dieser Impfung gegen HPV lesen Sie im Beitrag HPV-Impfung.
Support Groups
Krebsinformationsdienst: Krebs-Selbsthilfegruppen und Patientenverbände