Endometriosis is when cells of the uterine lining outside the uterine cavity (cavum uteri) settle. While the condition is benign, many suffer from severe menstrual cramps, abdominal pain between menstrual periods, pain during intercourse, and infertility. Read here everything important about symptoms, causes, diagnosis, treatment and prognosis of endometriosis!

Endometriosis: short overview
- What is endometriosis? One of the most common abdominal disorders in women. The uterine lining also settles outside the uterine cavity, on the ovaries or between the uterus and the rectum. Sexually mature women are usually affected. Only rarely does endometriosis become noticeable before the first or last menstrual period.
- Causes: Unknown, but there are various assumptions, such as mucosal cells with backward-flowing menstrual blood through the fallopian tubes into the abdominal cavity or that a malfunction of the immune system is involved in the pathogenesis.
- Symptoms and consequences: Some patients have no complaints. Others report severe menstrual pain, abdominal pain regardless of menstruation, pain during intercourse, urination or defecation. The illness can be very stressful and can be associated with infertility.
- Treatment options: Medicines (pain killers, hormone preparations), surgery; supportive often complementary methods (such as relaxation techniques, acupuncture, etc.)
- Forecast: Endometriosis is usually chronic. The course is unpredictable. Endometriosis herds can both spontaneously regress and spread. A therapy can usually relieve the symptoms, but often it comes afterwards to relapses. With the onset of menopause, the endometriosis usually comes to rest.
Endometriosis: description
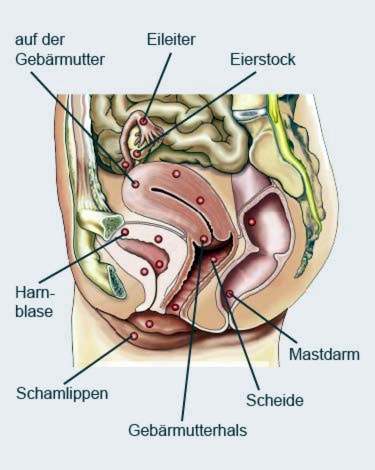
Endometriosis (English: endometriosis) causes scattered cell aggregates Uterine lining (endometrium) outside the uterine cavity on. These cell islands will be Endometriosis herd called. Depending on their location, doctors distinguish three major groups of endometriosis:
- Endometriosis internal genital: Endometriosis foci within the muscular layer of the uterine wall (myometrium). Doctors speak of this adenomyosis (Adenomyosis uteri). In addition, endometriosis foci in the fallopian tube belong to the group endometriosis genitalis interna.
- Endometriosis genitalis externa: Most common form of illness. Endometriosis foci in the genital area (in the pelvis), but outside the uterus, for example in the ovaries, on the uterus or in the Douglas space (depression between the uterus and the rectum).
- Endometriosis extragenitalis: Endometriosis foci outside the small pelvis, such as in the intestine (endometriosis), in the bladder, in the ureters or – very rarely – in the lungs, brain, spleen or skeleton.
The endometriosis foci are estrogen-dependent and behave like the mucous membrane within the uterine cavity: they become alternating during the menstrual cycle built up and repelled (with a little bleeding). The cell remains and the blood can not be excreted – as with the regular mucous membrane in the uterine cavity – over the vagina. Sometimes, the body can easily and unnoticeably remove it (take in the surrounding tissue and break down).
Often, however, tissue remnants and blood dissolve the endometriosis foci Inflammations and adhesions or adhesions that can cause more or less severe pain. In addition, so-called Chocolate cysts (endometriomas) form, on the ovaries, for example. Cysts are fluid-filled cavities. In endometriosis patients, these cavities are filled with old, clotted blood and thus appear brownish. That’s why the name chocolate cysts.
Endometriosis: frequency
Endometriosis is considered to be widespread. However, there is no reliable information on the exact frequency – especially since the endometriosis herd in many cases cause no discomfort and then often go undetected. However, physicians estimate that there are approximately 40,000 new cases a year in Germany.
It usually takes a long time to detect endometriosis: in Germany, an average of ten years elapse between the onset of the first symptoms and the diagnosis.
Endometriosis in men is extremely rare.
Endometriosis: symptoms and consequences
The scattered islets of uterine lining often cause more or less severe symptoms in affected women. However, endometriosis can also remain completely without discomfort. The following are the main symptoms that can occur in endometriosis, as well as possible consequences of the disease:
Strong menstrual pain: In endometriosis, the pain and cramps just before and during menstruation can be particularly severe. Physicians then speak of dysmenorrhea. Especially endometriosis foci in the uterine muscles can cause severe pain. In some women, the menstrual pain is so severe that they can not do their job and have to take strong painkillers.
Other abdominal pain: More or less severe pain in various parts of the abdomen may occur in endometriosis independently of the menstrual period. Sometimes these pains radiate into the back or legs. The symptoms can be caused by adhesions between various organs in the abdomen, such as between the ovary, intestine and uterus. Sometimes the solidified and less elastic structures trigger persistent pain. In addition, endometriosis foci can release inflammatory substances that additionally irritate the tissue and can lead to pain.
Pain during intercourse: Pain during sex (dyspareunia) – sometimes only afterwards – are also common endometriosis symptoms. They are often described by the affected women as burning or spasmodic. Cause are often Endometriose herd on the elastic straps, which “anchor” the uterus in the small pelvis: You can trigger pain when the pelvic organs move during sexual intercourse as usual. The symptoms can be so severe that affected women completely abstain from sex. That can weigh heavily on a partnership.
Pain when urinating or defecating: Rarer endometriosis symptoms are painful urination as well as bloating and pain during bowel movements. They are caused by endometriosis foci in the bladder or intestine. Sometimes, depending on the cycle, blood infusions also occur in the urine or stool.
Fatigue and exhaustion: Strong and / or frequent endometriosis symptoms can be physically very stressful in the long term. General fatigue and tiredness are possible consequences.
Mental stress: In addition to physical stress endometriosis often means a psychological burden. Many affected women suffer emotionally from the severe or frequent pain. This is especially true when countless visits to the doctor are necessary before the cause of the complaints is established – which unfortunately happens very often.
The extent of endometriosis complaints is not related to the stage of the disease! For example, women with few / small endometriosis herds may be in greater pain than patients with more extensive herds.
Infertility: Many women with endometriosis can not get pregnant. The exact reason for this is unknown. However, there are indications that egg development and early embryonic development may be disturbed in the patients. For more on the causes and treatment of unwanted infertility in endometriosis, see Endometriosis & Fertility.
Cancers: Endometriosis is a benign condition and is not associated with a generally elevated risk of cancer. However, a malignant tumor can develop on the bottom of endometriosis (usually ovarian cancer). But that happens only very rarely.
In addition, it has been observed that endometriosis sometimes occurs in association with various cancers. These include, for example, renal cell carcinoma (the most common type of kidney cancer), brain tumors, black skin cancer (malignant melanoma), non-Hodgkin’s lymphoma (forms of lymphoma) and breast cancer (breast cancer). However, the clinical significance of this observation is unknown.
Endometriosis: treatment
Endometriosis therapy always depends on the extent of the symptoms. A randomly detected endometriosis that does not cause any problems does not necessarily have to be treated. A treatment is advisable with:
- persistent pain,
- unfulfilled desire for children and / or
- an endometriosis herd disorder of organ function (ovary, ureter, intestine, etc.).
Be used surgical and / or medicinal therapy, How this endometriosis treatment looks in each individual case depends on several factors. In addition to the extent of the complaints, the location of the endometriosis herd and the age of the woman play a role. In addition, the doctor takes into account in the treatment planning, whether the patient still wants to have children or not.
In addition to surgery and / or medication can psychosomatic therapy Emotional problems and psychosocial stress can increase the pain in endometriosis or, conversely, can be caused or at least promoted by the disease. This can create a vicious circle that severely limits the patient’s quality of life. An early support and advice (such as a psychologist, pain therapists, sex consultants, etc.) can counteract this.
Drug endometriosis treatment
You can take various medications in endometriosis that serve different purposes: Painkillers are used to alleviate pain and cramping in the abdomen. In contrast, hormone preparations can slow down the growth of endometriosis foci.
Painkiller: Many endometriosis patients take so-called non-steroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid (ASA), ibuprofen or diclofenac. These agents have been shown to help with severe menstrual pain. Whether they are also effective in other endometriosis pain has not yet been scientifically proven. Possible side effects of NSAIDs include stomach upset, nausea, headache, and a blood clotting disorder. The preparations should therefore not be taken more often or for a longer period without medical supervision.
For very severe endometriosis pain the doctor sometimes prescribes so-called opioids, These are in principle very potent painkillers. However, their efficacy in endometriosis pain has not been conclusively proven. In addition, opioids can cause side effects such as nausea and vomiting, constipation and blood pressure fluctuations. With prolonged use there is also the danger that a dependency develops.
Hormone treatments: Hormonal endometriosis treatment is suitable for patients who do not want to have children. The hormones administered suppress hormone production in the ovaries and thus ovulation and menstruation. Above all, the production of estrogens is inhibited. Because the endometriosis foci are estrogen-dependent, they are “sedated” during hormone therapy. The complaints subsided. So far it is unclear whether the hormone treatment can also cause the Endometriose herd to regress and the endometriosis completely disappears. Various hormone preparations are used:
Sometimes the doctor recommends certain endometriosis patients hormonal contraceptives like the anti-baby pill or the contraceptive patch. Some anti-baby pill supplements can be taken continuously (without a break). This can be beneficial in endometriosis, because the withdrawal bleeding (bleeding after the end of a cycle of taking = a pill package) can be very painful for the patients. This long cycle is not officially approved in Germany, so it is “off label”.
Other hormone preparations that can be used for endometriosis therapy are so-called GnRH analogues, Just like hormonal contraceptives, they can relieve endometriosis symptoms. However, they have stronger side effects: It comes to symptoms that often occur during menopause (mood swings, hot flashes, sleep disorders, dry vagina). In addition, GnRH analogs can reduce bone density with prolonged use.
Progestin (Yellow body hormones) such as dienogest or dydrogesterone can also relieve endometriosis pain. In tablet form, they are taken continuously. If the pain persists even after an endometriosis operation, a progestogen-containing spiral (hormone spiral with levonorgestrel) may be inserted into the uterus. Sometimes this helps better against the discomfort than the surgery alone. Possible side effects of progestins include bleeding, headache, mood swings and reduced sexual interest (loss of libido).
Operative endometriosis treatment
Surgery may be indicated if endometriosis causes severe discomfort and / or infertility. Even with “chocolate cysts” of the ovaries, an intervention usually can not be avoided (a sole hormone treatment is not enough here). The same applies if the endometriosis has infested the intestine or the bladder and disturbs the function of these organs.
If endometriosis has become deeply embedded in the tissues of other organs (such as the vagina, bladder, bowel), the operation should be performed in clinics where there is much experience with such procedures.
The aim of an operation in endometriosis is to remove as far as possible the dislocated uterine lining islands – by laser, electric current or scalpel. Sometimes it is also necessary to remove some of the affected organs (fallopian tubes, etc.). The procedure usually takes place within the framework of a laparoscopy (Laparoscopy). Rarer is a big one laparotomy (Laparotomy) necessary.
When endometriosis causes very severe discomfort, other treatments fail, and there is no wish to have children, some women choose a complete one Removal of the uterus (Hysterectomy). Sometimes the complaints stop, but not always. Then maybe the Ovaries removed, This deprives all endometriosis herds of estrogen necessary for growth (ovaries are the major production sites of these hormones).
The removal of the ovaries, however, suddenly puts the patient into the menopause. Therefore, this radical intervention should be considered very carefully. If after the surgery very severe menopausal symptoms occur, the woman may take estrogen supplements against it. However, these can also cause the endometriosis symptoms to return.
Medicines plus surgery
Sometimes, drug and surgical endometriosis treatment are combined: Before and / or after a laparoscopy, patients receive hormone preparations (usually GnRH analogues). The pre-treatment with hormones should minimize the endometriosis herd as possible. Post-operative hormone treatment should calm remaining endometriosis foci and prevent the formation of new foci.
So far, however, it has not been proven in studies that a combination of hormone treatment and laparoscopy is actually more promising than a single surgery – neither in terms of pain nor the chances of getting pregnant. In addition, the hormone treatment caused side effects in some patients.
Endometriosis: Complementary therapies
Some women with endometriosis use alternative / complementary therapies for their complaints. The spectrum ranges from medicinal plants and homeopathy to acupuncture, relaxation and movement techniques (such as yoga or tai-chi) as well as psychological pain management training to chiropractic treatments and TENS (transcutaneous electrical nerve stimulation). Also a lifestyle change (more exercise, stress reduction, etc.) should be helpful.
Such alternative / complementary therapies can actually improve the symptoms and quality of life of some patients, even if scientific evidence of efficacy is lacking. Anyone interested in such procedures should discuss their use and possible side effects with an experienced physician or therapist.
Tip: Endometriosis pain can sometimes be relieved with heat applications, such as a hot water bottle, a heat pack or a warm bath. Heat has a calming, relaxing and antispasmodic effect.
Endometriosis: causes and risk factors
Exactly how endometriosis develops is still unclear despite intensive research. But there are different theories about it. One of them is the so-called Carryover or transplantation theory:
It assumes that cells of the uterine lining are removed from the uterine cavity to other parts of the body. This should be done either via the circulatory system or via a “reverse” (retrograde) menstruation – ie via a return flow of menstrual blood via the fallopian tubes into the abdomen. In fact, it is known that new out of ten women experience such retrograde menstruation. So theoretically it would be conceivable that this way mucosal cells of the uterus get into the abdomen.
A contrast to transplantation theory forms the Metaplasia theoryAccording to her, the mucosal cells of the endometriosis foci are formed directly on the spot (in the ovaries, for example), so they are not transported there from the uterus. Instead, for unknown reasons, they are supposed to develop from localized cells that have emerged from the same embryonic cell line during development in the womb as the uterine lining cells. This could explain why endometriosis can also occur in men (but extremely rare) – the original embryonic tissue is also found in them.
Other factors could contribute to the development of endometriosis, for example, a Disturbed interaction of hormones, Also one Malfunction of the immune system is discussed: Normally, the immune system namely ensures that cells from a particular organ can not settle on other parts of the body. In addition, antibodies in the blood of some patients can be detected against the endometrium. These antibodies cause inflammation in the area of the endometriosis herd. However, it is not yet known whether these antibodies are the cause or the result of endometriosis.
Genetic factors could also play a role in the development of endometriosis. Sometimes the disease occurs in several women within a family. However, there is no evidence that endometriosis is directly inheritable.
Endometriosis & childbearing
Many women with endometriosis try in vain to get pregnant. In such cases, experts generally recommend an operation: removing the dislocated uterine lining surgically can increase the chances of getting pregnant.
On the other hand, this can not be achieved with a drug endometriosis treatment alone. Also, hormone treatment with GnRH analogs after surgery can not improve the fertility of patients.
In some women, new endometriosis foci are formed after surgery, so pregnancy is still absent. Then should not be operated again. Instead, experts advise women to try artificial insemination.
Read more about infertility in endometriosis and the different treatment options in the article Endometriosis & Fertility.
Endometriosis: examinations and diagnosis
If suspected endometriosis, women should go to the gynecologist. This will be the first in a detailed conversation To raise medical history (Anamnesis): He can be described, among other things, the symptoms (severe menstrual pain, pain during intercourse, etc.) exactly. He also asks how long they have been and how much they affect everyday life and a possible partnership. In addition, the doctor asks if an endometriosis has been detected in the family (such as the mother or sister).
Endometriosis often causes no complaints. It is then discovered (if at all) only by chance, for example when a woman is examined more closely for unwanted childlessness.
The next step is one gynecological check, This includes scanning the abdominal wall, vagina, cervix and rectum. This can give him indications of possible pain, hardening or adhesions in these areas.
Valuable information can also be provided by the doctor Ultrasound examinations via the abdominal wall and via the vagina (transvaginal ultrasound). It can thus often detect larger endometriosis foci as well as cysts and adhesions. Ultrasound via the vagina is particularly suitable for detecting cysts of the ovaries. Transvaginal ultrasound is also necessary if there is a suspicion of endometriosis foci in the muscular uterine wall (adenomyosis).
If the physician suspects endometriosis infestation of the urinary tract, he will also examine the kidneys by means of ultrasound: If the endometriosis foci constrict the ureters, the urine can back into the kidney and damage the organ.
If you suspect endometriosis, the doctor also often takes one tissue sample suspicious areas and have them examined histologically in the laboratory. The sampling usually takes place via a laparoscopy (Laparoscopy). The tissue examination can show if it is indeed an endometriosis or perhaps another (possibly malignant) disease.
In some cases, in endometriosis further investigations make sense. For example, in the case of suspected infestation of the bladder or the rectum, a bladder reflection or an endoscopy can bring clarity. Very rarely, other imaging techniques (magnetic resonance imaging, computed tomography) are used in addition to ultrasound.
Endometriosis: history and prognosis
Endometriosis is usually chronic. How it develops in a particular case can not be predicted. In some women, the endometriosis herds spontaneously recover without treatment. In others, the disease progresses: The scattered mucosal islands grow steadily, spread and can affect various organs. This may necessitate repeated operations.
With the right therapy, the symptoms of endometriosis can be alleviated in most cases. However, the absence of symptoms is not always permanent: If endometriosis has been successfully treated with hormones, the symptoms often return after the medication has been discontinued. Surgery is also not a guarantee of ongoing symptom-freeness: nearly four out of five women develop new endometriosis foci within five years of surgery.
With the onset of menopause comes the endometriosis but for most women to rest.
Additional information
Books:
- Endometriosis: Advice and Help for Concerned and Relatives (Rat & Hilfe), Ewald Becher and Adolf Schindler, Kohlhammer W., GmbH, 2010
- How we live with endometriosis – Everyday life with chronic abdominal disease: a companion book for affected women, their families and medical contacts, by Kathrin Steinberger, edition riedenburg, 2013
Guideline:
- S2k Guideline for the “Diagnosis and Therapy of Endometriosis” of the German Society for Gynecology and Obstetrics (2013)
Self-help:
- Endometriosis Association Germany e.V. & # x202f;
- Network endometriosis