In arteriosclerosis, the arteries narrow due to deposits. The result: The blood flow is limited or at worst completely interrupted – then threatens an infarction. Older people are more likely to be at risk of atherosclerosis, but lifestyle factors such as a high-fat diet or lack of exercise also increase the risk of atherosclerosis. Here you will learn everything important about risk factors, consequences and prevention of atherosclerosis.
Atherosclerosis: description
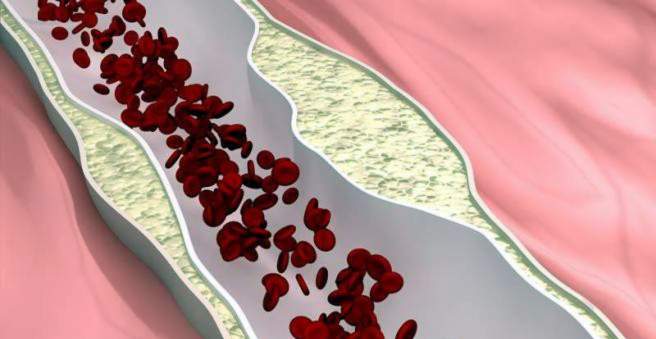
Arteriosclerosis, colloquially known as arteriosclerosis, is a disease of the arteries. These blood vessels carry oxygenated blood from the heart to the organs, muscles and tissues. In arteriosclerosis patients, blood fats, blood clots, connective tissue or lime are deposited in the vessel walls. These deposits are called plaques.
In principle, arteriosclerosis can develop in all arteries of the body, but it is preferably produced in certain vascular regions in the neck, the brain, the heart, the pelvis or the epididymis. Particularly frequently affected are sites where the blood flow physically encounters obstacles – for example, branching of vessels. The result: The blood vessels become narrower and lose their elasticity.
As a result, the blood can no longer flow unhindered. In the worst case, a plug of platelets (thrombus) forms on the plaques. Then an infarction threatens. The vascular wall can be weakened by arteriosclerosis but also so that it expands and aneurysm arises. Sequelae of atherosclerosis are the leading cause of death in the western industrialized nations.
Atherosclerosis: symptoms
Arteriosclerosis develops slowly – often symptoms only appear after years to decades. If the disease starts in adolescence, 30- to 40-year-olds already have complaints. Often, however, the symptoms of atherosclerosis occur only at a higher age. How the disease manifests depends on which vessels in the body are affected.
Are the Coronary artery Narrowed, one speaks of the so-called coronary heart disease. Symptoms are caused by the reduced blood flow to the heart muscle. Patients feel chest tightness or left-sided chest pain (angina pectoris). If a blood clot closes an already constricted vessel, it can lead to a heart attack.
Is the blood flow in the Carotid artery and its branches disturbed or the carotid artery is blocked by a blood clot, a stroke can be the result. It comes to functional disorders of the nervous system such as paralysis or speech disorders.
Also Arteries in the pelvis and the legs can be narrowed by arteriosclerosis. The so-called peripheral arterial occlusive disease (PAOD) is caused by circulatory disorders in the thighs and calves. Already after short walking distances muscle aches occur. Because sufferers have to take frequent pauses, one speaks also of the intermittent intercurrent claudication (Claudicatio intermittens). Arterial narrowing in the pelvis can also lead to impotence in men.
Arteriosclerosis in the renal vessels causes symptoms of impaired kidney function and high blood pressure. In the worst case it comes to kidney failure.
Atherosclerosis: causes and risk factors
How arteriosclerosis arises exactly is not yet known. Immediate cause is the damage to the inner vessel wall layer, which forms a fluid accumulation in the vessel wall. This favors an accumulation of fats and lime particles. What causes this damage to the arteries is something the experts disagree about. There are therefore different theories for the mechanism of arteriosclerosis formation.
Lipoprotein-induced-atherosclerosis hypothesis for the development of arteriosclerosis
There are two forms of cholesterol: “good cholesterol”, HDL for short, which removes fat from the body and brings it to the liver, where it is broken down; and the “bad cholesterol,” LDL. The latter transports fat from the liver to the body’s cells. The fat can then be stored in the inner walls of the arteries and trigger an inflammation there. This causes plaque formation: white blood cells migrate into the vessel wall and absorb as much LDL as possible. The immune cells swell to so-called foam cells, causing more defense cells on the plan, releasing the pro-inflammatory substances. Together with blood cells and foam cells they form a growing “fatty streak” in the arterial wall – the basis for arteriosclerotic plaques.
Response-to -injury hypothesis on the development of arteriosclerosis
The trigger for arteriosclerosis according to this hypothesis is a mechanical injury to the inner arterial wall layer. It can arise, for example, from hypertension. The body responds to the injury with growths and the formation of foam cells – herd-shaped plaques arise.
Infection hypothesis for the development of arteriosclerosis
According to this explanatory model, the inner wall of the vessel is damaged by poisons of certain bacteria, viruses or immune reactions.
Atherosclerosis risk factors
Older people are more likely to suffer from arteriosclerosis. Diet, physical inactivity, smoking, metabolic diseases such as diabetes and other factors promote disease development in all age groups. The most important risk factors:
- Fat and high calorie foods lead to high LDL cholesterol and obesity – both factors increase the risk of arteriosclerosis.
- Lack of exercise can raise blood pressure and worsen cholesterol metabolism.
- High LDL cholesterol levels promote plaque formation.
- Increased blood pressure directly damages the inner walls of the vessel.
- Fabrics off tobacco smoke Among other things, it promotes the formation of so-called unstable plaques. These are deposits in the arteries that can break loose.
- Diabetes mellitus (Diabetes) causes permanently increased blood glucose levels to damage the vessels (angiopathy), especially if the disease is not treated adequately.
- Chronic kidney failure can lead to a special form of arteriosclerosis, called mediasclerosis. The muscle layer of the arteries calcifies very strongly.
- Hyperthyroidism
- Gout, a metabolic disease in which uric acid crystals are deposited in the body
- Rheumatoid arthritis (“rheumatoid arthritis”)
- menopause (due to estrogen deficiency) in women
- The male gender is also a risk factor. At least pre-menopausal women are protected to a degree from arteriosclerosis by the female sex hormones, especially estrogen.
- Genetic predisposition
Atherosclerosis: examinations and diagnosis
As part of a medical examination, the doctor will ask you about your habits. So he can create an individual risk profile. In particular, the questions are whether you smoke, move regularly and sufficiently, how they feed themselves or if you have pre-existing conditions that favor arteriosclerosis.
Through a blood test, the doctor can determine whether elevated cholesterol and blood glucose levels are present. In addition, the doctor determines in case of suspected arteriosclerosis your blood pressure, your weight and possibly your waist circumference.
The doctor looks for signs of complications and conducts appropriate tests:
- The so-called auscultation, ie the listening with the stethoscope, can sometimes hear abnormal flow sounds above the heart, the aorta or the arteries in the neck.
- Vascular constrictions or extensions of the carotid artery can be detected with a Doppler sonography from the outside. The result can also be used to estimate the risk of stroke.
- If there is coronary heart disease (CHD), the physician performs a stress ECG. Deposits in the inner walls of the coronary arteries can be visualized by the doctor with intracoronary ultrasound (IVUS). He introduces a small ultrasound probe directly into the coronary vessel to be examined.
- If the physician suspects a peripheral arterial disease (PAOD), he measures the walking distance, which the patient can travel without a break.
- If kidney artery calcification is suspected, renal function is checked with blood and urine tests.
- Atherosclerosis is also the leading cause of impotence. Corresponding information from the patient as well as an ultrasound examination can provide information about whether there is a narrowing of the blood vessels of the penis.
The extent of vasoconstriction can also be detected with other imaging techniques. X-ray examinations or magnetic resonance imaging with contrast agents visualize the blood vessels.
Arteriosclerosis: treatment
Basically, you can treat arteriosclerosis with medication or with surgery. Which therapy is used on a case-by-case basis depends on the extent of vasoconstriction and the potential complications.
Lifestyle changes and drug treatment
Anyone who already has atherosclerosis or an increased risk of the disease can slow their development or progression by changing their lifestyle. In the early stages, the plaques in the vessels may even regress. Pay attention to a healthy diet and adequate exercise. For some patients, a cholesterol-lowering diet may be useful. Obesity should be reduced, abstain from smoking and avoid permanent, negative stress.
Specific diseases that increase the risk of arteriosclerosis must be treated. These include, for example, diabetes mellitus or chronic kidney failure.
Antihypertensive drugs (ACE inhibitors) and cholesterol-lowering drugs (CSE inhibitors / statins, cholesterol absorption inhibitors) can also reduce the risk of arteriosclerosis. Some drugs lower the unfavorable blood lipid levels, such as omega-3-acid ethyl ester, fibrates and nicotinic acid.
For the treatment of advanced arteriosclerosis, the same medicines are often used as for the treatment of some cardiovascular diseases. These contain active ingredients that inhibit blood clotting and thus prevent the formation of a blood clot (thrombus). Examples: acetylsalicylic acid or clopidogrel.
Surgical treatment
Life-threatening effects of arteriosclerosis, such as advanced coronary heart disease (coronary artery disease) or imminent occlusion of the leg arteries, must be treated surgically. The choice of therapy depends on the type and extent of calcification.
- balloon expansion: A small balloon catheter is advanced through the bloodstream to the narrowed site and inflated. As a result, the vessel expands and the blood can flow freely again. If a new vascular occlusion threatens, a small, self-unfolding wire mesh (stent) is inserted into the vessel by means of a catheter, in order to keep it open.
- bypass: The surgeon creates a “diversion” that carries the blood past the narrowed area. For this he uses either an endogenous vessel (usually a vein piece from the lower leg) or a vascular prosthesis made of plastic. The bypass begins at a free section of the artery and finally flows back into the vessel behind the narrowed area.
- Surgery of a narrowed carotid artery (carotid stenosis): A narrowed carotid artery usually involves surgery. Frequently, the narrowing is scraped out of the artery. To do this, the doctor makes a cut at the relevant site, exposing the artery, pinching it off and then opening it.
Arteriosclerosis: disease course and prognosis
The course and prognosis of arteriosclerosis depends on several factors:
- the site of critical plaques and vascular changes
- The extent of vasoconstriction (stenosis), and the length of which impede blood flow
- the health of the patient: people who have ever had a heart attack or stroke are at greater risk
- how well the risk factors are turned off (lifestyle changes, treatment of causing metabolic diseases)
The earlier you decide to change your lifestyle, the better the prospects. Because the arteriosclerosis can lead to serious sequelae – such as coronary heart disease. Two-thirds of patients with this disease die from sudden cardiac death or heart attack.