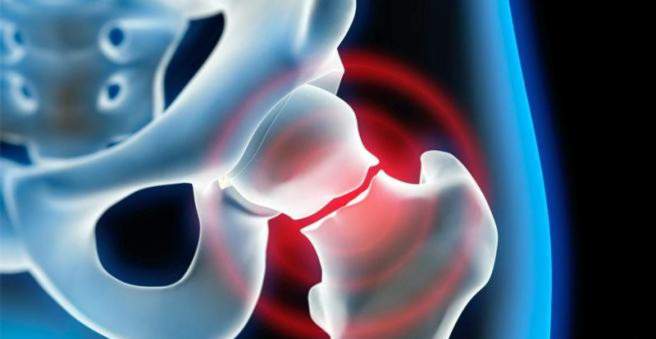
The femoral neck fracture (femoral neck fracture, femoral neck fracture) is common in older people with osteoporosis. Cause is usually a fall on the side of the hip or on the stretched or splayed leg. The hip fracture causes severe pain to those affected, and the leg can no longer be moved actively. The treatment of choice is usually surgery. Find out all about the femoral neck fracture here.
Femoral neck fracture: description
The femoral neck fracture is a common fracture in the elderly. Rarely, young people are affected in the context of a Hochrasanztraumas. Currently, about 100,000 people in Germany suffer a femoral neck fracture per year. Women are affected about four times more often than men. The lifetime risk of a fractured femur is about 11 to 23 percent in women and 5 to 11 percent in men, according to the Professional Association for Specialists in Orthopedics e.V.
Fractures: Classification according to Pauwels
The femur (femur) consists of four parts: a long shaft, the knee joint, a short, slightly angled neck and the head, which together with the pelvis forms the hip joint. In a femoral neck fracture exactly the part breaks between the head and shaft of the femur. Depending on the course of the fracture gap different fracture forms are distinguished (according to Pauwels). The Pauwels classification is based on how large the angle between the fracture surface and an imaginary horizontal line is and gives an indication of how stable the fracture is and which treatment option is appropriate:
- Pauwels Grade I: Fracture is <30 degrees to the horizontal plane. There are no shearing forces on the bone. This femoral fracture can be treated conservatively.
- Pauwels Grade II: The angle is 30 to 70 degrees. This form of fracture requires surgical treatment.
- Pauwels Grade III: The angle is greater than 70 degrees and must always be treated surgically.
femoral head necrosis
The femoral head is supplied to the front and back by blood vessels radiating into the joint capsule. If these capsule vessels are ruptured in a femoral neck fracture, there is a risk of femoral head necrosis (femoral head necrosis). The bony femoral head dies as a result of the reduced blood flow. The femoral head necrosis is one of the aseptic, so not infection-related bone necrosis.
Thighbone fracture: symptoms
If the hip is broken, severe compression and rotation pain in the groin and hip joint are the typical symptoms. This pain increases when the hip joint is moved passively (for example, by the doctor). The leg can not be moved actively. You may see local bruising and a bounce mark.
If the femoral neck fracture is postponed, the leg appears shortened in the lying patient and is rotated outward. Sometimes the thigh is additionally swollen in the area of the femoral head.
In rare cases, the complaints may be very mild in the crushed, solid femoral neck fracture, so that the person is only after several days because of increasing pain under pressure to the doctor.
Femoral neck fracture: causes and risk factors
Due to the increase in the frequency of osteoporosis (bone loss) in old age, the risk of a femoral neck fracture increases with the years of life. With osteoporosis, due to the reduced bone density, only a small amount of force is sufficient to break a bone. Already trivial falls in the house or over a curb can then lead to a fractured femoral neck.
Part of the falls in the elderly is caused by dizzy spells or a brief unconsciousness due to cardiovascular or nervous disorders. Also, drugs that limit the coordination and perception, alcohol and vision problems come as an accident cause in question.
Due to an existing tumor disease with secondary tumors (metastases) in the bone, a femoral neck fracture rarely occurs.
In children, adolescents and adults before the age of 60, a femoral neck fracture is very rare. They require strong bone action to cause the fracture, such as an accident involving a car or bicycle, a skiing accident or a fall from a high altitude.
Femoral neck fracture: examinations and diagnosis
A femoral neck fracture can be life threatening. Therefore, if you suspect a femoral neck fracture, you should immediately call the primary care service or your family doctor. The specialist for fractures of all kinds is the doctor for orthopedics and trauma surgery. He will ask you or any of your family members about the diagnosis and your medical history. Possible questions could be:
- How did the accident happen?
- Can you remember the exact time of the accident?
- Was there a direct or indirect trauma?
- Where is the possible fracture?
- How do you describe the pain?
- Are there pre-existing conditions such as osteoporosis, cardiac arrhythmias, diabetes and ametropia?
- Have you previously had symptoms such as stress-related pain?
In most cases, the characteristic symptoms following a fall already indicate a fractured femoral neck. For a more detailed explanation, the doctor will examine you carefully. In doing so, he will also pay attention to injuries to the vascular and nervous system by checking your motor skills, sensitivity and blood circulation. In addition, he will look for typical accompanying injuries of the skin and soft tissues.
Imaging diagnostics
The diagnosis of femoral neck fracture is secured by radiographs of the hip in two planes. The X-ray image also shows exactly where the break is. This plays an important role in further therapy. To accurately plan the operation, computer tomography (CT) is often used.
In case of advanced osteoporosis – despite clear discomfort – no fracture can be detected in the radiograph, further investigations are necessary. This includes a control X-ray examination three to five days after the accident and possibly a computed tomography (CT) or a magnetic resonance imaging (MRI). In case of doubt on the diagnosis of femoral neck fracture, MRI examination is the procedure of choice.
Thigh neck fracture – Differential diagnoses
Other fractures on the femur or hip cause similar symptoms as the femoral neck fracture. These include, for example, the pertrochanteric femoral fracture, the anterior pelvic fracture and the hip-joint fracture (pipkin fracture). The different fractures can be demarcated with the help of X-ray diagnostics.
Thighbone fracture: treatment
A femoral neck fracture is usually operated on. Only unstable, stable (“crushed”) fractures can sometimes be treated conservatively.
Elderly patients are often less mobile after treating a femoral neck fracture – often for fear of further fractures – and therefore rely on everyday help. The treatment goal is therefore that patients can use their leg as soon as possible. This is also important because with prolonged lying the muscle mass is rapidly degraded and complications such as pneumonia may occur.
Thighbone fracture: Conservative treatment
A femoral neck fracture close to the femoral head, not displaced, is called stable femoral neck fracture. If the patient suffers from only minor pain, he does not necessarily have to undergo surgery, but can be treated conservatively. The injured leg is splinted and patients receive painkillers and a physiotherapy exercise. However, conservative treatment is unfortunately an exception, as the fracture is postponed in most cases.
Conservative treatment may also be appropriate if, for some reason, a patient is not allowed to undergo surgery (such as in a risky general condition).
Thighbone fracture: OP
In femoral neck fracture, different surgical methods are available, depending on where the fracture line runs. Basically, a distinction hüftkopferhaltende and hüftkopferetzende procedures. Which method is better in an individual case depends, among other things, on the age and condition of the patient, the fracture shape and the ability to regenerate the bone tissue. Studies have shown that in patients over the age of 65, joint replacement often appears to be the better method.
Surgery should be performed as quickly as possible in the event of a femoral neck fracture: surgery within six to 24 hours after the trauma halves the risk of femoral head necrosis.
Femoral neck fracture: Hip-cup holding surgery
The hip-headed surgery is more likely to be used in younger and active patients. The fragments are then restored in the correct anatomical position and joined together with screws, plates and / or other implants. This procedure is called osteosynthesis. However, there must be sufficient blood flow for the bone to heal well.
In some cases, special screws such as the dynamic hip screw (DHS) or the cannulated screw osteosynthesis are used. If the femoral neck fracture has only been screwed or flattened, the leg must be consistently relieved for twelve weeks. In the other methods as well as in the dynamic hip screw, the patient is mobile faster.
Femoral neck fracture: Hüftkopfersetzende OP
In older patients, the femoral head is often supplied with little or no circulation. Then a joint replacement (endoprosthesis) is necessary: either the femoral head (condyle) alone or the acetabulum (acetabulum) is replaced by an artificial prosthesis. In the latter case one speaks of a total endoprosthesis (TEP, “artificial hip joint”). The advantage of this method is that the artificial joint can be loaded immediately and the patient is usually quickly mobilized after the procedure. Already in the first days after the operation, the patient can start with physiotherapy exercises. A TEP is also used in patients with femoral neck fracture who additionally have joint wear in the hip joint.
Thighbone Neck Surgery: Complications
Complications such as wound healing disorders, rebleeding, vascular or nerve injuries are relatively rare in a femoral neck fracture. If the hip joint is replaced, one expects during the operation with more or less large blood losses. There is a risk of blood clots (thromboses) forming after the procedure.
A dreaded surgical complication of a femoral neck fracture is infection. They can be tedious but are rare.
Also rarely happens that the prosthesis stem breaks out of the femur. He then has to be replaced and fixed in another operation. This significantly delays the healing process.
In rare cases, a graft or plaque surgery will worsen blood flow to the femoral head. He can die off (Hüftkopfnekrose) and must then be replaced by a prosthesis. The risk of this complication associated with a femoral neck fracture increases with age, so often from the outset, an artificial joint is used.
Further treatment
Before, during, and some time after the femoral neck fracture surgery, patients receive thrombosis injections into the subcutaneous fat tissue to prevent blood clots (thrombosis). Wearing support stockings and physiotherapy can also prevent clots.
Once the treatment of the femoral neck fracture has been completed, intensive physiotherapy should be started, which primarily trains the thigh muscles. The goal is that the patients can go back and climb stairs as quickly as possible.
Younger patients should partially load their leg for six weeks, while older patients are advised to fully load the leg, always in pain. Pain-adapted means that the pain is always good to endure.
Regular X-ray checks are important to check the fracture gap for position and firmness.
Thighbone fracture: disease course and prognosis
If a femoral neck fracture is operated soon, a very good result is usually achievable. In individual cases, the prognosis can be estimated from the extent to which the femoral head has shifted and thus affects the blood supply. This Garden classification looks like this:
- Garden I: A collapsed abduction fracture usually has a good prognosis and a low necrosis rate.
- Garden II: This is an axially compressed fracture that has not moved. The risk of necrosis is low.
- Garden III: The adduction fracture is postponed without the posterior cortical bone being displaced. The necrosis rate is high.
- Garden IV: The fragments are completely displaced and the vascular supply is interrupted. There is a high Hüftkopfnekroserate.
The steeper a break passes, the more the shear forces increase under axial load, whereby the fragments are moved. This also increases the risk of Hüftkopfnekrose and pseudoarthrosis (not growing together break).
Thigh neck fracture – healing time
The duration of healing in femoral neck fracture is individually different. It depends on several factors, such as how old and active the patient is.
In patients under the age of 65 years, with adequate treatment, up to 90 percent of bones heal fully. In the long-term course, however, it comes with nearly 20 percent to a Hüftkopfnekrose, which then a reoperation with joint replacement is necessary.
According to the German Society for Traumatology, patients with the hip-cup-holding procedure have an average of 11.7 days in the hospital, while a joint replacement is expected to have a mean length of stay of 12.4 days. During osteosynthesis, the implant is removed at the earliest after 12 months.
Thighbone fracture: prevention
There are simple ways to prevent a femoral neck fracture. If you suffer from other underlying conditions such as arrhythmia, diabetes and ametropia, it is important to have them treated. They increase the risk of falling and thus also the risk of a femoral neck fracture.
Sleeping aids are also dangerous for old people because they reduce the ability to react and thus also increase the risk of falls (for example when going to the toilet at night).
Hip protectors are only useful in patients who often fall, for example, in the nursing home. These are specially developed underwear, in the side of the hip pockets are incorporated. These bags contain plate-like, soft or hard protective elements made of various materials that can prevent a hip fracture when falling.
A calcium-rich diet and regular physical activity make the bones more stable so they do not break easily. You may supplement your diet with calcium and vitamin D-containing supplements – your doctor will advise you in this regard. Measures such as age-appropriate home furnishings with grab handles, walking aids and the weather adapted footwear can also one Femoral neck fracture prevent.