The gastric banding is an operative method that suppresses the natural feeling of hunger in overweight people. During surgery, a silicone band is wrapped around the upper part of the stomach. This artificially creates a very small stomach pocket. If it fills with food, the stomach signals satiety. Because of a rather high complication rate, the method loses importance. Read all about the use, effects and risks of gastric banding.
What is a gastric band?
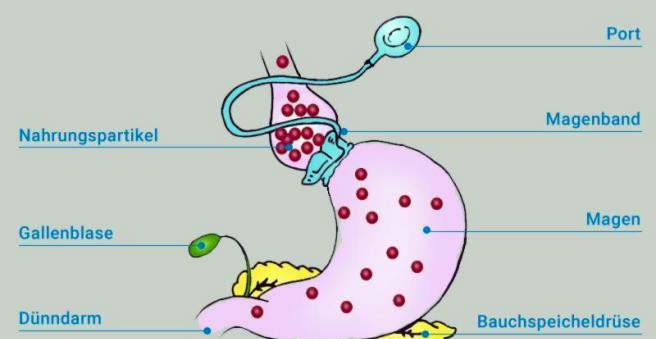
The so-called gastric band is a silicone tube, which is wound over an operation around the upper part of the stomach. He artificially divides the stomach into a small “forestomach” (pouch) and the large remaining stomach. The forestomach has a volume of only about 20 to 30 milliliters. That’s about the size of a table tennis ball. If the forestomach is stretched by food intake, this gives the brain the signal of saturation. The gastric band is therefore an aid that helps to lose weight, above all, by suppressing the feeling of hunger.
The gastric band is hollow inside and connected via a small tube with a so-called port system. The port is a small chamber, which is implanted under the skin during gastric band surgery. With a special needle, liquid can be filled into the port chamber and thus into the gastric band. This allows you to regulate the degree of gastric constriction as needed: the more fluid is injected into the gastric band, the more it strangles the stomach. If fluid is withdrawn, the inner diameter of the gastric band increases again and the stomach has more space.
Course of Gastric Band Op
A gastric band surgery takes about 30 to 60 minutes and is performed under general anesthesia. The hospital stay usually extends from one day before surgery to three to five days after surgery. As a rule, the procedure is performed as a so-called keyhole surgery (laparoscopy). In the keyhole technique, a total of five approximately two centimeters large skin incisions are set, over which the camera and the instruments are introduced. For implantation of the port, a slightly larger skin incision is also necessary at the lower edge of the sternum.
The silicone band is introduced via one of the working channels. With the instruments, the surgeon positions the band around the upper part of the stomach (cardia) and pulls it together like a cable tie. To be able to better estimate the size of the forestomach, a stomach tube with a small, deployable balloon is introduced into the forestomach next through the mouth. In the unfolded state, this is about as big as a table tennis ball (volume approx. 20-30 ml) and corresponds approximately to the final volume of the forestomach.
The gastric band can be adjusted after inserting the gastric balloon a bit up or down or even tightened a little firmer. Once the perfect position for the gastric band is achieved, it is still fixed to the surrounding tissue by several sutures.
Finally, the tube and the port chamber emerging from the gastric band are guided outwards through a cut in the region of the abdominal wall and are placed underneath the skin at the lower end of the sternum and sewn up. Through the port at any time a regulation of the gastric band diameter by liquid extraction or addition is possible.
About one month after the gastric band surgery, the port is pierced for the first time to deliver a few milliliters of fluid. As a liquid (a maximum of 9 milliliters) usually a so-called X-ray contrast agent is used, which is visible in the X-ray image. Thus, for example, a leak in the gastric band can be identified in the X-ray image. The ability to work is usually given two to three weeks after the operation, depending on the profession.
For whom a gastric band is suitable
The gastric band is suitable for people with a body mass index (BMI) of ≥ 40 kg / m² (grade III obesity). If a person suffers from other metabolic diseases such as diabetes (diabetes mellitus), hypertension or sleep apnea because of his or her excess weight, gastric banding may be useful from a BMI of 35 kg / m².
In any case, it is a prerequisite that all conservative (non-operative) measures have not produced sufficient success over six to twelve months. These measures include, for example, nutritional counseling, exercise training and behavioral therapy (Multimodal Concept, MMK). For gastric band surgery should be at least 18 and no more than 65 years old, the intervention in individual cases can also be done in younger or older people.
For whom a gastric band is not suitable
Certain physical and mental illnesses speak against an obesity operation such as the gastric band: in particular previous operations or malformations of the stomach, gastric ulcers and addictions or untreated eating disorders (for example, “binge eating” or bulimia) are important contraindications for a gastric band. Even pregnant women and people who take long-term anticoagulant drugs, must do without a gastric band.
Efficacy of gastric band surgery
Compared to the other surgical procedures, gastric banding achieves on average the lowest weight loss. Only a few patients reach their normal weight with the gastric band (BMI ≤ 25 kg / m²). Inadequate weight loss is especially to be expected when the patient ingests calorie and fat rich, soft foods or liquids that can easily pass through the tightness of the gastric band.
Studies indicate that with the gastric band, a loss of about 50 percent of the overweight can be achieved in the long term. Often this information is misunderstood: this does not mean that the method will lose 50 percent of the original weight. For example, if a patient has a BMI of 45 kg / m² prior to gastric band surgery, this is 20 kg / m² over normal weight (maximum 25 kg / m²). If the patient creates a reduction of his BMI by 10 kg / m² to 35 kg / m² through the gastric band, this corresponds to a weight loss of 50 percent of the excess weight.
Benefits of gastric banding over other procedures
Gastric band surgery is a bit of a complicated procedure and, with the correct surgical technique, poses a minimal risk to the patient. The comparatively low surgical risk is therefore not to be underestimated, especially since overweight people already have a significantly increased surgical risk anyway. Another great advantage of the gastric band is that it can be removed at any time and relatively easily and thus the procedure is completely reversible.
Risks and complications
Basically, the usual surgical risks exist when inserting a gastric band. These include bleeding, organ injuries, infections, wound healing disorders and problems due to anesthesia. Finally, there is also the danger that the stomach will be injured during the operation.
However, recent study results of recent years suggest that the complication rate of gastric banding is relatively high. Not the relatively low-risk operation itself is therefore the problem, but the complications that can occur after months or years. The most common specific complications of gastric banding include:
- Gastric band shift (“bandslippage”, in about 5.5 percent of all cases)
- Volume increase of the forestomach due to gradual dilation of the forestomach (“pouch dilatation”, in about 5.5 percent of cases)
- Gastric band leak or leak in connecting tube to port with leakage (in about 3.6 percent of cases)
- Elongation of the esophagus before the gastric band (“esophageal dilatation”, in about 3 percent of cases).
In very rare cases, more serious complications may occur, such as perforation of the gastric band through the stomach wall into the stomach (gastric perforation) or infection of the port chamber with pathogens. In some studies, the risk of reoperation (revision surgery) after gastric band surgery is estimated to be around 30 to 50 percent. This is problematic insofar as adhesions (adhesions) and scarring can occur due to every abdominal surgical intervention, which severely complicate follow-up operations and can also cause massive complications up to intestinal obstruction.
Diet with the gastric band
After the operation, the first postoperative day starts with food alone with liquids. These are taken only slowly and swallowed throughout the day. For the next four weeks, the hospital will provide you with a nutritional plan that describes the exact structure of the food. For about two weeks, it will only stay with liquid food. For the next two weeks, only soft food is on the menu. About four weeks after the operation, you finally start with normal diet. But there are some things to keep in mind:
- Gastric bandents should not only eat less, they also have to eat differently than before. In order for the porridge to pass the bottleneck, every bite must be chewed very thoroughly. Long fiber (beef, pork) or vegetables often cause problems.
- Since liquids also fill the small forestomach, at least for a short time, you should separate your food and drink.
- Sweets, especially sweet drinks, but also alcohol, high-calorie soups and porridge should avoid stomach tape carrier. They pass unhindered through the constriction between the front and the rest of the stomach, making them thick and thus nullifying the weight loss effect.
Gastric band: cost
The gastric band costs are made up of different parts: On the one hand, of course, the operation itself. In addition, there are other costs for inpatient hospitalization and the control appointments to check the gastric band. The gastric band costs vary considerably depending on the doctor and the treatment costs. The price range is approximately between 5000 to 10,000 euros.
Gastric band: Health insurance often takes over the costs
A gastric banding (gastric banding) is not a regular benefit of the statutory health insurance, but the intervention is usually accepted by the statutory and private health insurance on request. However, the criteria already mentioned above must be fulfilled. The application itself must also be prepared very carefully in order to assess the chances of reimbursing the costs gastric Banding to increase.