In a pulmonary embolism (pulmonary artery embolism) is a blood vessel of the lungs clogged, usually by a blood clot. The lung is then less perfused. So only insufficient oxygen gets into the blood. Signs of pulmonary embolism include sudden breathlessness and chest pain. The cycle can collapse. In the worst case, the patient dies. Read all about the symptoms, causes and treatment of pulmonary embolism.
Pulmonary embolism: short overview
- symptoms: Shortness of breath, chest pain, anxiety and restlessness, (cough) coughing, dizziness or fainting
- Treatment: Stabilize respiration and circulation, administer oxygen and pain / blood thinning agents (dissolution of thrombus), if necessary, catheter therapy, rarely surgery
- Prevent: Exercise, quit smoking, compression stockings, etc.
- Risk factors: u. a. Smoking, baby pill, heart and lung disease, older age, prolonged confined sitting, obesity, surgery, bed-rest
- Examination: Blood test, ECG, ultrasound, computed tomography (CT), scintigraphy
- Forecast: high risk of death in the first two hours after symptom onset; improved prognosis with rapid treatment
Pulmonary embolism: symptoms
The type and severity of pulmonary embolism symptoms depend on the size of the diseased lung area. Very small pulmonary embolisms sometimes cause no discomfort. Mostly it comes to a right sudden onset of respiratory distressby chest pain is accompanied. A pronounced pulmonary embolism can even lead to a circulatory collapse and in the worst case to death.
Classic symptoms of pulmonary embolism
Depending on the size of the clogged blood vessel of the lung, the following pulmonary embolism signs appear:
- Shortness of breath and / or accelerated breathing
- Cardiac arrhythmias (tachycardia, heart stuttering)
- Chest pain (may radiate to the abdomen or shoulder)
- Fear and restlessness
- Coughing and / or coughing up blood
- Rattle sounds when breathing
- sweats
- Dizziness or fainting
If very large vessels are affected by the embolism or a large area of the lung is no longer supplied with blood, it comes very quickly Circulatory collapse in the form of a shock, At the same time the blood pressure is very low. The heart still tries to pump enough blood into all the organs of the body and therefore beats faster. Hands, arms, feet and legs are coolbecause they are the least perfused. Sometimes they turn sour Lips bluishbecause they get too little oxygen. Often the sufferers, if they are still conscious, are very restless and / or have great fear.
If a large lung area is affected, it is also called a fulminant pulmonary embolism.
Harbinger of a pulmonary embolism
Before a blood clot clogs a pulmonary artery, small parts may detach from it and migrate into smaller pulmonary vessels. These small emboli may already have symptoms like chest pain, one whistling breathing, to cough or powerlessness cause. If treatment is given quickly, it is often possible to prevent a larger and more dangerous pulmonary embolism.
The complaints should therefore be taken seriously. This is especially true in respiratory distress and chest pain, if one at the same time Vein thrombosis is present. Parts of the blood clot in deep leg veins can be carried away by the blood and washed into the lungs. Then a pulmonary embolism threatens. In leg vein thrombosis, the affected leg is often painfully swollen, reddish and warmer than the other leg. If the patient was previously not mobile as usual and perhaps even bedridden, a reddened leg is already a thrombosis alarm. Since patients are typically inactive after surgery, the risk of pulmonary embolism is particularly high here. Because without movement, the veins have harder to keep the blood flow in motion. Then blood clots form easily.
Inactivity and / or immobilization of a limb slows down blood flow. As a result, the risk increases that a blood clot is created and a pulmonary embolism triggers!
Complications of pulmonary embolism
The bigger the blood vessel that is blocked, the heavier the consequences. They can even become life-threatening for the patient. The following table lists possible pulmonary embolism episodes and their main symptoms.
|
Complication of pulmonary embolism |
symptoms |
|
Pleural inflammation |
breath-dependent chest pain |
|
Entry of tissue water between the two pulmonary leaves (pleural effusion) |
Shortness of breath, noises during breathing |
|
pulmonary infarction |
coughing up blood |
|
Pneumonia caused by a pulmonary infarction (infarct pneumonia) |
Cough, shortness of breath, fever, chills |
|
Right heart failure and right heart failure |
jammed (thickened) jugular veins, water retention in the legs |
|
Hypertension in the pulmonary circulation (pulmonary hypertension) |
decreasing efficiency, shortness of breath in light conditions, dizziness |
Some of the problems can occur quite soon after an embolism. Others develop only after days or weeks.
Pulmonary embolism: treatment
If you suspect a pulmonary embolism you should call the emergency doctor immediately! The patient should move as little as possible. Otherwise, further clots may detach and block a vessel. In cardiovascular arrest you have to start immediately with the revival!
If necessary, the emergency physician will continue the resuscitation and, if necessary, give the patient artificial respiration. The respiration and circulation of the patient must be stabilized as quickly as possible in order to prevent organ damage (such as in the brain). The doctor can administer oxygen and medication to the patient, including blood thinners and analgesics. The hospital will then carry out necessary examinations and initiate further measures of pulmonary embolism therapy. They depend on the severity of the disease. Patients with severe pulmonary embolism must be monitored and treated in the intensive care unit.
Anticoagulant
In a pulmonary embolism are generally Anticoagulant drugs (Called anticoagulants). These ensure that no new blood clots form and do not enlarge existing clots. Small blood clots are broken down by the body.
Often the patient is first given a coagulation inhibitor for several days as a syringe or infusion, for example heparin. Thereafter, patients begin taking a anticoagulant in tablet form.
There are now also two anticoagulant agents that can be given as a tablet right after the diagnosis – ie without previously anticoagulant syringes or infusions must be administered.
The use of an anticoagulant in tablet form (“oral anticoagulation”) must be continued for several months.
In case of mild pulmonary embolism, coagulation inhibitors are often sufficient as the sole therapy. In addition, if the risk of complications is low, sometimes patients can even be treated on an outpatient basis (at home).
Medicines that dissolve the blood clot
In a severe pulmonary embolism, the anticoagulant therapy is not enough. The blood clot in the lungs must be specifically removed to restore blood flow to the lung tissue. This can be achieved with certain drugs, the so-called thrombolytics (also called fibrinolytics) such as streptokinase and urokinase. They are administered directly into the bloodstream of the patient and can rapidly expel the clot in the lungs. This form of pulmonary embolism therapy is called drug thrombolysis or lysis therapy.
Lysis therapy is very effective in pulmonary embolism, but it can have serious side effects: in some patients, it causes dangerous bleeding in the body, such as in the brain. Therefore, before using this form of pulmonary embolism treatment, the physician will weigh the benefits and risks for each patient. Most commonly, the method is used in people with severe pulmonary embolism and unstable blood flow. These “hemodynamically unstable” patients have a high risk of (fatal) complications. Therefore, it is particularly important to quickly eliminate the clot in the lungs.
Remove blood clots using a catheter
In some patients, drug-based thrombolysis would be too risky, perhaps because the risk of bleeding is too high. Then the blood clot in the pulmonary vein can instead be removed using a catheter. The catheter is gently inserted through a vein into the affected vessel and advanced to the blood clot. Using tiny instruments, the blood clot can then be minced into very small pieces. Some catheters also generate ultrasonic waves to clear the clot. At the same time, a thrombolytic agent can be administered via the catheter, which dissolves the clot.

Remove blood clots in an open operation
If catheter pulmonary embolism treatment is unsuccessful, it may be necessary to remove the clot in open surgery. The procedure will be pulmonary embolectomy called. The patient receives a general anesthetic and is connected to a heart-lung machine. This takes over the tasks of the two organs for the duration of the operation.
Since the entire operation is very risky, it is only performed in the most extreme emergency.
Pulmonary embolism: causes and risk factors
A pulmonary embolism is caused by the fact that a blood-supplying vessel of the lung clogged. This constipation can have several reasons.
Pulmonary embolism due to blood clots
In most cases, the pulmonary embolism is the result of a blood clot that has developed in a leg vein (leg vein thrombosis) and was flushed with the bloodstream into the lungs. The reason why the clot breaks off in the leg can be quite banal, for example getting up in the morning, but also pressing in the bowels and sudden physical exertion.
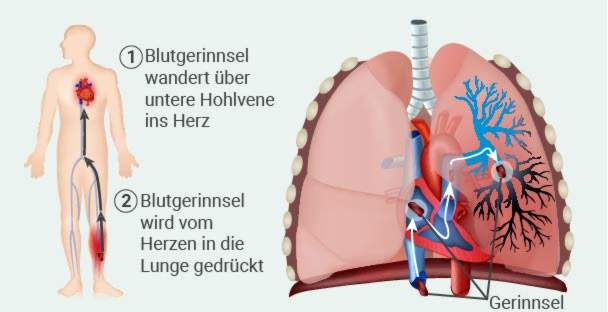
The detached clot gets to the right heart with the venous blood and is pumped from there into the lungs. As the pulmonary arteries continue to ramify and become narrower, the clot eventually gets stuck and blocks the vessel.
Certain risk factors promote the development of leg vein thrombosis. These include:
- Smoke
- Taking the anti-baby pill or hormone replacement therapies
- Pregnancy and childbed
- Limitation of movement (bed rest, plaster casts)
- Cancers or treatments
- Operations (especially on the abdomen, hip or knee)
- overweight
- longer air travel
- Heart and lung diseases
- Coagulation disorders of the blood
- higher age (from 50 to 60 years)
- Thrombosis in family members
- Chronic venous insufficiency, varicose veins
Other causes of pulmonary embolism
More rarely, the obstruction of a pulmonary artery in pulmonary embolism has other reasons than a blood clot:
Sometimes it is fat embolism behind it. This dissolves fat from the bone marrow, which migrates via the venous vessels into the lungs and clogs a vessel. This can happen, for example, after orthopedic surgery such as the implantation of a hip prosthesis or after a fracture of the femur.
The Amniotic fluid embolism is a very dangerous complication for the mother and child at birth. Through the wound caused by the partially dissolved placenta in the uterus, amniotic fluid can penetrate the maternal bloodstream and enter the lungs. Through various chemical processes and a form of allergic shock thromboses are formed in the blood vessels. The arteries of the lungs narrow. The numerous blood clots trigger further embolisms. Ultimately, the cardiovascular system can collapse.
The Pulmonary embolism due to gas (Air embolism) occurs when air passes into the body veins and is transported with the blood into the pulmonary arteries. Very rarely can this happen via venous access or through medical intervention.
Pulmonary embolism: examinations and diagnosis
Symptoms such as sudden chest pain and respiratory distress may indicate pulmonary embolism but may have other causes as well. For clarification, the doctor will first ask the patient some questions to raise the medical history (anamnese). This helps to estimate the likelihood of pulmonary embolism. Possible questions of the doctor are:
- Are the lower legs swollen or red?
- Have you undergone surgery in the past four weeks?
- Were you bedridden or mobile for a long time?
- Do you suffer from a tumor disease?
- Have you received any tumor therapy in the last six weeks (radiation, chemotherapy, etc.)?
- Have you ever had deep vein thrombosis or pulmonary embolism?
- Do you cough up blood?
- Is there a pregnancy?
- Are you taking the baby pill or any other female sex hormone supplement?
Following the anamnesis interview follows an exact physical examinationto find further evidence of pulmonary embolism. The doctor, for example, listens to the heart and lungs and measures the patient’s blood pressure.
Pulmonary embolism: blood tests
Certain blood levels may be groundbreaking for a pulmonary embolism diagnosis. Because with a leg vein thrombosis or a pulmonary embolism the body tries to dissolve the blood clots again. This creates so-called D-dimers, These are fission products of the fiber whiteness fibrin, which is involved in building up a blood clot. If no D-dimers are detectable in the patient’s blood, pulmonary embolism is highly unlikely.
Other important blood counts are troponin and Brain Natriuretic Peptides (BNP), In a pulmonary embolism, their blood levels are increased.
Also oxygen and carbon dioxide in the blood are important parameters in case of suspected pulmonary embolism. Since the gas exchange in the lung is impaired in a pulmonary embolism, the oxygen content in the blood decreases. Breathing accelerates to compensate for this deficiency. As a result, more carbon dioxide is exhaled – its content in the blood also decreases.
Pulmonary embolism: ECG
Electrocardiographic examination may also support pulmonary embolism diagnosis. For this purpose, several electrodes are attached to the chest, wrists and ankles of the patient and connected with cables to a meter. A recorder records the heartbeat. Since in a pulmonary artery embolism the heart has to pump against a stronger pressure and is supplied with less oxygen, the ECG shows signs of an overload of the heart muscle.
Pulmonary embolism: ultrasound examination
An ultrasound examination of the heart (echocardiography) can show if cardiac function is impaired as a result of pulmonary embolism. For this purpose, a gel is applied to the chest in the area of the heart. The examiner can use the ultrasound probe to look at the heart cavities, valves and blood flow. In addition, the leg veins are often examined with the ultrasound machine: Very often a pulmonary embolism develops as a result of a vein thrombosis. Ultrasound can be used to expose possible residual clots in the veins.
Pulmonary embolism: CT and scintigraphy
through Computed tomography (CT) In most cases, a pulmonary embolism can be made very visible. Before the examination, the doctor injects the patient with a contrast medium into a vein. Subsequently, a CT image is taken of the patient’s chest. The radiologist can then follow the course of the pulmonary vessels and locate thrombi.
In some cases, too Scintigraphy of the lungs carried out. This is a nuclear medicine examination in which the patient must inhale a radioactively labeled substance. In the pictures of the examination, one can see how well the individual lung areas are perfused and ventilated.
Pulmonary embolism: disease course and prognosis
How dangerous a pulmonary embolism is depends on the extent and health of the patient. A pronounced pulmonary embolism is life threatening. Acute deaths often occur within two hours of symptoms of pulmonary embolism. The chance of survival of a patient can be increased if a doctor is immediately contacted and the correct treatment is initiated.
After surviving disease, the likelihood of re-pulmonary embolism is often increased. It is therefore important to reduce the risk of blood clots. This includes, for example, that patients conscientiously take the anticoagulant medication prescribed by the doctor. This drug prevention can last for months or years. Some patients also need to use the anticoagulants for life.
Further preventive measures can be found below.
Pulmonary embolism: prevention
In general, take care of everyday life regular exercise, This prevents the formation of blood clots and thus also a possible pulmonary embolism.
For longer bed rest and diseases that promote thrombosis, the doctor prescribed often Anticoagulant drugs (as a heparin syringe). They are designed to reduce the risk of thrombosis and pulmonary embolism.
Do not smoke! This is especially true if you have already experienced thrombosis.
After an operation You should move quickly if possible. If you need to lie in bed, you can accelerate the flow of blood in the veins by changing the tension of the muscles. This reduces the risk of blood clots forming.
Also on longer air travel you should stimulate the blood flow in the legs. Get up every now and then and walk a few steps. You can also sit down Fußgymnastik operate (for example, the feet circling). Drink enough, but not coffee or alcohol. Do not wear tight clothes. Especially with known venous insufficiency you should compression stockings wear during the flight. Even with longer bed rest and during pregnancy such stockings can be useful.
If there is a high risk of thrombosis and pulmonary embolism, a sort of sieve (Cava filter) are inserted into the inferior vena cava. It captures clots from the leg veins so they do not enter the lungs and cause pulmonary embolism.
Additional information
guidelines
- S2k guideline “Diagnosis and therapy of venous thrombosis and pulmonary embolism”, German Society for Angiology – Society for Vascular Medicine e.V. (as of 2015)