People with lactose intolerance do not tolerate many dairy products. Because they lack an enzyme that is needed for the utilization of lactose. The most common symptoms of lactose intolerance are flatulence, abdominal cramping and diarrhea. But lactose intolerance can also be felt outside the gastrointestinal tract. Read here, which triggers lactose intolerance, how to identify food intolerance and what to do about it.

Lactose intolerance: short overview
- Causes: Deficiency of the enzyme lactase, bacteria produce gases and acids in the colon
- symptoms: Abdominal pain, diarrhea, abdominal distension, intestinal wind, bloating, nausea, nonspecific symptoms such as headache
- Diagnosis: H2 breath test, diet / exposure test, symptoms alone provide insufficient evidence
- Treatment: Adaptation of diet, abandonment of dairy products, lactase tablets
- Forecast: no illness, not dangerous, but limits quality of life
Lactose intolerance: causes and triggers
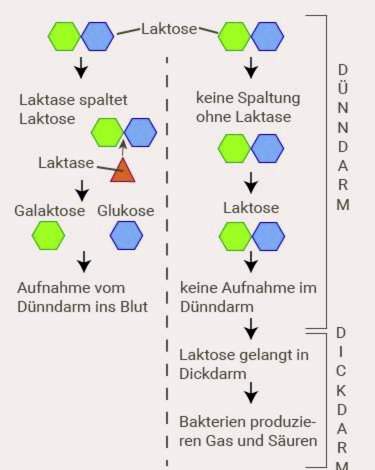
Milk products contain lactose, which is also referred to as lactose. Lactose itself can not be absorbed by the intestinal mucosa, but only the individual sugars that make it up. This means that the milk sugar must first be broken down with the help of an enzyme so that it can enter the blood via the intestinal mucosa. The enzyme is called lactase. It is normally produced by the mucus cells in the small intestine – but not or not enough in people with lactose intolerance.
The result: the lactose continues to migrate from the small intestine into the large intestine. There he serves bacteria as food. This waste products remain, which then trigger the typical symptoms. These waste materials include lactic acids, short-chain fatty acids and gases such as hydrogen, carbon dioxide and methane.
Although the cause of lactose intolerance is ultimately a deficiency of the enzyme lactase, this deficiency can come in several ways. Accordingly, the symptoms are different and can occur at different ages for the first time.
Primary lactose intolerance is very common
Actually, lactose intolerance is not a disease. Across the world, adults who can digest lactose are even the exception. It’s different with babies. Newborns can normally metabolize lactose without any problems. Breast milk also contains lactose, even more than cow’s milk. But already after the first months of life, the amount of the enzyme gradually decreases.
If it falls below a certain level, lactose intolerance symptoms appear. When this time is reached is different. Therefore, the age varies when so-called primary lactose intolerance begins. The victims are usually between five and twenty years old. In children under the age of five lactose intolerance rarely occurs. Most of the time, the first symptoms appear in adolescence. Primary lactose intolerance is by far the most common form of lactose intolerance.
Incidentally, the enzyme production does not completely set. Most sufferers still have a small amount of the enzyme. There are large individual fluctuations, which is why some people with lactose intolerance still tolerate a certain amount of lactose in the diet, others react to even the smallest amounts with complaints.
That about one third of humanity can digest lactose for life is due to a genetic mutation. Scientists assume that this change in DNA originated in Central Europe about 7500 years ago. Although the amount of lactase in these people also decreases, it remains large enough to continue to split lactose.
This condition could have been a survival advantage at that time. For with the beginning of livestock milk was present in large quantities and became an important source of food. Even today, every person who has no lactose intolerance is the carrier of this genetic change.
Acquired (secondary) lactose intolerance
Unlike primary lactose intolerance, secondary lactose intolerance is the result of another disease. The production of lactase is not natural, but throttled by damage to the intestinal mucosa. Triggers are sometimes major operations in the gastrointestinal tract, autoimmune diseases such as Crohn’s disease or severe courses of gastrointestinal influenza. Also, gluten intolerance (celiac disease) is often the cause of secondary lactose intolerance, because the intestinal mucosa becomes inflamed in this disease and thereby the production of the enzyme lactase is impaired.
Usually secondary lactose intolerance returns as soon as the mucosal cells have recovered in the intestine. In rare cases, however, it can become chronic. It always depends on the severity of the causative disorder.

Congenital lactose intolerance in the baby
Innate lactose intolerance is a very rare form of the disease. In her case, the body can either produce no lactase at all, or only in tiny amounts due to a genetic defect from the beginning of life. One therefore speaks of an absolute lactose intolerance. The affected babies already get persistent diarrhea through the breast milk after a few days. Breastfeeding is not possible. Under certain circumstances, the uncleaved lactose can even enter the bloodstream via the gastric and intestinal mucosa and cause severe poisoning there. As a therapy is only a lifelong waiver of lactose in question.
However, if newborns have milk sugar problems, it is not necessarily a congenital lactose intolerance. The digestive tract can generally be very sensitive during the first weeks of life. Sometimes the lactase production is not working properly, but usually this problem will soon go away.
Lactose intolerance due to bacterial colonization of the small intestine
In some journals it is discussed whether possibly a deficient colonization of the small intestine with bacteria can lead to a lactose intolerance. Normally, bacteria and other microorganisms are found mainly in the colon. This is completely normal and even very important for digestion. Under certain circumstances, however, it may lead to an increased colonization of the small intestine, which is problematic.
On the one hand the colonization of the small intestine mucosa – and thus the production of lactase – can be impaired. On the other hand the bacteria in the small intestine begin to decompose the lactose before it can be split by the lactase. Still, there is no clear research that confirms this assumption. However, some studies show that in some cases lactose intolerance disappears as soon as the small bowel malady is treated with antibiotics.
Lactose intolerance: symptoms
The following symptoms typically occur with lactose intolerance:
- bloating
- bloating
- intestinal winds
- loud bowel sounds
- stomach pain
- Nausea, rarely with vomiting
- diarrhea
Flatulence and abdominal pain are caused by the gases that bacteria produce in the colon when they break down the lactose. Other wastes that are formed, namely milk and fatty acids, are “water-tapping”. As a result, more fluid flows into the intestine and produces diarrhea.
The symptoms are often aggravated by the fact that sufferers are embarrassing the sometimes foul-smelling intestinal wind, which is why they understandably hold them back in public. If the air can not escape, the intestine continues to dilate and the abdominal pain increases.
Paradoxically, lactose intolerance can also cause constipation. And that is when predominantly methane is produced during lactose decomposition. This gas slows down the intestinal activity and thus causes constipation.
What influences the lactose intolerance symptoms?
The described lactose intolerance symptoms can be very different from human to human, or be perceived. Some have pronounced symptoms after each meal containing lactose, others feel little more than a slight malaise. The following factors influence the lactose intolerance symptoms:
Degree of lactase deficiency
There is a lack of the enzyme lactase behind a lactose intolerance. This lactase deficit is individually very different. In some cases, almost no enzyme is produced, while others still have a certain amount and usually do not feel any complaints with a smaller intake of lactose.
Lactose content of the meal
Of course, the lactose content plays a crucial role in a meal. The more milk sugar it contains, the more pronounced the symptoms of lactose intolerance. In addition, the further composition of the food has an influence. Depending on the other nutrients with which lactose is taken up, this can have different effects on processing in the intestine.
Composition of the intestinal flora
In each person live in the large intestine slightly different bacteria (= intestinal flora). The better these roommates can reduce the lactose, the more violent are the symptoms of lactose intolerance. Not only varies the amount of gases produced, but the microorganisms also form different gases. For example, if they produce predominantly carbon dioxide, the intestinal winds are less foul-smelling than they produce more methane.
Speed of food transportation
The path taken by food during digestion is the same for all people, but not the time they need it. Up to the stomach there are hardly any differences, but how quickly the porridge is transported through the intestine, is individually very different.
This in turn has an influence on the lactose intolerance symptoms. The longer the porridge stays in the small intestine, the more time lactose has to split the milk sugar. If he walks on quickly, more undigested lactose gets into the large intestine and leads there to the typical complaints. The duration of transport in the small intestine varies between about one and two and a half hours, but in some people is even outside this range. Accordingly, the time after which lactose intolerance symptoms occur in those affected varies.
Personal pain sensation
Every person perceives pain differently. Where some have gone to the doctor for a long time, others hardly notice anything. Even with lactose intolerance, the symptoms feel differently. Lactose intolerance pain is caused by excessive intestinal stretching. In patients with irritable bowel syndrome, for example, there is generally an increased sensitivity to pain in the gastrointestinal tract. If these people then additionally have a milk sugar intolerance, they perceive this all the more violent. On the other hand, it may also happen that someone has been shown to be unable to digest the milk sugar but still has little or no lactose intolerance symptoms.
Lactose intolerance symptoms outside the gastrointestinal tract
In addition to gastrointestinal discomfort, the following unexpected symptoms may occur with lactose intolerance:
- a headache
- dizziness
- memory problems
- listlessness
- body aches
- acne
- Depressed moods
- sleep disorders
- sweats
- Arrhythmia
Although not typical, these lactose intolerance symptoms may in some cases be in addition to gastrointestinal symptoms or even alone. In the latter case, food intolerance is difficult to detect.
How a milk sugar intolerance outside the gastrointestinal tract can cause discomfort is still under discussion. A possible explanation: The bacterial decomposition of lactose in the colon produces toxic metabolic products that enter the bloodstream. These could cause problems in different body structures (especially in the nervous tissue).
Lactose intolerance: test
Most commonly, the so-called hydrogen breath test or H2 breath test is used to diagnose lactose intolerance. It is based on the intestinal bacteria also produce hydrogen gas when decomposing the milk sugar. This can be detected in the exhaled air. Further diagnostic options are the lactose tolerance test, genetic test, small bowel biopsy or the diet / exposure test.
How the individual tests work in detail and which advantages and disadvantages they have, you can read here: Lactose intolerance test
Lactose intolerance: diagnosis
Lactose intolerance can not be clearly diagnosed on the basis of the typical symptoms. Because gastrointestinal complaints also occur in many other food intolerances and other diseases of the gastrointestinal tract. For example, a cow’s milk allergy can also cause the typical lactose intolerance symptoms – not always specific allergic symptoms are added.
In addition, every person sometimes has bloating and abdominal pain, so that these symptoms are often not associated with lactose intolerance for a long time and are not always immediately recognized by doctors as lactose intolerance symptoms.
Lactose intolerance: When do you need to see a doctor?
If you are experiencing persistent gastrointestinal symptoms in yourself or your child, you should always go to the doctor to find the cause. The right contact for suspected lactose intolerance is the family doctor or a specialist in internal medicine. Already by the description of your complaints (anamnesis) he receives important information. It may also make sense that you keep a journal in which you document your meals and any complaints that may occur. Possible questions of the doctor could be for example:
- Do you suffer from abdominal pain, flatulence and diarrhea after consuming dairy products?
- How long have the complaints already been?
- Are there cases of lactose intolerance in your family?
- Do you have other bowel disease (gastrointestinal flu, Crohn’s disease, etc.?)
- Do you take any medicine?
After the anamnesis interview, the physical examination follows. The doctor with the stethoscope listens to the bowel sounds and gently scans the belly. The physical examination is mainly used to rule out other causes of the symptoms. This usually requires further examinations such as blood count with determination of the inflammatory values or an ultrasound.
If there is a reasonable suspicion of lactose intolerance, the next step may be a transient low-lactose diet. If the symptoms improve, a lactose intolerance is very likely. Final safety only provide special lactose intolerance tests.
Lactose intolerance: treatment
Since lactose intolerance is not a disease, it can not be cured. By a lactose-poor / -free lifestyle, however, you can live mostly free of complaints. An artificial supply of the missing enzyme lactase via tablets is also possible if required.
Lactose intolerance: nutrition
The most important measure of lactose intolerance is one Adaptation of nutrition, This is not easy at first, because you have to do without many things, which of course previously belonged to the menu. Nevertheless, the most important rule for the lactose intolerance diet is to stay away from anything that contains more lactose. However, every person has a different tolerance limit in terms of the amount of lactose he can tolerate. To find out, just try it out. Some products also contain far less milk sugar than many believe.
“Lactose-free” refers to products that contain a maximum of 0.1 grams of lactose per 100 grams of food. These low levels are usually tolerated by people with lactose intolerance. Many sufferers get even with a content of 1 g lactose / 100 g food still no complaints.
Lactose intolerance: foods with low lactose content (≤ 1 g / 100 g)
The following foods have a lactose content of ≤ 1 g lactose per 100 g food. They are usually very well tolerated. With cheeses in general applies: The longer the cheese has ripened, the lower the lactose content. Hard cheese such as Parmesan or ripe Gouda are therefore usually well tolerated:
|
Food |
Grams of lactose per 100 g of the food |
|
Parmesan and other long matured cheeses |
about 0 – 0.05 |
|
Butter lard, butter pure fat |
about 0.1 |
|
Camembert |
about 0.1 – 1 |
|
butter |
about 0.5 – 1 |
|
Mozzarella, Brie |
about 0.5 |
|
Feta cheese |
about 0.5 – 1 |
|
bitter chocolate |
about 0.5 |
Lactose intolerance: foods with moderate lactose content (1 to 5 g / 100 g)
The following foods have a moderate content of 1 to 5 g of lactose per 100 g of food. While some people with lactose intolerance still tolerate these foods without any problems, they can already cause symptoms in others:
|
Food |
Grams of lactose per 100 g of the food |
|
Nut nougat cream |
about 1.5 – 3.0 |
|
mascarpone |
about 2.5 |
|
sour cream |
about 3 |
|
cream |
Approximately 3.3 |
|
plugs |
about 3 – 4 |
|
yogurt |
about 3 – 4.5 |
|
cottage cheese |
about 4 |
|
buttermilk |
about 4 – 5 |
Lactose intolerance: foods with high levels of lactose (> 5 g / 100 g)
In the following foods, the lactose content is often more than 5 g lactose per 100 g food. Due to their high lactose content, they can cause discomfort in people with lactose intolerance:
|
Food |
Grams of lactose per 100g of food |
|
milk |
about 5 |
|
cheese spread |
about 6 |
|
ice cream |
about 7 |
|
milk chocolate |
about 10 |
|
evaporated milk |
about 10 |
|
Skimmed milk powder |
approx. 50 |
|
whey powder |
about 70 |
Lactose intolerance: food with hidden lactose content
Many foods may contain lactose, although you would not expect it. Especially with finished products, you should read the ingredient list carefully.
- Margarine (often lactose-free)
- Baked goods of all kinds
- spreads
- Ready meals (such as instant soups, preserves, mashed potatoes powder)
- canned fish
- Canned vegetables, such as gherkins
- spice mixtures
- cereal mixtures
- Salad dressing, pesto, mayonnaise
- Meat and sausage products, including ham
Also many medicines contain lactose as a binder, but mostly in irrelevant quantities. However, read carefully the package leaflet with the ingredients before taking it and consult a doctor or pharmacist if necessary.

The food industry likes to use milk sugar as a bulking agent to give food a “fuller” taste in the mouth. This is why milk sugar is also found in bread, meat and many ready meals. But even here, the lactose quantities are usually negligible.
Especially at the beginning, the “world of lactose” still seems quite confusing, but with increasing experience, those affected usually know very well what can be eaten despite lactose intolerance and what is not. For professional advice on the right diet for lactose intolerance you can also go to trained dieticians.
Products for people with lactose intolerance
In recent years, the industry has increasingly launched products for people with lactose intolerance on the market. They no longer contain lactose and are specially labeled.
For those who do not like dairy products, lactose-free dairy products are a good choice, especially to prevent calcium deficiency. In some cases, however, the label “lactose-free” advertised, even if from the outset no lactose is included. This is worth a comparison of prices and the view of the contents of the food from other providers. Even if lactose-free foods seem a bit like a lifestyle product at the moment, people without lactose intolerance do not benefit from them and unnecessarily ease their wallet.
Complication: osteoporosis and calcium deficiency
Avoiding dairy products often does not provide the body with sufficient calcium – there is a risk of osteoporosis. This is why it is sometimes necessary to take calcium supplements. Discuss this with your attending physician. It also makes sense to include other calcium-rich foods other than dairy products, such as green leafy vegetables, coconut flakes or sesame, more often on the menu. In particular, in children can be due to the absence of dairy products, a calcium deficiency and thus a bone mineralization disorder. Basically, lactose intolerance is rarely the sole cause of osteoporosis.
Lactose intolerance: medicines
If you are in the mood for apple strudel with custard or chocolate ice cream despite lactose intolerance, you can prevent the symptoms by drinking Lactase tablets or take capsules just before or during the meal. The tablets provide the body with lactase, which it can no longer produce itself. The amount of enzyme per tablet is given in the unit FCC (“Food Chemical Codex”). For each five grams of milk sugar, 1000 FCC is recommended.
Estimating the lactose content of a meal is very difficult and requires a lot of experience. But you do not have to be afraid of an overdose with lactase – the enzyme does no harm. If in doubt, take too much rather than too little lactase. Since the preparations are usually relatively expensive and not paid by the health insurance, they are not suitable for the long-term therapy of lactose intolerance, but allow now and then a small “sin” when eating.
Who at the same time iron tablets must, however, be careful, since one interaction between the medications consists. The intake should therefore take place at least three hours delayed. Also note that a variety of non-standard preparations containing lactase are commercially available. Let your doctor or pharmacist recommend a suitable preparation.
Lactose intolerance: disease course and prognosis
Lactose intolerance is neither life-threatening nor does it limit life expectancy. You should only be aware of the symptoms that can occur with nutritional errors. Most sufferers are symptom free with a low-dairy diet. If the symptoms persist despite the right lactose intolerance diet, another cause, such as irritable bowel syndrome, may be behind it. To avoid this, you should get a doctor test for lactose intolerance.
Lactose intolerance: frequency
Anyone who suffers from lactose intolerance in Germany is the exception. Even though about 10 to 20 percent of Germans are now unable to digest lactose: the shelves in the supermarkets are full of dairy products and in the restaurant you hardly get a dessert that does not contain lactose.
On the other hand, lactose intolerance is in good company around the world. In textbooks, the number of people affected is estimated at about 70 percent globally. Overall, a strong north-south gradient is emerging. In Northern Europe and North America, the numbers are similar to those in Germany or even lower. Even in Russia, less than half of the population has lactose intolerance. A completely different picture emerges in South America, Africa and Asia.
There lactose intolerance is the norm. In China and Southeast Asia, the rate is almost 100 percent. Even in southern Europe, the majority is lactose intolerant. The reason for this geographically different distribution of lactose intolerance is genetically determined.
Additional information
book recommendations
- The Lactose Navigator: For lactose intolerance (Jan Niklas Stratbücker, 2015, LAXIBA)