In a polyneuropathy peripheral nerves are damaged. These can be, for example, nerves in the arms and legs or those that supply internal organs. The most common causes of this nerve damage include diabetes mellitus and alcohol abuse. Read more about symptoms, causes, diagnosis and treatment of polyneuropathy here.
Polyneuropathy: short overview
- What is polyneuropathy? A group of diseases in which several or many peripheral nerves are damaged. These are the nerves outside the central nervous system (brain and spinal cord). Polyneuropathy is also called “peripheral polyneuropathy” or “peripheral neuropathy” (PNP).
- symptoms: depending on which nerves are damaged. It often comes to nausea, tingling, pain and numbness in the legs and / or arms, muscle weakness, muscle spasms and paralysis, disorders of bladder emptying, constipation or diarrhea, impotence, etc.
- investigations: physical examination, electroneurography (ENG), electromyography (EMG), blood tests etc.
- Causes: especially diabetes (diabetes mellitus) and alcohol abuse. Other causes include other acquired diseases or poisoning. Rarely is a polyneuropathy genetically determined. Sometimes, no cause can be found.
- Therapy: If possible, the cause is eliminated or treated. In addition, the symptoms can be specifically treated (painkillers, TENS, antidepressants, anticonvulsants, physiotherapy, alternative baths, wraps, orthopedic aids, etc.)
Polyneuropathy: symptoms
In a polyneuropathy peripheral nerves are damaged. These can be, for example, nerves that command muscle contractions (motor nerves) or control digestion or respiration (autonomic nerves). Often nerves are also affected, which are responsible for the sensitive sensation of touch, temperature, pressure and vibration (sensitive nerves).
Which type of polyneuropathy symptoms occur in a patient thus depends on the damaged nerves. Accordingly, one distinguishes motor, autonomous and sensitive disorders.
You can also classify polyneuropathy symptoms according to their distribution on the body:
- Most polyneuropathy symptoms affect both feet or both arms. This is called symmetric polyneuropathy, On the other hand, if the nerve damage only occurs in one side of the body, there is one asymmetric polyneuropathy in front.
- If the nerve damage mainly affects areas of the body that are away from the trunk (such as feet, hands), it is one distal polyneuropathy). Much rarer, the disease extends to body parts close to the body (proximal polyneuropathy).
Polyneuropathy Symptoms: Sensitive Nerves
Nerves leading from the skin to the brain are called “sensitive”. They inform the brain, for example, about touch, pressure, temperature or pain stimulus or vibrations. When this sensibility is disturbed by a polyneuropathy, perception suffers, for example, in the arms and legs. The toes are often affected first. It happens, for example Abnormal sensations, tingling or stinging, burning pain.
numbness are also possible polyneuropathy symptoms. If these occur in the legs, sufferers have, for example Coordination problems while walking.
Is this Temperature sensation disturbed, it can be easier to get injuries. For example, polyneuropathy patients do not realize that their footbath is too hot. People with pronounced polyneuropathy can also To perceive pain only diminished, This also increases the risk of injury.
Most polyneuropathies are associated with sensitive disorders.
Polyneuropathy Symptoms: Motor Nerves
Motor nerves direct commands from the brain to the skeletal muscles. The commands cause a muscle to contract (contract). In motor polyneuropathy these nerves are damaged. As a result, the concerned Lose muscle strength, In the worst case occur muscle paralysis on. Also muscle cramps are possible.
In general, when tissue is insufficiently or not activated by the supplying nerves for a long time, it degenerates: it shrinks and shrinks. This happens very fast with the skeletal muscles. Thus, a motor polyneuropathy in severe cases too muscular dystrophy (Muscular atrophy).
Polyneuropathy Symptoms: Autonomic Nerves
Autonomic (vegetative) nerves control the function of internal organs such as the heart, lungs, stomach, intestines, genitalia and bladder. They are not subject to the will. For example, you can not consciously order the heart muscle to contract.
If autonomic nerves are damaged, it can lead to serious or even life-threatening symptoms. For example, if a polyneuropathy is damaged in the intestinal nerves diarrhea or constipation occur. Are nerves affected, which regulate the bladder function, urination, so the Bladder emptying disturbed, A nerve damage in the lungs can Apnea trigger. Autonomic polyneuropathy affects nerves on the myocardium, which can be dangerous Arrhythmia result.
Polyneuropathy symptoms at a glance
The following table shows important polyneuropathy symptoms at a glance:
|
Sensitive symptoms |
Motor symptoms |
Autonomic symptoms |
|
Tingling, running ants |
muscle twitching |
pupillary disorders |
|
sting |
muscle cramps |
Water retention (edema) |
|
Fuzziness and numbness |
muscle weakness |
ulceration |
|
Feeling of being tied up |
muscular dystrophy |
reduced sweating |
|
swelling feelings |
Tachycardia in peace |
|
|
Feeling of unpleasant pressure |
Stomach paralysis (gastroparesis) |
|
|
Feeling like cotton wool |
Diarrhea, constipation |
|
|
Gait insecurity (especially in the dark) |
disturbed bladder emptying |
|
|
lack of temperature sensation |
Impotence (erectile dysfunction) |
|
|
painless wounds |
Dizziness / fainting when getting up |
Diabetic polyneuropathy: symptoms
In polyneuropathy due to diabetes (diabetes mellitus), the symptoms develop creeping. First of all, the sensitive nerve fibers are usually damaged. The affected then notice, for example Numbness or tingling in the legs, Many also feel one burning pain in the feet ( “Burning Feet Syndrome”).
These polyneuropathy symptoms are on especially at rest or at nightnoticeable. Some patients say that they can hardly bear the weight and touch of the duvet.
Often the pain is only diminished by the diabetic polyneuropathy. Then stay small injuries often go unnoticed, Because in diabetes in many cases, the circulation is disturbed, so can badly healing wounds arise. This usually happens on the feet (diabetic foot syndrome). The affected tissue can even die off (necrosis). Most diabetics are affected by polyneuropathy on both feet or legs.
In the further course, the polyneuropathy can also spread to autonomous nerves. Possible consequences are for example dysphagia, Vomit and alternating diarrhea and constipation, Also urinary incontinence and Erectile Dysfunction (Men) may turn out to be symptoms of polyneuropathy.
Alcoholic polyneuropathy: symptoms
Also widely used is alcoholic polyneuropathy. It usually progresses slowly. Most sufferers have Nervous disorders on the legsand in both (symmetrical polyneuropathy): There are, for example, pain, abnormal sensation, sensory disturbances, muscle wasting and severe muscle weaknesses (paresis). For example, those affected can no longer stand properly.
In severe cases, polyneuropathy symptoms develop in the eye area, for example pupillary disorders and Paralysis of the eye muscles
In some cases, alcoholic polyneuropathy may be symptomatic.
Polyneuropathy: causes and risk factors
Doctors now know more than 200 different polyneuropathy causes. Most commonly, nerve damage is caused by the diabetes (Diabetic polyneuropathy) or by alcohol (Alcoholic polyneuropathy) triggered.
Polyneuropathy in diabetes
Diabetic polyneuropathy is the most common form of polyneuropathy. It can occur in both type 1 and type 2 diabetes.
An estimated one in two diabetics develops polyneuropathy during their lifetime. The decisive factor is whether and how well the diabetes is treated: Diabetics, whose blood sugar levels are poorly adjusted, namely, especially at an early stage and especially hard to get a polyneuropathy.
By what mechanisms a permanently elevated blood sugar damages the nerves, is not yet clarified in detail.
- On the one hand, many blood sugars can directly damage the nerves: Experts suggest that the sugar molecules form reactive compounds with various proteins (proteins). These attack the nerve cells and irreversibly damage them over time.
- On the other hand, many blood sugars damage the tiny blood vessels in the body (microangiopathy). This can result in nerves no longer being adequately supplied with oxygen and nutrients. This suffers their function. Over time, the underserved nerves can even die.
This nerve damage is usually insidious in diabetic patients. The symptoms of polyneuropathy are therefore slowly starting to appear. Nerve damage also varies with each patient. The type and severity of the symptoms can therefore vary considerably.
Polyneuropathy due to alcohol
The second most common cause of polyneuropathy is alcohol, chronic alcohol abuse. Again, the exact mechanisms that lead to the nerve damage, are not yet fully understood. Research suggests, however, that alcohol can directly attack the nerves. This mechanism is considered to be the main cause of nerve damage in alcoholics.
To make matters worse, a second factor may be added: Alcoholism is often associated with malnutrition. Many alcoholics feed poorly and one-sidedly. This can lead to a lack of vitamin B12. This vitamin is very important for the function of the nervous system. A vitamin B12 deficiency could thus additionally favor nerve disorders in alcoholics. Even if taken alone, it can trigger a polyneuropathy.
Other polyneuropathy causes
Other possible causes of polyneuropathy include:
- Vitamin B12 deficiency (in vegans or after stomach surgery)
- kidney disease
- liver disease
- Disorders of thyroid function (under- and overfunction)
- gout
- Poisons (like arsenic, lead) and medicines (especially cancer medicines)
- some infections with bacteria or viruses (Lyme disease, diphtheria, glandular fever, shingles, herpes simplex infections, HIV etc.)
- Guillain-Barré syndrome (an autoimmune disease)
- Cancer (polyneuropathy may be the first sign here)
Most polyneuropathies are triggered by such diseases or intoxications. Rarer is a nerve damage genetically conditioned, So there are several congenital diseases that are accompanied by a polyneuropathy. These include, for example, the HMSN (hereditary motor-sensitive neuropathy), of which there are several subforms.
In about 20 percent of all patients remains the Cause of polyneuropathy unexplained.
If nerve agents such as alcohol, heavy metals or drugs damage the nerves, it is a “toxic polyneuropathy”.
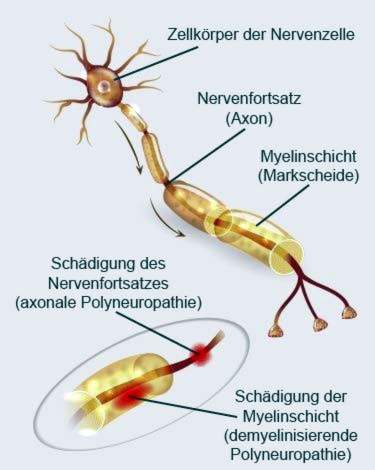
Which part of the nerve cells is damaged?
Each nerve cell is composed of a cell body and a nerve process (axon). The axon can be up to a meter long. You can imagine the nerve processes like cables. The body protects its “nerve cables” with an insulating layer called the myelin sheath or medullary sheath, which, in addition to its protective function, has another function: it accelerates the transmission of the electrical nervous signals.
Depending on which part of a nerve cell is damaged, a distinction is made between demyelinating and axonal polyneuropathy:
The demyelinating polyneuropathy is characterized by the decay of the protective medulla layer (myelin layer). If the axon itself is affected, it is a axonal polyneuropathy, Shapes can also be combined. Then, sheathes and axons are equally damaged.
Polyneuropathy: examinations and diagnosis
If you notice any polyneuropathy symptoms, you should see a doctor immediately. If the nerve damage is detected early and its cause treated, this has a positive effect on the polyneuropathy course.
Doctor-patient conversation
The doctor will first talk to you in detail to make your medical history (anamnesis). He describes the symptoms in detail and asks how long they have lasted. He also inquires about possible pre- or underlying diseases (such as diabetes, kidney disease, hypofunction of the thyroid, etc.). Also tell the doctor about any medications they use and any toxins they may be exposed to in the workplace.
Important information for the clarification of polyneuropathy are also information on drug and alcohol consumption. If you have any questions, you should answer your doctor frankly and honestly. Only then can he find the right cause for the nerve disorders.
Examinations and tests
Following the conversation, the doctor will physically examine you. For example, the doctor tests your reflexes (such as the Achilles tendon reflex). He also checks if your pupils respond properly to incident light. Also on possible malformations of the skeleton (deformities) pays attention of the doctor. For example, claw toes and hollow foot may be an indication that the polyneuropathy is hereditary.
In addition, further investigations follow. Some of these are performed on each patient, others only in certain cases:
In the Electro-neurography (ENG) the nerve conduction velocity is measured. The doctor uses a small electronic impulse in at least two different parts of the nerve. Then he measures the time to reaction (contraction) of the associated muscle. In polyneuropathy this nerve conduction velocity is usually reduced.
In the Electromyography (EMG) the electrical muscle activity is checked. In motor disorders such as muscle weakness or muscle paralysis can thus find out whether the problem is the muscle itself or in the supplying him nerves. If the EMG shows that the nerve function is disturbed, this indicates a polyneuropathy.
In the quantitative sensory examination The doctor will check how a nerve reacts to certain stimuli such as pressure or temperature. This can be used to determine whether the sensitivity of the nerve is impaired – as in polyneuropathy. In this way a nerve damage can be detected well. The investigation is very time consuming. In addition, the patient has to concentrate and cooperate well. Therefore, the method is not routinely used to clarify a polyneuropathy.
A Electrocardiography (ECG) can give information about whether the autonomic nerve fibers of the heart are damaged.
through Ultrasound examination of the bladder The doctor can determine whether residual urine is still in the bladder after urination. If so, bladder emptying is probably disturbed. This happens very often in autonomous polyneuropathy.
At a nerve biopsy A tiny sample of the nerve tissue is taken through a small skin incision. The tissue sample is then examined diagnostically under the microscope. However, this investigation is only carried out in very specific cases. It may be necessary, for example, in diabetics in which only nerves on one side of the body are damaged (asymmetric diabetic polyneuropathy). Even if the doctor suspects leprosy as a cause of nerve damage, he can perform a nerve biopsy.
Also only in selected cases becomes one skin biopsy carried out. A tiny piece of skin is punched out (for example on the lower leg) and examined in detail.
blood tests Above all, they serve to detect common and treatable causes of nerve damage. Rarer causes can also be detected on the basis of certain laboratory values if suspected. Some examples of laboratory tests for polyneuropathy:
- Elevated levels of inflammation (such as CRP, white blood cells, etc.) may indicate an inflammatory cause of nerve damage.
- An oral glucose tolerance test (oGTT) indicates how well the body can process sugar. Conspicuous test results may indicate undetected diabetes (or a precursor to it). Also, the fasting blood sugar is very meaningful.
- In the case of a known diabetes mellitus, the HbA1c value (“long-term blood sugar”) is particularly important: it indicates how well the diabetes has been adjusted in recent months.
- The vitamin B12 status is measured to see if there is a deficiency.
- If the liver or kidney values are out of the norm, polyneuropathy may be caused by liver or kidney disease. Liver damage can also be caused by alcohol abuse.
- If it is suspected that a particular infectious disease causes polyneuropathy, special blood tests are useful. For example, a suspected Lyme disease can be clarified by searching for antibodies to Borrelia in the patient’s blood.
A genetic examination is indicated if there are multiple cases of polyneuropathy in a family. Then it is suspected that it is a hereditary nerve damage.
The same applies if the patient has certain misalignments of the foot (claw toe, hollow foot) or other skeletal abnormalities (such as scoliosis). They are typical of a hereditary polyneuropathy. The doctor can then have the genetic material of the patient examined for corresponding changes (mutations).
Polyneuropathy: treatment
Effective polyneuropathy therapy involves eliminating or treating the cause of the condition, if possible. This is called one causal or causal therapy, For example, alcoholics should make a withdrawal. In diabetic patients, blood sugar needs to be taut. If a vitamin B12 deficiency has been found, one should eat a more balanced diet and balance the deficiency with a vitamin supplement. If toxins or drugs are the cause of polyneuropathy, they must be avoided as much as possible.
Many polyneuropathy symptoms can also be treated specifically. These symptomatic therapy can supplement a causal therapy, if such is possible. For example, the following therapeutic measures are used:
pain Management
In many polyneuropathy patients, nerve damage causes burning pain. These can be alleviated with a pain therapy. Often the doctor recommends Painkiller like ASA (acetylsalicylic acid) or paracetamol. He will select an individually appropriate dosage for each patient.
For very severe nerve pain, he may also called so opioids prescribe. These are very strong painkillers, but they have two drawbacks: firstly, their effects may decrease over time. To relieve the pain, then ever higher dosages are needed. On the other hand, opioids can make you dependent. Your application must therefore be carefully monitored by the doctor.
For very persistent polyneuropathy pain, it may be useful for the patient to be treated by a pain therapist. This specializes in the treatment of chronic pain.
In case of nerve pain can too anticonvulsants (antiepileptics) help, for example gabapentin or pregabalin. They ensure that the nerve cells are less excitable. The pain in the nerves subsides. The therapy with cramps is “crept in”, that is: It starts with a low dose, which is then slowly increased to the desired effect. This prevents side effects. In addition, the doctor will regularly examine the patient’s blood during treatment. Because antiepileptic drugs can alter certain blood levels.
In the context of pain therapy often come too mood-enhancing agents (antidepressants) such as amitriptyline used. They inhibit the transmission of pain signals in the spinal cord. The pain will not be taken away from the patient, but they will be bearable. As with the antispasmodic agents, it is also recommended to “sneak in” the therapy with antidepressants (initially low dose, then incremental dose). This reduces the risk of side effects such as low blood pressure, cardiac arrhythmias or urinary problems.
Some polyneuropathy patients with nerve pain benefit from the so-called TENS (Transcutaneous electrical nerve stimulation), also called stimulation current therapy. An electrode is placed on the painful skin region. It is connected to a small portable device. If required, the patient can deliver gentle electrical impulses via the electrode into the skin area at the touch of a button. That can dampen the pain.
How that is possible, you do not know exactly. But there are different theories. For example, some experts suspect that the electrical impulses release the body’s own pain-relieving messengers (endorphins).
The effectiveness of TENS on nerve pain has not been scientifically proven.
Physical therapy
Especially with sensitive and motor disorders of a polyneuropathy physical therapies can help. These include, for example, physiotherapy, alternating baths, electrical treatment of paralyzed muscles as well as warm and cold wraps. Among other things, these procedures can increase blood circulation and strengthen weakened muscles. In addition, physical therapy helps keep polyneuropathy patients mobile despite pain and other disabling conditions.
Further therapy measures
Depending on the nature and extent of the symptoms, further therapeutic measures may be considered. Some examples:
With frequent calf cramps Polyneuropathy patients can try taking magnesium. Maybe the active ingredient quinine also helps.
Do polyneuropathy patients have big Problems when walking, orthopedic aids are useful. If, for example, the so-called peroneus nerve in the leg is damaged, the affected person can barely lift the foot or not at all. Then a special rail or a special shoe / boot helps.
Resolves polyneuropathy Bloating, nausea and vomiting Patients should change their eating habits: better than a few large meals are then few small meals that are consumed throughout the day. In addition, nausea and vomiting can be relieved with prescription drugs (metoclopramide or domperidone).
at constipation Patients should drink a lot, eat high-fiber foods and exercise regularly. Against acute diarrhea In polyneuropathy, the doctor may prescribe a drug (such as loperamide).
Autonomic disorders in polyneuropathies are, for example Circulatory problems when getting up Lying or Sitting (Orthostatic Hypotension): Those affected become dizzy with a sudden fall in blood pressure, or even faint. As a precaution, patients should always get up slowly. In addition, support stockings can help: They prevent the blood sagging when getting up in the legs and thus trigger the circulatory problems. Regular muscle training is also useful. If necessary, the doctor can also prescribe medication for low blood pressure.
If polyneuropathy a incontinence Patients should go to the bathroom regularly (for example, every three hours) – even if there is no urgency. Then too much residual urine can not accumulate in the bladder. That favors a bladder infection.
A impotence (Erectile dysfunction) can be caused by the polyneuropathy itself as well as medications such as antidepressants. In the second case, patients should discuss with the doctor whether the medications may be discontinued. If this is not possible or the impotence persists after that, affected men can use a vacuum pump. Maybe the doctor can also prescribe a sexual enhancer (Sildenafil etc.).
Polyneuropathy: course and prognosis
The polyneuropathy course can be positively influenced by eliminating or treating the trigger (if possible). Various therapies can also alleviate the symptoms. Nevertheless, many patients are asking themselves: is polyneuropathy curable?
Basically, the earlier the nerve damage is detected and treated, the better the prognosis. Unfortunately, polyneuropathy is often symptomless for a long time or the first mild symptoms are not taken seriously. At the time of diagnosis, the disease is already well advanced. Often then there are already irreversible (irreversible) nerve damage due to the polyneuropathy. Healing is then no longer completely possible. With the right treatment, however, attempts are made to further nerve damage by the polyneuropathy prevent and improve existing symptoms.
Additional information:
Books:
- This is how you treat polyneuropathy – holistically and effectively: The first easy-to-understand guide for those affected (Sigrid Nesterenko, Rainer Bloch, 2017)
- Polyneuropathy: how to overcome agonizing nerve pain (Udo Zifko, 2017, Springer)
- Guide to Polyneuropathy and Restless Legs: Living with numb feet, aching and restless legs (Christian Schmincke, 2017, Springer)
guidelines:
- Guideline “Diagnosis of Polyneuropathies” of the German Society of Neurology (as of 2012)