A herniated disc (disc prolapse, disc prolapse) is most common in people between 30 and 50 years of age. He often causes no complaints. But it can also cause strong back pain, emotional disorders and even paralysis – then fast action is important. Read all about symptoms, examinations and therapy of the herniated disc!

Herniated disc: short overview
- Possible symptoms: depending on the level and extent of the event, e.g. Back pain, which may radiate into a leg or arm, sensory disturbances (ants running, tingling, numbness) or paralysis in that leg or arm, bladder and bowel movements
- Causes: usually age-related and stress-related wear and tear, as well as lack of exercise and obesity; Infrequent injuries, congenital malpositions of the spine or congenital connective tissue weakness
- Important investigations: Physical and neurological examination, computed tomography (CT), magnetic resonance imaging (MRI), electromyography (EMG), electroneurography (ENG), laboratory tests
- Treatment options: Conservative measures (such as mild to moderate exercise, sports, relaxation exercises, heat treatments, medications), surgery
- Forecast: Symptoms usually disappear by themselves or with the help of conservative therapy; Surgery not always successful, complications and relapses possible
Herniated disc: symptoms
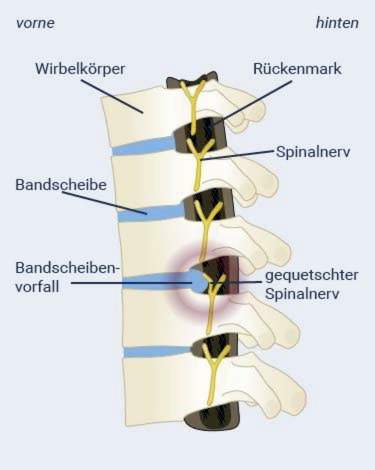
In some patients, a herniated disc causes symptoms such as pain, a tingling sensation or ants running in arms or legs, numbness or even paralysis in the extremities. Reason for the discomfort is that the inner core of the intervertebral disc emerges and presses on nerves on the spinal canal.

Symptoms do not always occur
Not every herniated disc causes symptoms like pain or paralysis. It is then often discovered by accident only as part of an investigation.
If a herniated disc causes symptoms, this indicates that the slipped disc is pressing against individual nerve roots, the spinal cord or the nerve fiber bundle in the lumbar spine (cauda equina = horse tail).
Herniated disc symptoms when pressure on nerve roots
Which herniated disc symptoms occur when pressure is applied to a nerve root depends on the height of the affected nerve root – in the area of the lumbar, thoracic or cervical spine.
Herniated Disc – Lumbar Spine:
Symptoms of a herniated disc are almost always from the lumbar spine, because the body weight here exerts a particularly strong pressure on the vertebrae and intervertebral discs. Physicians speak of lumbar disc herniation or “herniated disc LWS”. Symptoms usually occur due to herniated discs between the 4th and 5th lumbar vertebra (L4 / L5) or between the 5th lumbar vertebra and the 1st coccyx vertebra (L5 / S1).
The pressure on nerve roots in the lumbar spine sometimes causes severe pain in the lower back, which can radiate into the leg (along the supply area of the nerve root in question). Also, neurological deficits such as sensory disturbances (such as ants, tingling, numbness) and paralysis in this area are possible.
It is particularly unpleasant when the sciatic nerve is affected by the lumbar disc herniation. This is the thickest nerve in the body. It consists of the fourth and fifth nerve roots of the lumbar spine and the two first nerve roots of the sacrum. Patients often describe the pain that occurs when they become trapped as being shooting or electrifying. They run from the buttocks over the back of the thigh down to the foot. The symptoms are often increased by coughing, sneezing or when moving. Physicians call this complaint as sciatica.
Herniated disc – cervical spine:
Occasionally, a disc herniation occurs in the cervical region (cervical disc prolapse or herniated disc HWS). It preferably relates to the disc between the 5th and 6th or the 6th and 7th cervical vertebrae. Doctors use the abbreviation HWK 5/6 or HWK 6/7.
Cervical disc herniation symptoms may be pain radiating to the arm. Also, sensations of sensation (paresthesia) and deficits (muscle paralysis) in the area of spread of the affected nerve root are possible symptoms.
Herniated disc – thoracic spine:
At the thoracic spine, a herniated disc is extremely rare. The diagnosis here is “thoracic herniated disc” (or in short: “herniated disc BWS”). Symptoms can be back pain, which is usually limited to the affected spine segment. Only rarely does the pain radiate into the supply area of the compressed nerve.
Herniated disc symptoms with pressure on the spinal cord
The spinal cord extends from the brainstem to the first or second lumbar vertebrae. If a disc herniation presses on the spinal cord, intense pain in one leg or arm as well as emotional disturbances (ants running, tingling sensation, deafness) can occur. Also, an increasing weakness of both arms and / or legs are possible consequences of a herniated disc. Signs that the herniated disc is pressing on the spinal cord may also be dysfunctional of the bladder and bowel. They are accompanied by deafness in the anal and genital area and are considered an emergency – the patient must go to the hospital immediately!
Herniated disc symptoms on pressure on the horse tail
The spinal cord continues at the lower end in a nerve fiber bundle, the horse tail (Cauda equina). It extends to the sacrum, an extension of the spine.
Pressure against the horse’s tail (Caudasyndrom) can cause disturbances at urination and defecation. In addition, those affected no longer have any feeling in the area of the anus and genitals, as well as on the inner thighs. Sometimes even the legs are paralyzed. With such symptoms, one must also immediately go to the hospital!
Suspected herniated disc symptoms
Herniated discs do not always trigger symptoms like back pain – even if the X-ray shows an incident. Sometimes, tension, spinal changes (such as wear, inflammation) or neurological disorders are the cause of suspected herniated disc symptoms. Even pain in the leg is not a clear sign – herniated disc with pressure on a nerve root is just one of several possible explanations. Sometimes there is a blockage of the joint between the sacrum and the pelvis (sacral joint blockade) behind it. Most leg pain can not be associated with any nerve root in back problems.
Herniated disc: examinations and diagnosis
In case of unclear back pain you should first go to the family doctor. If a herniated disc is suspected, he can refer you to a specialist. This can be a neurologist, neurosurgeon or orthopedist.
In order to determine a herniated disc, it is usually sufficient to have a questionnaire of the patient (anamnesis) as well as a thorough physical and neurological examination. Only in certain cases are imaging techniques (such as MRI) necessary.
Doctor-patient conversation
To clarify the suspicion of a herniated disc, the doctor will first raise his medical history in conversation with the patient (anamnesis). He asks, for example:
- What complaints do you have? Where exactly do they occur?
- Since when are the complaints and what has triggered them?
- Does the pain increase when you cough, sneeze or move, for example?
- Do you have problems urinating or defecating?
The information helps the physician to narrow down the cause of the condition and to estimate from which point of the spine they may originate.
Physical and neurological examination
The next step is followed by physical and neurological examinations. The doctor performs palpation, tapping and pressure checks on the spine and back muscles to detect abnormalities or pain points. He also tests the range of motion of the spine. In addition, muscle strength, feeling in the affected arms or legs as well as the reflexes are checked. The nature and localization of the symptoms often give the doctor an indication as to what height of the spine there is a herniated disc.
Imaging procedures
Computed tomography (CT) and magnetic resonance imaging (MRI) can visualize a herniated disc. The doctor then recognizes, for example, the extent of the incident and in which direction it occurred: In most cases, it is mediolateral herniated disc in front. Here, the leaked gelatinous core has slipped between the inter-vertebral and spinal canal.
One lateral herniated disc can be seen from the fact that the gelatinous core has slipped sideways and exits into the intervertebral holes. If he presses on the nerve root of the page concerned, unilateral complaints.
Rarer is one medial herniated disc before: The gelatinous mass of the nucleus nucleus occurs here in the middle backwards in the direction of the spinal canal (spinal canal) and can press directly on the spinal cord.
When are imaging procedures necessary for herniated discs?
CT or MRI is only necessary if consultation with the doctor or physical examination has indicated evidence of a clinically significant herniated disc. This is the case, for example, when paralysis occurs in one leg or both legs, the bladder or bowel function is disturbed, or persistent severe discomfort persists despite weeks of treatment. MRI is usually the first choice.
Imaging is also required when back pain is accompanied by symptoms suggestive of a possible tumor (fever, night sweats or weight loss). In these rare cases, a representation of the space between the spinal cord and the spinal cord (dural space) with an X-ray contrast agent is necessary (myelography or myelo-CT).
A normal X-ray examination is usually not useful if a herniated disc is suspected because it can show only bone but not soft tissue structures such as intervertebral discs and nerve tissue.
Imaging techniques are not always helpful
Even if a disc prolapse is detected on MRI or CT, it does not have to be the cause of the discomfort caused by the patient’s visit to the doctor. In many cases, a herniated disc is without symptoms (asymptomatic).
In addition, imaging techniques can help make the patient’s pain chronic. Because looking at a picture of one’s own backbone can obviously have a negative psychological effect, as studies show. Therefore, especially with diffuse back pain without neurological symptoms (such as sensory disturbances or paralysis) one should first wait and see. Only if the symptoms do not improve after six to eight weeks, an imaging examination is indicated.

Measurement of muscle and nerve activity
If a paralysis or a feeling disorder occurs in the arms or legs and it is unclear whether this is the direct result of a herniated disc, electromyography (EMG) or electroneurography (ENG) can provide certainty. With the EMG, the attending physician uses a needle to measure the electrical activity of individual muscles. In cases of doubt, the ENG can reveal which nerve roots are squeezed by the herniated disc, or if there is another nerve disease, such as polyneuropathy.
laboratory tests
In rare cases, certain infectious diseases such as Lyme disease or herpes zoster (shingles) can cause similar symptoms as a herniated disc. Therefore, if the imaging does not show a finding, the doctor may take a blood sample from the patient and possibly also a sample of cerebrospinal fluid (cerebrospinal fluid). These samples are tested in the laboratory for infectious agents such as Borrelia or herpes zoster viruses.
The doctor may also initiate the determination of general parameters in the blood. These include inflammatory findings such as the number of leukocytes and the C-reactive protein (CRP). These are important, for example, if the symptoms could also be due to inflammation of the intervertebral disc and adjacent vertebral bodies (spondylodiscitis).
Herniated disc: treatment
Most patients are particularly interested in: “What to do if herniated disc?”. The answer depends mainly on the symptoms. In more than 90 percent of patients a conservative herniated disc treatment is sufficient, ie therapy without surgery. This is especially true when the herniated disc causes pain or mild muscle weakness, but no other / more serious symptoms.
These include above all paralyzes and disorders of the bladder or rectum function. In such cases, surgery is usually performed. Even with persistent symptoms despite conservative treatment for at least three months, surgery can be considered.
Herniated disc: treatment without surgery
As part of the conservative herniated disc treatment, the doctor recommends today only rarely immobilized or bed rest, But it may be necessary, for example, in a cervical disc prolapse immobilization of the cervical spine by means of neck brace. In case of severe pain due to lumbar disc herniation, a step bed support can be helpful in the short term.
In most cases, conservative herniated disc therapy includes slight to moderate movement, Normal everyday activities are – as far as the pain allow – so quite advisable. Many patients also receive physiotherapy as part of an outpatient or inpatient rehabilitation. The therapist exercises with the patient, for example, low-pain movement patterns and gives tips for activities in everyday life.
Regarded in the long term, regular exercise is very important in a herniated disc: On the one hand promotes the change between loading and unloading the intervertebral discs their diet. On the other hand, physical activity strengthens the core muscles, which relieves the intervertebral discs. Therefore, exercises to strengthen the back and abdominal muscles are highly recommended in herniated disc. Physiotherapists can show these exercises to patients as part of a back training program. Subsequently, the patients should train themselves regularly.
In addition, one may and should be with herniated disc Sports if it is disc-friendly. This applies, for example, to aerobics, running, backstroke, cross-country skiing and dancing. Less good for the discs are tennis, downhill skiing, football, handball and volleyball, golf, ice hockey, judo, karate, gymnastics, canoeing, bowling, wrestling, rowing and squash.
If you do not want to do without such a type of sport that is harmful to the lumbar disc, you should do a physical exercise and strength training to compensate, for example, walk, cycle or swim regularly. If in doubt, patients should discuss the nature and extent of physical activity with the doctor or physiotherapist.
Many people with back pain due to a herniated disc (or other reasons) also benefit from relaxation exercises, These can help, for example, to release painful muscle tension.
Have the same effect heat applications, Therefore, they are also often part of the conservative treatment for herniated disc.
If necessary drugs used in herniated disc. These include above all analgesics such as non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac etc.). In addition to an analgesic, they also have an anti-inflammatory and decongestant effect. Other drugs may also be used, such as COX-2 inhibitors and cortisone. They also have anti-inflammatory and analgesic. For very severe pain, the doctor may prescribe opiates in the short term.
The pain therapy for herniated disc should be closely monitored by the doctor to avoid serious side effects. Patients should adhere strictly to the doctor’s instructions when using the painkillers.
In some cases, the doctor will also prescribe muscle-relaxing drugs (muscle relaxants), because the muscles can be painful and a possible restraint tense and harden. Sometimes antidepressants are also useful, for example for severe or chronic pain.

Herniated disc: When should surgery be performed?
Whether a herniated disc operation should be performed, doctor and patient decide together. The criteria for an intervertebral disc surgery are:
- Symptoms of pressure against the spinal cord (early or immediate surgery)
- severe paralysis or increasing paralysis (immediate surgery)
- Symptoms suggesting pressure against the horse’s tail (Cauda equina) (immediate operation)
- decreasing pain and increased paralysis (rapid surgery because of the risk of the nerve roots already dying)
There are several techniques for surgical treatment of herniated disc. Today, microsurgical procedures are standard. They reduce the risk of scarring. Alternatively, in some cases, minimally invasive procedures may be considered in a herniated disc surgery.
Herniated disc surgery: Microsurgical discectomy
The most common technique in surgical herniated disc treatment is microsurgical discectomy (disc = disc, ectomy = removal). The affected disc is removed using a surgical microscope and the smallest special instruments. This should relieve those spinal nerves (spinal nerves), which are narrowed by the herniated disc and cause discomfort.
For the introduction of surgical instruments only small skin incisions are needed. This is why microsurgical surgical technique is one of the minimally invasive procedures.
Due to microsurgical discectomy, all herniated discs can be removed – regardless of which direction the disc part has slipped. In addition, the surgeon sees directly whether the troubled spinal nerve has been released from any pressure.
Expiration of the operation
The microsurgical discectomy is performed under general anesthesia. The patient is in a kneeling position with the upper body at a higher level on the operating table. This increases the distance between the vertebral arches and facilitates the opening of the spinal canal.
At the beginning, the surgeon makes a small incision over the diseased area of the disc. Then he pushes the back muscles carefully to the side and cuts the yellow band (ligamentum flavum), which connects the vertebral bodies, partially (as little as necessary). So the surgeon can see with the microscope directly into the spinal canal. Sometimes he also needs to remove a small piece of bone from the vertebral arch to improve vision.
With special instruments, he now loosens the protruding disc tissue under visual control of the spinal nerve and removes it with a forceps. Larger defects in the fibrous ring of the intervertebral disc can be sutured microsurgically. Also in the spinal canal slipped disc parts (sequester) can be removed. In the last step of the intervertebral disk operation, the surgeon closes the skin with a few stitches.
Possible complications
In microsurgical disc surgery, the nerve to be relieved may be injured. Possible consequences are emotional and motor disorders of the legs, disorders of the bladder and bowel and sexual disorders. Such complications are rare.
As with any surgery, this disc surgery also poses a certain risk of anesthesia and the risk of infection, wound healing and rebleeding.
Some of the patients feel again pulling pain or, for example, a tingling sensation after weeks to months, even with optimal intervertebral disc surgery and removal of the eventualities. This late succession is called “failed back surgery syndrome”.
After the operation
As with any surgery under anesthesia, sometimes the bladder needs to be emptied with a catheter on the first day after surgery. After a short time normalize but the bladder and bowel function. Mostly, the patient can get up on the evening of the day of surgery.
On the first day after the procedure, physiotherapy exercises are started on the herniated disc patient. This is supposed to strengthen his muscular and ligamentous apparatus. Psychologists, dietitians and occupational therapists also work as specialists in rehabilitation after a herniated disc surgery.
The hospital stay usually takes only a few days. Six or twelve months after microsurgical discectomy, the long-term success of the disc surgery is reviewed. This is helped by imaging techniques.
Herniated Disc Operation: Open Discectomy
Before the surgical microscope was introduced, herniated discs were often operated on with the conventional open technique with a larger access (larger incisions). Today, the open discectomy is rarely performed, such as malformations of the spine. Their results are comparable to those of microsurgical discectomy. However, serious complications are more common.
Expiration of the operation
The open discectomy is essentially the same as the microsurgical hernia, but larger incisions are made and the surgical field is not assessed with a micro-optic, but from the outside.
Possible complications
The potential complications of open discectomy are similar to those of microsurgical discectomy, but more common.
After the operation
Sometimes, on the first day after open disc surgery, the bladder must be emptied using a catheter. Within a very short time, however, the bladder and bowel function normalize again.
The patient is usually allowed to get up again on the evening of the surgery day. The next day is usually started with physiotherapy exercises to strengthen the muscular and ligamentous apparatus of the back again. The patient usually only has to stay in hospital for a few days.
Herniated Disc Operation: Endoscopic Discectomy
In addition to the microsurgical method, the minimally invasive techniques of intervertebral disk surgery include so-called percutaneous endoscopic methods. The disc is removed using endoscopes, video systems and micro-instruments (partly motor-driven), which are inserted via small skin incisions. The patient is usually in a semi-awake state and under local anesthesia. Thus, he can communicate with the surgeon.
The endoscopic herniated disc surgery can not be performed on every patient. It is for example unsuitable if parts of the intervertebral disc have detached (sequestrated herniated disc) and have slid up or down in the vertebral canal. Endoscopic discectomy is also not always applicable to herniated discs in the transition region between the lumbar spine and the sacrum. Because here the iliac crest blocks the way for the instruments.
By the way: With endoscopic methods, not only the entire disc can be removed (discectomy), but possibly also only parts of the nucleus. Then one speaks of percutaneous endoscopic nucleotomy.
Expiration of the operation
The patient is lying on his stomach during the endoscopic disc surgery. The skin over the affected spinal column section is disinfected and locally anesthetized. Over one or two small incisions, one to two small metal tubes are advanced into the disc space under X-ray control. These are working sleeves with a diameter of three to eight millimeters. They allow instruments such as small forceps and an endoscope to be inserted into the disc space. The latter has a special lighting and optics. The images from the operating area inside the body are projected onto a video monitor where the operating doctor can see them.
The surgeon can now selectively remove disc tissue that presses on a nerve. After the endoscopic disc operation, he sutures the incisions with one or two stitches or supplies them with special patches.
Possible complications
The complication rate is relatively low in endoscopic disc surgery. Nevertheless, there is a certain risk of injuring nerves. Possible consequences are feeling and movement disorders in the legs as well as functional disturbances of bladder and intestine.
In addition, as with any surgery, there is a risk of infection, wound healing disorders and rebleeding.
Compared to microsurgical discectomy, the rate of recurrence (recurrence rate) in endoscopic disc surgery is higher.
After the operation
If the endoscopic intervertebral disc surgery has no complications, the patient can get up within three hours and leave the hospital on the same day or the next morning. Physiotherapy should be started the day after the operation.
Disc surgery with intact fibrous ring
If someone has only a slight disc herniation, with the fiber ring still intact, the affected disc in the area of the nucleus can sometimes be minimized or shrunk by a minimally invasive procedure. This relieves the pressure on nerve roots or spinal cord. This technique is also useful for disc protrusions (here the fiber ring is always intact).
The advantage of minimally invasive procedures is that they only require small skin incisions, are less risky than open surgery and can usually be performed on an outpatient basis. However, they are only suitable for a small number of patients.
Expiration of the operation
In this minimally invasive disc operation, the skin is first disinfected and locally anesthetized over the affected spinal column. Sometimes the patient is also put into a drowsy sleep. Now the doctor under image control carefully pricks a hollow needle (cannula) into the middle of the affected intervertebral disc. Through the hollow channel he can introduce working tools to shrink or shrink the tissue of the gelatinous core:
That can be about one laser be that evaporates the gelatinous nucleus inside the intervertebral disc by individual flashes of light (Laserdiskusdekompression). The jelly core consists of over 90 percent water. By vaporizing tissue, the volume of the core is reduced. In addition, the heat destroys “pain receptors” (nociceptors).
In the thermolesion the surgeon pushes one Thermo catheter under X-ray control to the inside of the disc before. The catheter is heated up to 90 degrees Celsius, so that a part of the disc tissue overcooked. At the same time, the outer fiber ring should solidify due to the heat. Even a part of the pain-conducting nerves is destroyed.
In the so-called Nucleoplasty the doctor uses radio frequenciesto generate heat and vaporize the tissue.
The doctor can also do one decompressor insert it into the intervertebral disc via the cannula. At the top sits a rapidly rotating spiral thread. It cuts into the tissue and at the same time it can suck out up to one gram of gelatinous mass.
In thechemonucleolysis The enzyme chymopapain is injected, which chemically liquefies the gelatinous core inside the intervertebral disc. After a certain waiting time, the liquefied core mass is sucked off via the cannula. It is very important here that the fiber ring of the affected disc is completely intact. Otherwise, the aggressive enzyme may leak out and cause severe damage to surrounding tissue (such as nerve tissue).
Possible complications
Possible complications of minimally invasive disc surgery include bacterial disc disease (spondylodiscitis). It can spread to the entire vertebral body. Therefore, the patient usually gets a preventive antibiotic.
After the operation
In the first few weeks after a minimally invasive intervertebral disk operation, the patient should take care of themselves physically. Sometimes the patient is prescribed a corset (elastic bodice) for relief for this period.
Herniated disc surgery: Implants
As part of the surgical herniated disc treatment, the worn disc is sometimes replaced with a prosthesis to preserve the mobility of the spine. The disc implant is designed to maintain the space between the vertebrae as well as their normal mobility and relieve the pain.
So far, it is unclear which patients benefit from an intervertebral disc implant and what the long-term successes look like. Ongoing studies have yielded quite positive results so far. Es fehlen aber noch echte Langzeitergebnisse, zumal die meisten Patienten zum Zeitpunkt der Bandscheiben-Operation im mittleren Lebensalter sind, also vermutlich noch einiges an Lebenszeit vor sich haben.
Nucleus pulposus-Ersatz
Im frühen Stadium des Bandscheibenverschleißes (Bandscheibendegeneration) ist es möglich, nur den Gallertkern der Bandscheibe (Nucleus pulposus) zu ersetzen. Diese Operation wird weltweit in klinischen Studien weiterentwickelt und beobachtet. Der künstliche Gallertkern fungiert als Platzhalter zwischen den Wirbeln und ist mit Hydrogel gefüllt. Dieses Gel kommt den biochemischen und mechanischen Eigenschaften des natürlichen Gallertkerns sehr nahe, weil es Flüssigkeit aufnehmen kann. Wie die Bandscheibe saugt es bei Entlastung Wasser auf und gibt es bei Belastung wieder ab.
Die Bandscheiben-Operation wird unter Vollnarkose durchgeführt. Der Zugang zur Bandscheibe erfolgt entweder über einen Hautschnitt im Rücken oder minimal-invasiv vom Bauch aus. Schon am Tag nach der Operation kann der Betroffene aufstehen. Über Langzeitergebnisse ist bisher wenig bekannt.
Bandscheiben-Totalersatz
Beim Bandscheiben-Totalersatz werden die Bandscheibe und Teile der Grund- und Deckplatten der angrenzenden Wirbel entfernt. Der Bandscheibenersatz besteht bei den meisten Modellen aus titanbeschichteten Grund- und Deckplatten und einem Polyethylen-Inlay (also ganz ähnlich wie die bekannten Hüftprothesen).
Zum Ablauf der Bandscheiben-Operation: Die alte Bandscheibe wird entfernt; zusätzlich wird ein Teil des Knorpels an den Grund- und Deckplatten der angrenzenden Wirbel weggeraspelt. Mithilfe von Röntgendurchleuchtung wird die Bandscheibengröße bestimmt und ein passendes Implantat ausgewählt. In die Grund- und Deckplatte der angrenzenden Wirbel meißelt der Operateur nun je nach Modell einen kleinen, senkrechten Schlitz. Er dient der Verankerung der Prothese. Dann bringt der Chirurg den Bandscheibenersatz ein. Der Druck der Wirbelsäule stabilisiert das Implantat. Innerhalb von drei bis sechs Monaten wächst Knochenmaterial in die speziell beschichteten Grund- und Deckplatten der Bandscheiben-Vollprothese ein.
Schon am ersten Tag nach der Operation kann der Patient aufstehen. In den ersten Wochen darf er keine schweren Lasten heben und muss Extrembewegungen vermeiden. Zur Stabilisierung dient ein elastisches Mieder, das der Patient selbst anlegen kann.
Patienten, die an Osteoporose (Knochenschwund) leiden oder bei denen der zu behandelnde Wirbel bewegungsinstabil ist, dürfen keinen Bandscheiben-Totalersatz bekommen.
Bandscheibenvorfall: Ursachen und Risikofaktoren
Beim Vorfall einer Bandscheibe – dem Stoßdämpfer zwischen zwei Wirbeln – verrutscht der innere Gallertkern der Bandscheibe. Die derbe, faserige Hülle (Anulus fibrosus) der Bandscheibe reißt und der Gallertkern tritt nach außen. Er kann auf die am Rückenmark entspringenden Nerven (Spinalnerven) drücken und so Beschwerden verursachen. Manchmal rutschen auch abgelöste Teile des Gallertkerns in den Wirbelkanal. Dann lautet die Diagnose „sequestrierter Bandscheibenvorfall“.

Die Ursache eines Bandscheibenvorfalls ist meist eine alters- und belastungsbedingte Degeneration des Bindegewebsrings der Bandscheibe: Er verliert seine stabilisierende Funktion und reißt bei großer Belastung ein. Der Gallertkern kann teilweise austreten und dabei auf eine Nervenwurzel oder das Rückenmark drücken. Die Häufigkeit der Bandscheibenvorfälle nimmt ab dem 50. Lebensjahr wieder ab, weil der Bandscheibenkern dann immer mehr an Flüssigkeit verliert und deshalb seltener austritt.
Darüber hinaus sind Bewegungsmangel and Übergewicht wichtige Risikofaktoren für Bandscheibenvorfälle. Typischerweise sind dann zusätzlich die Bauch- und Rückenmuskeln schwach, Eine solche Instabilität des Körpers fördert eine Fehlbelastung der Bandscheiben, da nur eine starke Rumpfmuskulatur die Wirbelsäule entlastet.
Mögliche Auslöser eines Bandscheibenvorfalls sind auch Haltungsfehler, ruckartige Bewegungen such as Sportarten, bei denen die Wirbelsäule erschüttert (Reiten, Mountainbiking) oder in sich verdreht wird (Tennis, Squash). Das Gleiche gilt für schwere körperliche Arbeit, wie das Heben schwerer Lasten. Allerdings kann dies allein keinen Bandscheibenprolaps verursachen. Das kann nur passieren, wenn eine Bandscheibe bereits Abnutzungserscheinungen aufweist.
Seltener sind Verletzungen(etwa durch einen Treppensturz oder Verkehrsunfall) sowie angeborene Fehlstellungen der Wirbelsäule die Ursache eines Bandscheibenvorfalls.
Bei manchen Menschen trägt eine angeborene Schwäche des Bindegewebes zur Entstehung eines Bandscheibenprolaps bei.
Vom Bandscheibenvorfall (Bandscheibenprolaps) zu unterscheiden ist die Bandscheibenvorwölbung (Diskusprotrusion). Hier verlagert sich das innere Bandscheibengewebe nach außen, ohne dass der Anulus der Bandscheibe zerreißt. Trotzdem können Beschwerden wie Schmerzen und Empfindungsstörungen auftreten. Bekanntes Beispiel ist der Hexenschuss (Lumbago): Darunter versteht man akut einschießende, heftige Schmerzen im Lendenwirbelbereich.
Bandscheibenvorfall: HWS
Die altersbedingte Abnutzung von Wirbelgelenken und Bandscheiben ist der Hauptgrund, warum vor allem bei älteren Menschen die Halswirbelsäule einen Bandscheibenvorfall aufweisen kann: Die Wirbelgelenke lockern und verändern sich mit den Jahren, die Bandscheiben zermürben zunehmend.
Die Auswirkungen eines Bandscheibenvorfalls in der Halswirbelsäule betreffen meist Schultern, Arme sowie den Brustbereich, weil die versorgenden Nerven in dieser Höhe das Rückenmark verlassen.
Wenn jüngere Menschen einen Bandscheibenvorfall HWS erleiden, ist die Ursache oft eine Verletzung oder ein Unfall. Zum Beispiel kann eine abrupte Drehbewegung des Kopfes dazu führen, dass eine Bandscheibe zwischen den Halswirbeln vorfällt.
Mehr über Ursachen, Symptome und Behandlung eines zervikalen Bandscheibenprolaps lesen Sie im Beitrag Bandscheibenvorfall HWS.
Bandscheibenvorfall: Krankheitsverlauf und Prognose
Bei etwa 90 von 100 Patienten lassen die Schmerzen und Bewegungseinschränkungen, die ein akuter Bandscheibenvorfall verursacht, innerhalb von sechs Wochen von allein nach. Vermutlich wird das verschobene oder ausgetretene Bandscheibengewebe vom Körperbeseitigt oder verschiebt sich, sodass der Druck auf Nerven oder Rückenmark nachlässt.
Falls eine Behandlung notwendig wird, genügen meist konservative Maßnahmen. Sie sind deshalb vielfach die Therapie der Wahl bei einem Bandscheibenvorfall. Die Dauer der Regeneration und Heilungschancen hängen vom Schweregrad des Bandscheibenvorfalls ab.
Auch nach einer erfolgreichen Behandlung kann es an der gleichen Bandscheibe oder zwischen anderen Wirbelkörpern zu einem neuen Vorfall kommen. Daher sollte jeder nach einem überstandenen Bandscheibenvorfall seine Rumpfmuskulatur regelmäßig trainieren und weitere Ratschläge beherzigen, mit denen sich ein Bandscheibenvorfall vorbeugen lässt (siehe unten).
Nach einer Operation
Eine Operation bei Bandscheibenvorfall sollte sorgfältig überdacht werden. Oftmals verläuft sie zwar erfolgreich, aber es gibt auch immer wieder Patienten, bei denen der Eingriff langfristig nicht die gewünschte Schmerzfreiheit bringt. Mediziner sprechen hier vom Failed-back-surgery-Syndrom oder Postdiskektomie-Syndrom. Es entsteht dadurch, dass der Eingriff die eigentliche Ursache für die Schmerzen nicht beseitigt hat oder aber neue Schmerzursachen geschaffen hat. Das können zum Beispiel Entzündungen und Narbenbildung im Operationsgebiet sein.
Als weitere Komplikation einer Bandscheiben-Operation können Nerven und Gefäße beim EIngriff geschädigt werden.
Aus verschiedenen Gründen kann sich also ein Patient nach einer Bandscheibenoperation unter Umständen schlechter fühlen als vorher. Zudem können Folgeoperationen notwendig werden. Das kann auch der Fall sein, wenn bei operierten Patienten später erneute Bandscheibenvorfälle auftreten.
Ein Bandscheibenvorfall sollte deshalb nur dann operiert werden, wenn es dringend notwendig ist, etwa weil er Lähmungen verursacht. Außerdem sollte der zu erwartende Nutzen deutlich größer sein als die Risiken. Um die Ergebnisse zu verbessern, schließen sich bei vielen Patienten nach der Operation Aufenthalte in Reha-Kliniken an.
Bisher gibt es noch keine Möglichkeit, im Vorfeld sicher herauszufinden, welche Patienten mit Bandscheibenvorfall von einer Bandscheiben-OP am meisten profitieren.
Bandscheibenvorfall: Vorbeugen
Eine gesunde, starke Rumpfmuskulatur ist die Voraussetzung dafür, dass der Körper die alltäglichen Herausforderungen meistern kann. Wenn Sie einige Regeln beachten, können Sie gegen einen Bandscheibenvorfall was tun. Vorbeugende Maßnahmen sind unter anderem:
- Achten Sie auf Ihr Körpergewicht: Übergewicht belastet den Rücken und begünstigt einen Bandscheibenvorfall.
- Treiben Sie regelmäßig Sport: Besonders günstig für den Rücken sind Wandern, Jogging, Skilanglauf, Kraulen und Rückenschwimmen, Tanzen, Wassergymnastik und andere Arten von Gymnastik, welche die Rückenmuskulatur stärken.
- Bestimmte Entspannungstechniken wie Yoga, Tai Chi und Pilates fördern ebenfalls eine gute Körperhaltung und helfen, Rumpf und Rücken zu stärken. Das ist die beste Entlastung für Wirbelsäule und Bandscheiben.
- Sitzen Sie nach Möglichkeit aufrecht und auf einem normal hohen Stuhl. Wechseln sie häufig die Sitzposition. Ein begleitendes Krafttraining stabilisiert die Rumpfmuskulatur.
- Positionieren Sie Gegenstände, die Sie oft verwenden, in einer gut erreichbaren Höhe: Augen und Arme werden entlastet und Sie verhindern, dass Sie die Halswirbelsäule überlasten. Das ist auch bei einem rückenfreundlichen Arbeitsplatz wichtig.
- Meiden Sie tiefe und weiche Sitzmöbel; empfehlenswert ist ein keilförmiges Sitzkissen.
- Arbeiten im Stehen: Der Arbeitsplatz muss so hoch sein, dass Sie (dauerhaft) aufrecht stehen können.
- Heben Sie sehr schwere Gegenstände nie mit gestreckten Beinen und gebeugter Wirbelsäule: Gehen Sie in die Knie, lassen Sie die Wirbelsäule gestreckt und heben die Last “aus den Beinen heraus”.
- Verteilen Sie die Last in beide Hände, damit die Wirbelsäule gleichmäßig belastet wird.
- Winkeln Sie die Wirbelsäule nicht zur Gegenseite hin ab, wenn Sie Lasten tragen.
- Halten Sie die Arme beim Tragen von Lasten dicht am Körper: Verlagern Sie dabei das Gewicht des Körpers nicht nach hinten und vermeiden Sie ein Hohlkreuz.
- Sorgen Sie dafür, dass die Wirbelsäule auch beim Schlafen nicht abknicken kann. Sinnvoll ist eine gute Matratze (die Härte sollte dem Körpergewicht entsprechen) plus Lattenrost sowie eventuell ein kleines Kissen zur Unterstützung der natürlichen Wirbelsäulenform.
An diese Ratschläge sollten sich besonders auch Menschen halten, die bereits einen Bandscheibenvorfall hatten.
Additional information
Bücher
- Bandscheiben-Leiden – Was tun?: Mit den besten Übungen für den Alltag (Paul Th. Oldenkott et al.,2013, Goldmann Verlag)
Leitlinien
- S2k Leitlinie “Konservative und rehabilitative Versorgung bei Bandscheibenvorfällen mit radikulärer Symptomatik” der Deutschen Gesellschaft für Orthopädie und Orthopädische Chirurgie (DGOOC) (Stand:2014)
- S2k-Leitlinie „LumbaleRadikulopathie“ der Deutschen Gesellschaft für Neurologie (Stand: 2012)
- S1-Leitlinie „Zervikale Radikulopathie“ der Deutschen Gesellschaft für Neurologie (Stand: 2012)