Aortic valve stenosis is the most common heart valve defect. The cause is usually an acquired calcification of the aorta, which results from an unhealthy lifestyle. The oxygen-rich blood can then no longer be sufficiently pumped into the large circulation. Symptoms of aortic valve stenosis include a lack of brain supply, dizziness, and lower exercise capacity. Read all important information about aortic valve stenosis here.
Aortic valve stenosis: description
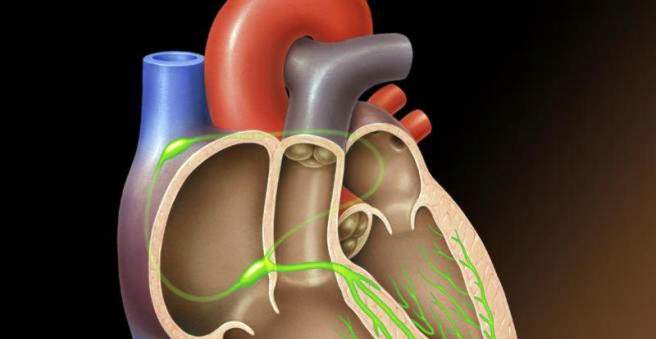
Aortic stenosis is the most common heart valve defect. It is characterized by a hardening and narrowing (stenosis) of the heart valve at the exit of the left ventricle. This aortic valve consists of three crescent-shaped pockets. Their job is to release the oxygenated blood into the aorta and then into the body.
This “exit” from the heart is reduced in the aortic valve stenosis, so that the heart has to muster more strength to pump against it. Nevertheless, not enough oxygen-rich blood gets into the systemic circulation. The human brain needs oxygen most urgently to maintain its functions. Accordingly, it also responds as the first organ to an oxygen deficiency, as it arises as a result of aortic valve stenosis. The lack of oxygen leads to dizziness symptoms after just two to four seconds.
Aortic valve stenosis: symptoms
Those affected complain at the beginning mostly about dizziness and an occasional circulatory collapse (syncope). This is due to the lack of blood flow to the brain due to aortic stenosis. The heart can no longer keep up, especially in situations of physical stress (climbing stairs or even sports): aortic valve stenosis prevents the body’s increased oxygen demand from being covered during physical activity. So comes to a shortage of blood.
To pump against the aortic valve stenosis, the left half of the heart needs more muscle power. Over time, it adapts to it by expanding. The increase in myocardial tissue also increases its oxygen demand. Even if the coronary arteries that supply the heart with blood are healthy, it can lead to a tightness in the chest and chest pain (angina pectoris).
The enlargement of the left ventricle leads to further symptoms. The lack of supply of the heart muscle and its enlargement can lead to symptoms of heart failure (heart failure) or cardiac arrhythmias (for example, atrial fibrillation). Patients suffer from shortness of breath and feel cold-sweat. The blood accumulates from the left ventricle back towards the lungs, which can lead to fluid accumulation in the lungs (pulmonary edema). The performance generally decreases sharply and those affected are very quickly weakened.
Aortic valve stenosis: causes and risk factors
Aortic valve stenosis may be acquired or congenital.
Acquired aortic valve stenosis
Aortic valve stenosis is acquired in most cases, most often through wear processes (calcification) in older age. An unhealthy lifestyle contributes, above all, permanently increased blood lipids (especially cholesterol). It settles in the vessels, often together with lime and collagen. This thickening and hardening of the tissue leads to aortic valve stenosis in the area of the aortic valve. Three to five percent of over 75 year olds have severe aortic stenosis.
Also, rheumatic fever and inflammation of the heart lining (endocarditis) can leave behind a scarred tissue on the aortic valve, causing aortic valve stenosis: scar tissue is less flexible than healthy tissue, and can hinder blood flow from the heart into the aorta.
Symptoms usually occur in the case of acquired aortic valve stenosis only from the age of 60 years.
Congenital aortic valve stenosis
Congenital aortic valve stenosis is much rarer and causes discomfort at a younger age. It can be divided into three forms depending on the location of the constriction:
Most often, the heart valve itself is affected by the narrowing (valvular aortic valve stenosis). If, on the other hand, the area above the aortic valve (the beginning of the aorta) is narrowed, this is called supravalvular aortic valve stenosis. In a subvalvular aortic valve stenosis, the tissue is narrowed below the heart valve.
Aortic valve stenosis: examinations and diagnosis
If aortic valve stenosis is suspected, the doctor performs a physical examination. He measures the patient’s blood pressure and listens to his heart with the stethoscope. In the case of an aortic valve stenosis, a heart murmur can be heard during the ejection phase of the heartbeat. This murmur is usually audible at the level of the carotid arteries, where it appears as a whirring noise. Aortic valve stenosis is best heard with the stethoscope between the second and third ribs on the right breast next to the sternum.
To ensure the diagnosis “Aortenklappenstenose”, usually followed by a diagnostic apparatus:
roentgen
The x-ray of the ribcage reveals any thickening of the left ventricle or the aorta. In a lateral X-ray, even the calcification of the aortic valve can be visualized.
Electrocardiography (ECG)
As a rule, if an aortic valve stenosis is suspected, an ECG is also made to better assess the severity of the constriction. A wall thickening of the left ventricle can be detected.
echocardiography
Echocardiography is an ultrasound of the heart. Hereby one can prove the Aortenklappenstenose very well. The flow velocity at the throat is measured. The flap opening area can also be determined, ie how far the aortic valve opens. The valve opening area is an important diagnostic tool for determining the severity of aortic valve stenosis:
- Slight aortic stenosis: Greater than two square centimeters
- Moderate aortic stenosis: Between 1.1 and two square centimeters
- High grade aortic stenosis: Less than 0.75 square centimeters
Cardiac catheter examination
Aortic valve stenosis can also be examined with the help of a left heart catheter. For this purpose, a thin plastic tube (catheter) is usually introduced into an artery in the groin and advanced over the aorta to the aortic valve.
Aortic valve stenosis: treatment
If it is a mild aortic stenosis without symptoms, a conservative (non-invasive) treatment can be carried out first: the person concerned should avoid physical exertion and be sufficiently gentle.
Moderate to severe aortic valve stenosis usually causes symptoms. In these cases, an operative therapy is recommended.
Aortic valve stenosis: surgery
As operative measures different procedures are used for aortic valve stenosis:
An aortic valve replacement is particularly often used in acquired stenoses.
As part of a cardiac catheterization can also perform a balloon dilatation. A small balloon is inflated at the constricted area to dilate the narrowed area. In congenital aortic stenosis, this procedure shows good results. In acquired aortic valve stenosis, however, balloon dilation has a high relapse rate (recurrence rate).
The Ross operation is mainly performed on congenital aortic valve stenosis in children. The aortic valve is replaced by another heart valve – the pulmonary valve, which sits between the right ventricle and the large pulmonary artery. It in turn is replaced by a graft. This procedure allows the vital aortic valve to grow with you.
Aortic valve stenosis: medication
An additional drug therapy aims at an improvement of the symptoms until surgery. For example, the consequences of aortic valve stenosis – heart failure and cardiac arrhythmias – can be treated with beta-blockers, cardiac glycosides or even diuretics.
Aortic valve stenosis: disease course and prognosis
Untreated aortic stenosis can have serious consequences: Turbulent blood flow to the calcified aortic valve can cause small clots to form. They can be carried along by the bloodstream and get into the brain. If they clog a vessel there and stop the blood supply, it is called a stroke.
Aortic valve stenosis can also cause cardiac arrhythmias. If left untreated, these can lead to ventricular fibrillation and cardiac death.
In surgical treatment of aortic valve stenosis However, the forecast is good.